Copyright
©The Author(s) 2020.
World J Clin Cases. Sep 26, 2020; 8(18): 4100-4108
Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4100
Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4100
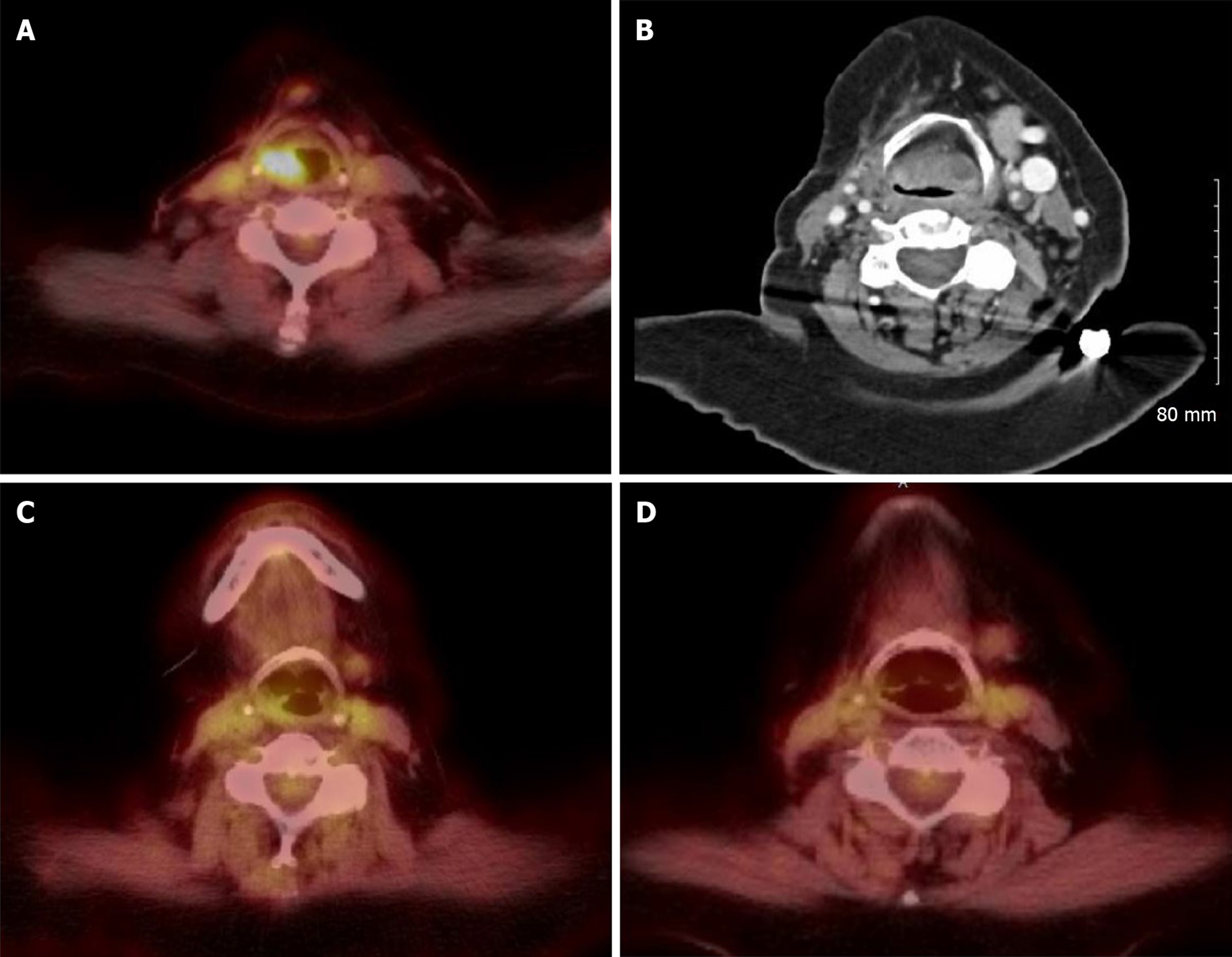
Figure 1 Positron emission tomography/computed tomography fusion images with fluorodeoxyglucose-18 and computed tomography soft tissue of neck.
A: New fluorodeoxyglucose (FDG) avidity and soft tissue fullness in the right supraglottic fold extending to the epiglottis with mild leftward deviation of the trachea with narrowing in September 2018; B: Computed tomography neck soft tissue: considerable supraglottic soft tissue thickening, manifested most in posterior supraglottic larynx which threatens laryngeal airway in January 2019; C: Resolving right supraglottic soft tissue fullness and FDG activity 4 d after first dose of infliximab in March 2019; D: Improvement of right supraglottic soft tissue fullness and FDG activity in June 2019.
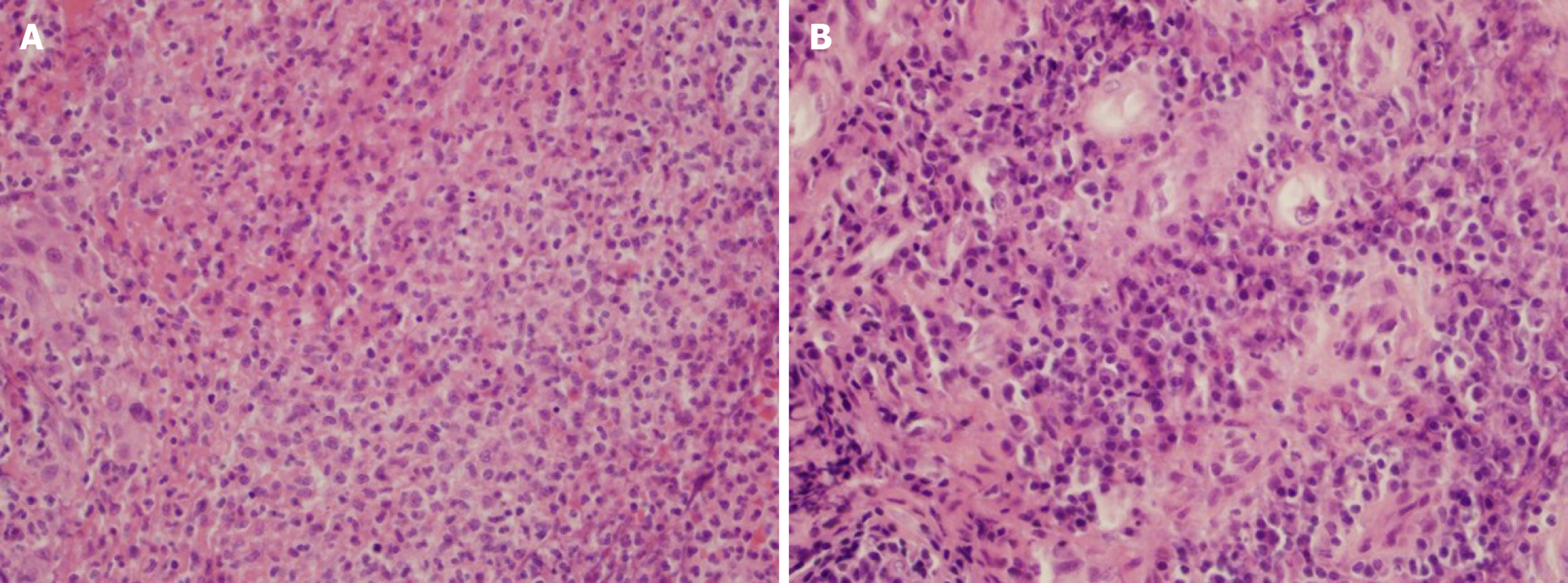
Figure 2 HE stain of larynx biopsy results.
A: Larynx, right arytenoid tissue: Fibrinopurulent exudation; B: Larynx, left false vocal cord: Granulation tissue. HE stain of larynx biopsy (× 400).
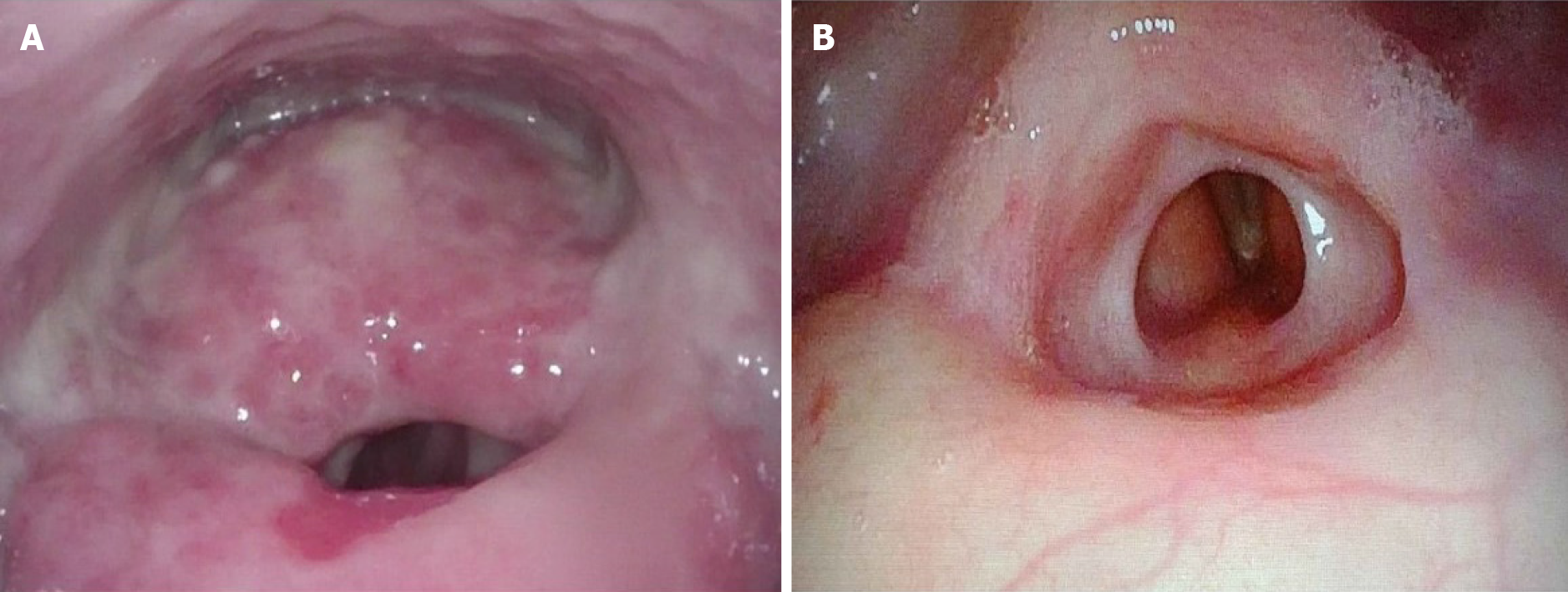
Figure 3 Direct laryngoscopy.
A: January 2019, before infliximab treatment: Massive swelling of posterior supraglottic larynx obliterating normal posterior supraglottic landmarks and diffuse inflamed granular mucosa with weeping character involving nearly all of supraglottic larynx and much of lower pharynx. Supraglottic mass encroaches over posterior supraglottic laryngeal airway. True vocal cords remain clear and mobile; B: May 2019, after infliximab treatment: Resolution of mucosal inflammation but with residual posterior supraglottic submucosal scarring with continued obliteration of posterior supraglottic landmarks and now additional lower supraglottic web. Both true vocal cords continue to look normal and maintain mobility.
- Citation: Dang H, Sun J, Wang G, Renner G, Layfield L, Hilli J. Management of pembrolizumab-induced steroid refractory mucositis with infliximab: A case report. World J Clin Cases 2020; 8(18): 4100-4108
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4100.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4100