Copyright
©The Author(s) 2019.
World J Clin Cases. Mar 6, 2019; 7(5): 562-571
Published online Mar 6, 2019. doi: 10.12998/wjcc.v7.i5.562
Published online Mar 6, 2019. doi: 10.12998/wjcc.v7.i5.562
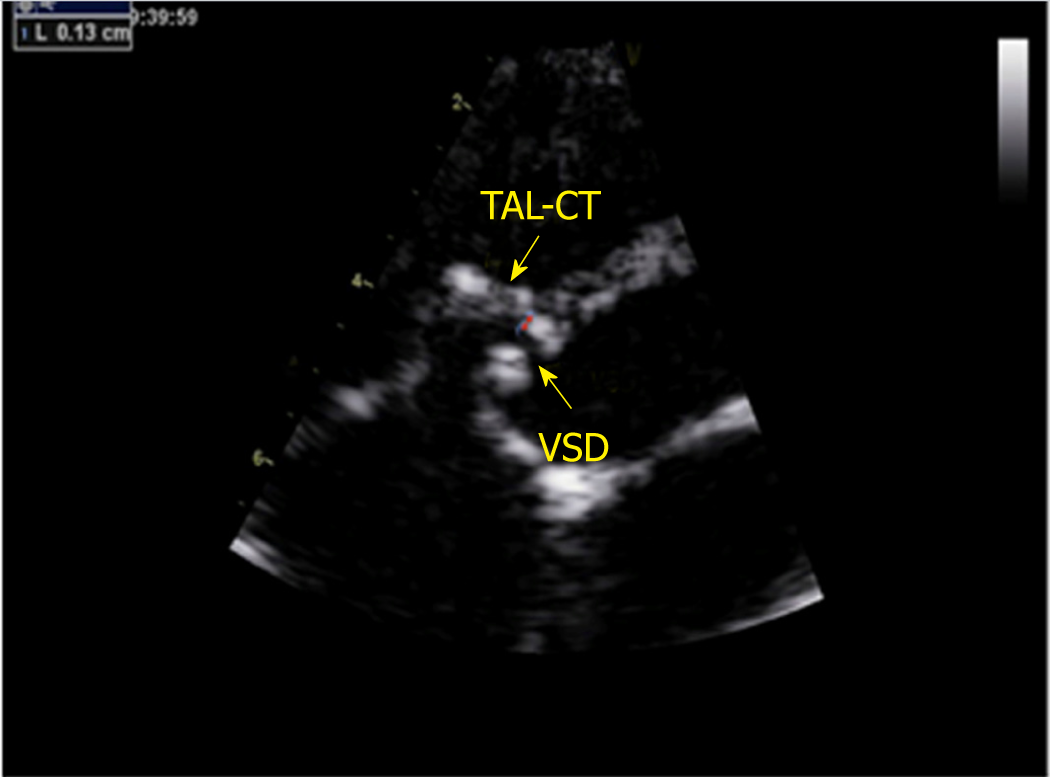
Figure 1 Non-standard aortic short-axis view.
The red arrow shows the distance (1.3 mm) from the attachment point of the tricuspid anterior leaflet chordae tendineae to the inferior edge of the right ventricular side. TAL-CT: Tricuspid anterior leaflet chordae tendineae; VSD: Ventricular septal defects.
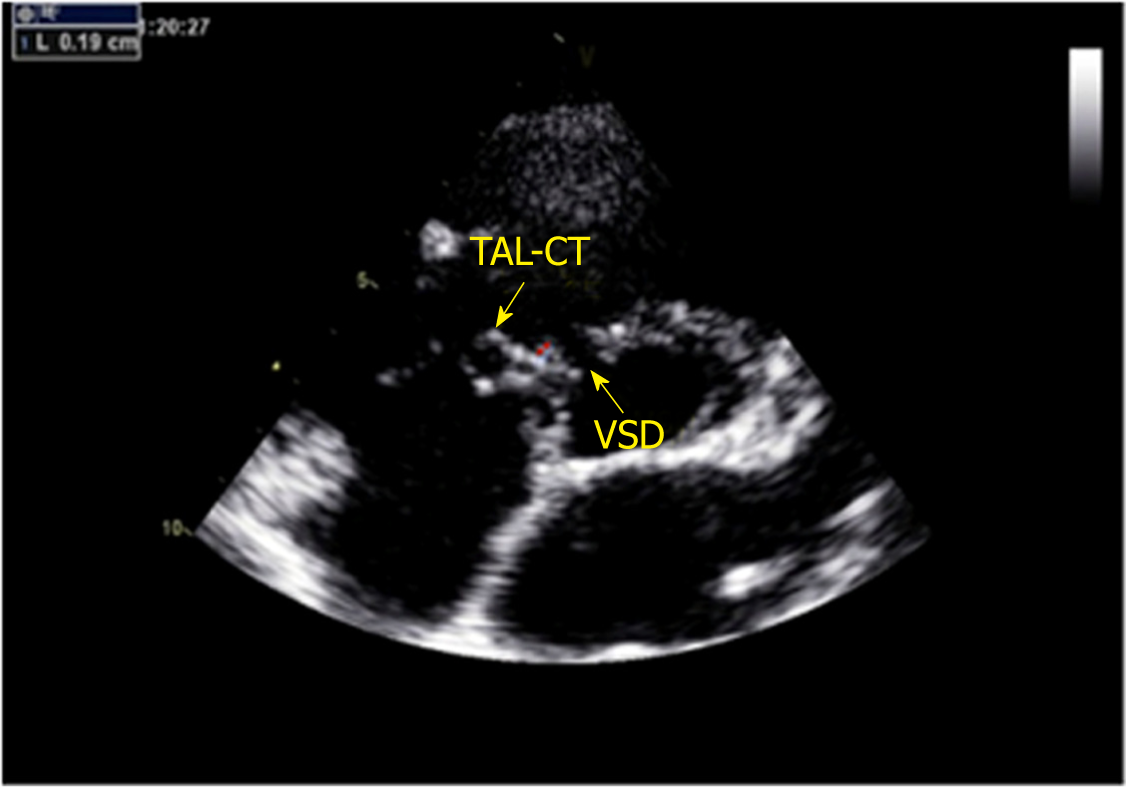
Figure 2 Non-standard aortic short-axis view.
The red arrow shows the distance (1.9 mm) from the attachment point of the tricuspid septal leaflet chordae tendineae to the superior edge of the right ventricular side. TSL-CT: Tricuspid septal leaflet chordae tendineae; VSD: Ventricular septal defects.
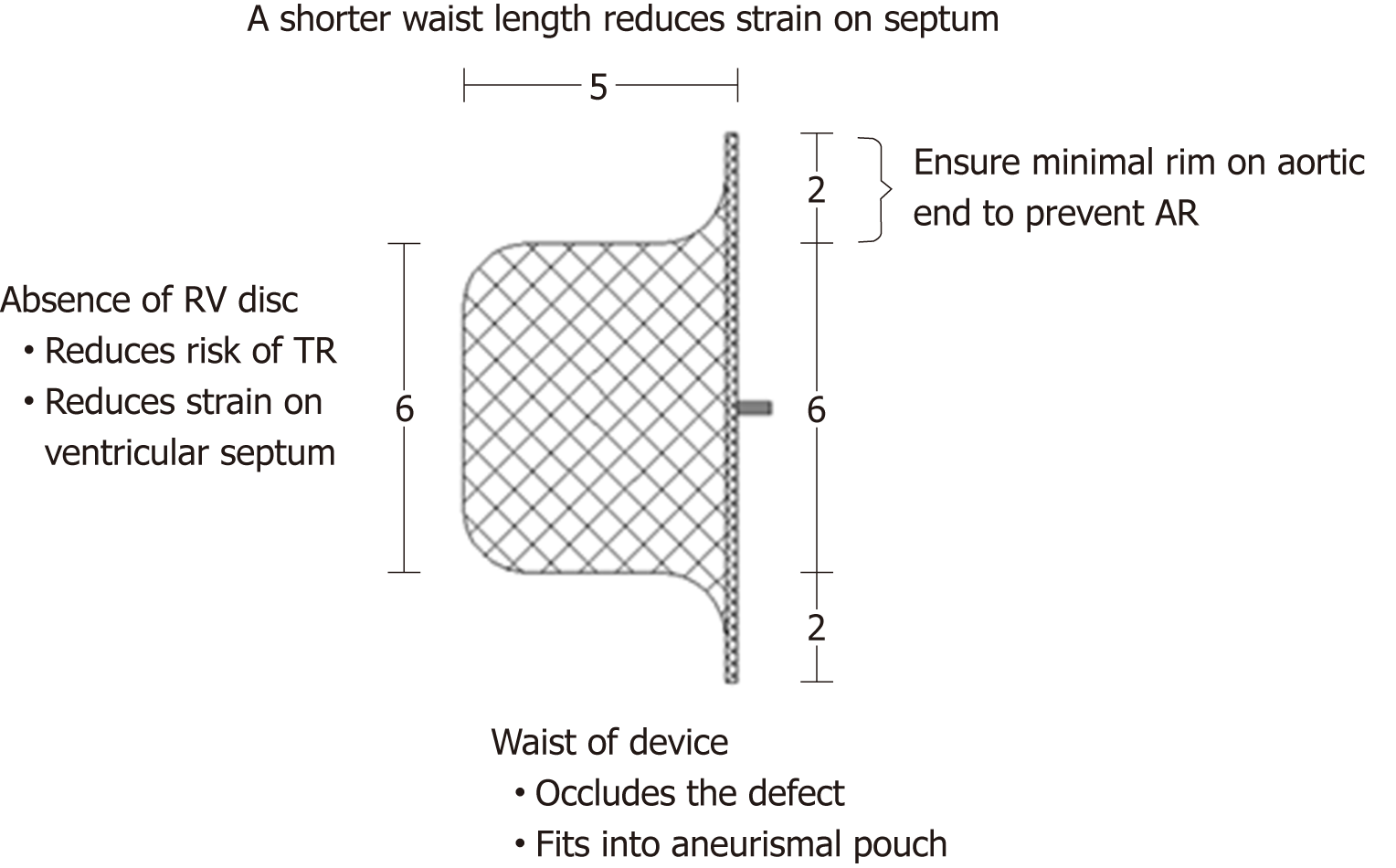
Figure 3 The improved patent ductus arteriosus occluder (6 mm) and its advantages for the closure of perimembranous ventricular septal defects with abnormally attached tricuspid chordae tendineae.
RV: Right ventricular; TR: Tricuspid regurgitation; AR: Aortic regurgitation.
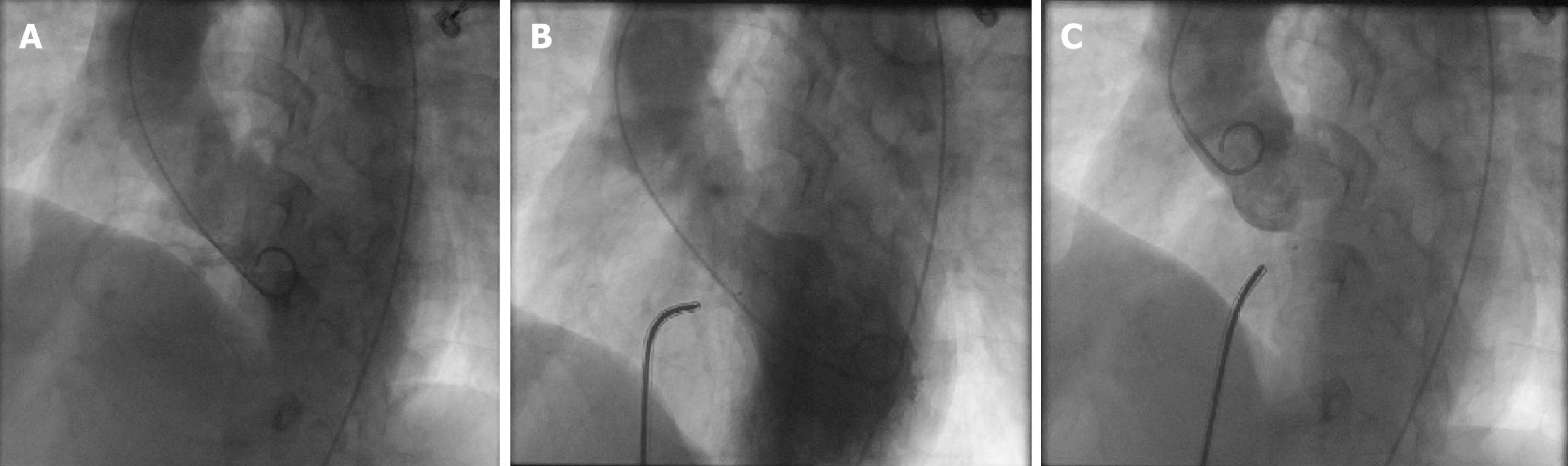
Figure 4 Left ventricle angiography performed before and after the procedure.
A: Left ventricle angiography before the procedure showed perimembranous ventricular septal defects, the diameter of left ventricular side was about 8 mm, and right ventricular side was multiple-outlet with a diameter of about 1.5-2.5 mm; B: Left ventricle angiography after the procedure; C: Angiography of the ascending aorta after the procedure showed that there was no aortic insufficiency.
- Citation: He L, Du YJ, Cheng GS, Zhang YS. Safety of an improved patent ductus arteriosus occluder for transcatheter closure of perimembranous ventricular septal defects with abnormally attached tricuspid chordae tendineae. World J Clin Cases 2019; 7(5): 562-571
- URL: https://www.wjgnet.com/2307-8960/full/v7/i5/562.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i5.562