Copyright
©The Author(s) 2019.
World J Clin Cases. Oct 6, 2019; 7(19): 3039-3046
Published online Oct 6, 2019. doi: 10.12998/wjcc.v7.i19.3039
Published online Oct 6, 2019. doi: 10.12998/wjcc.v7.i19.3039
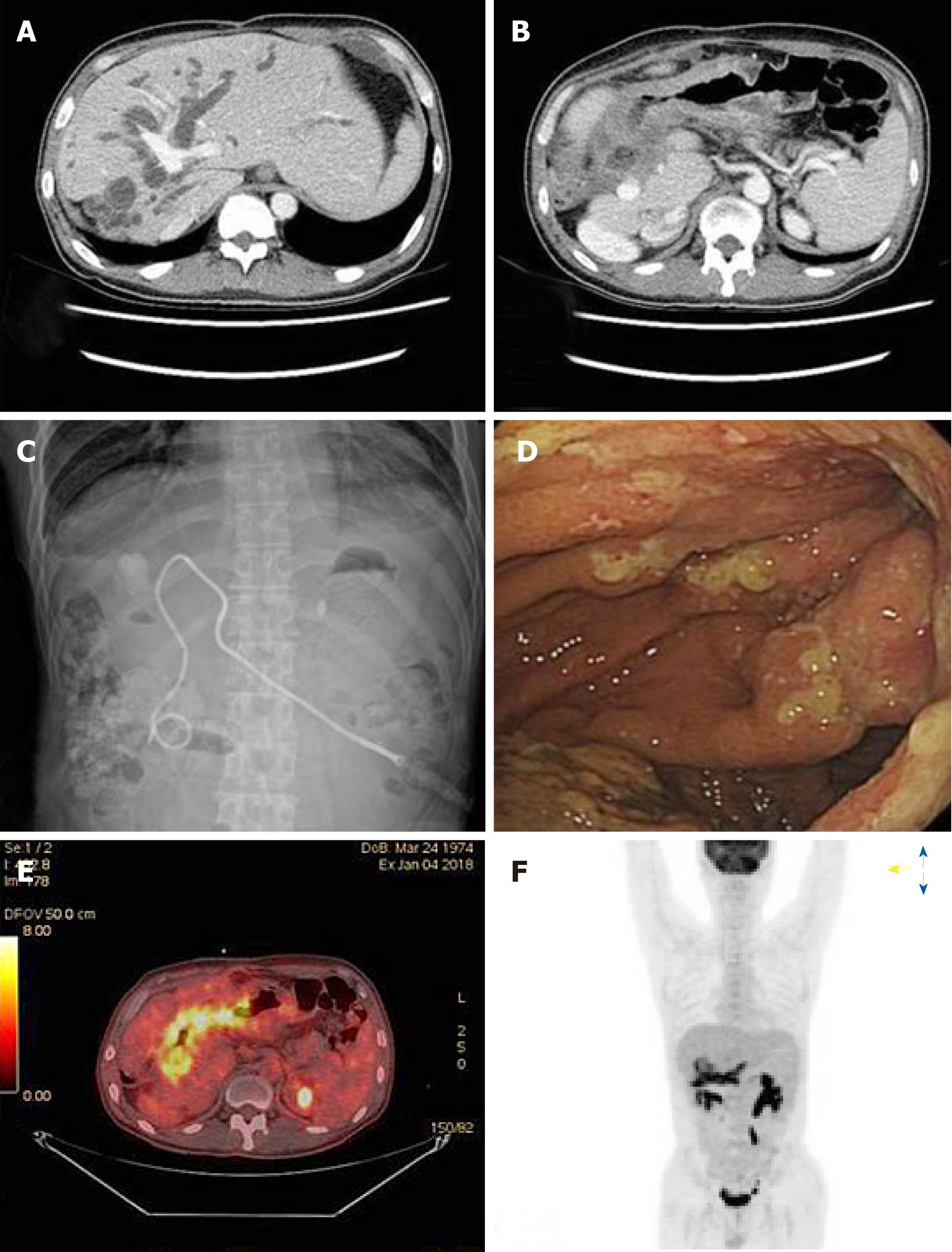
Figure 1 Imaging of admission state.
A and B: Abdominopelvic computed tomography shows that the bile duct was severely dilated due to direct infiltration of the hilar area of the liver by a gastric tumor. C: During percutaneous transhepatic biliary drainage, obstructive jaundice was observed. D: Based on gastroenteroscopy findings, diffuse Bormann type 4 gastric cancer was suspected, accompanied by luminal narrowing and mucosal ulceration. E and F: On positron emission tomography-computed tomography, the mass appeared hypermetabolic, but no distant metastases were detected.
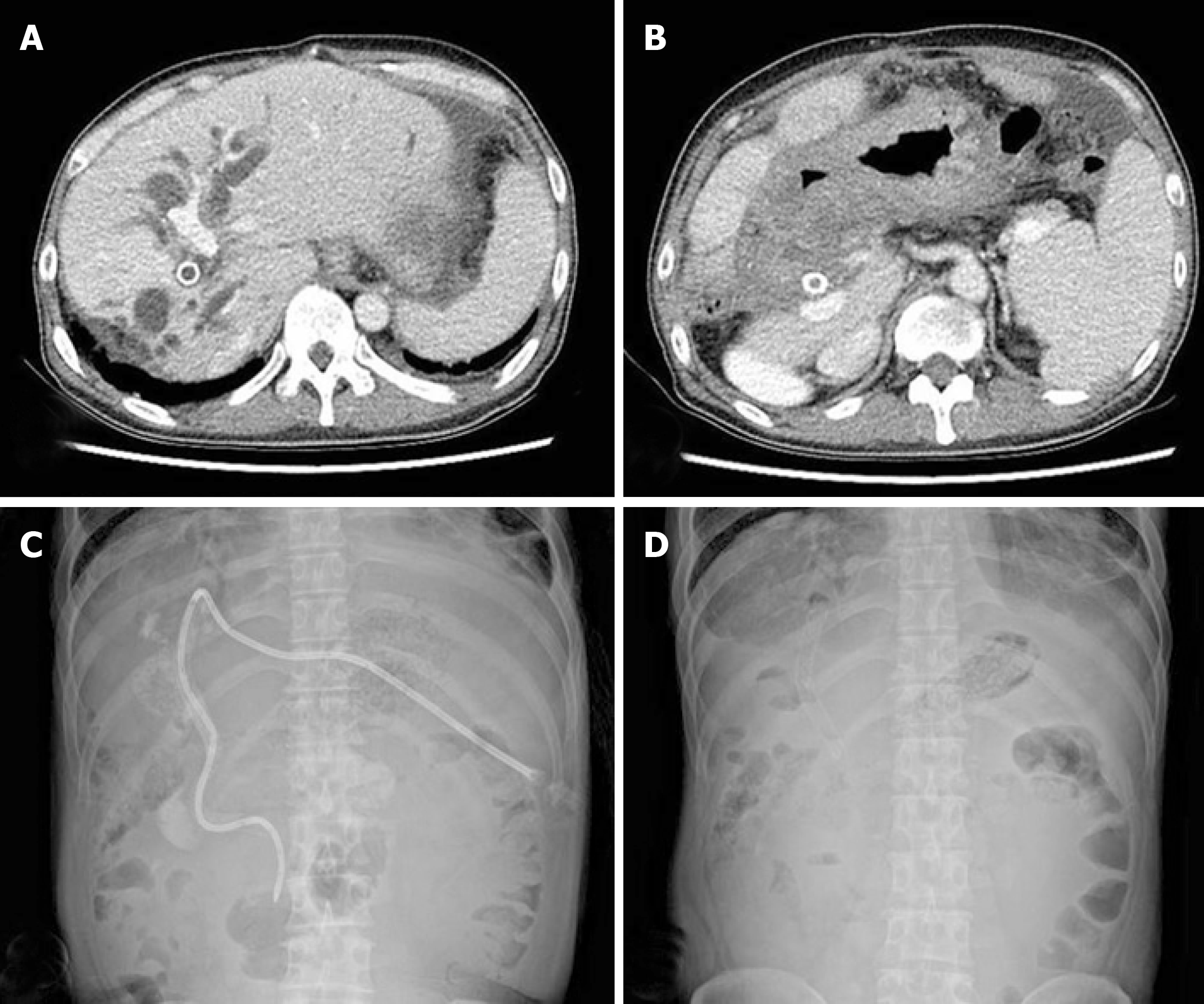
Figure 2 Imaging after first-line chemotherapy.
A and B: Computed tomography showed that the bile duct was dilated, indicating disease progression. C and D: To lower the elevated bilirubin level, percutaneous transhepatic biliary drainage and stent placement were performed again.
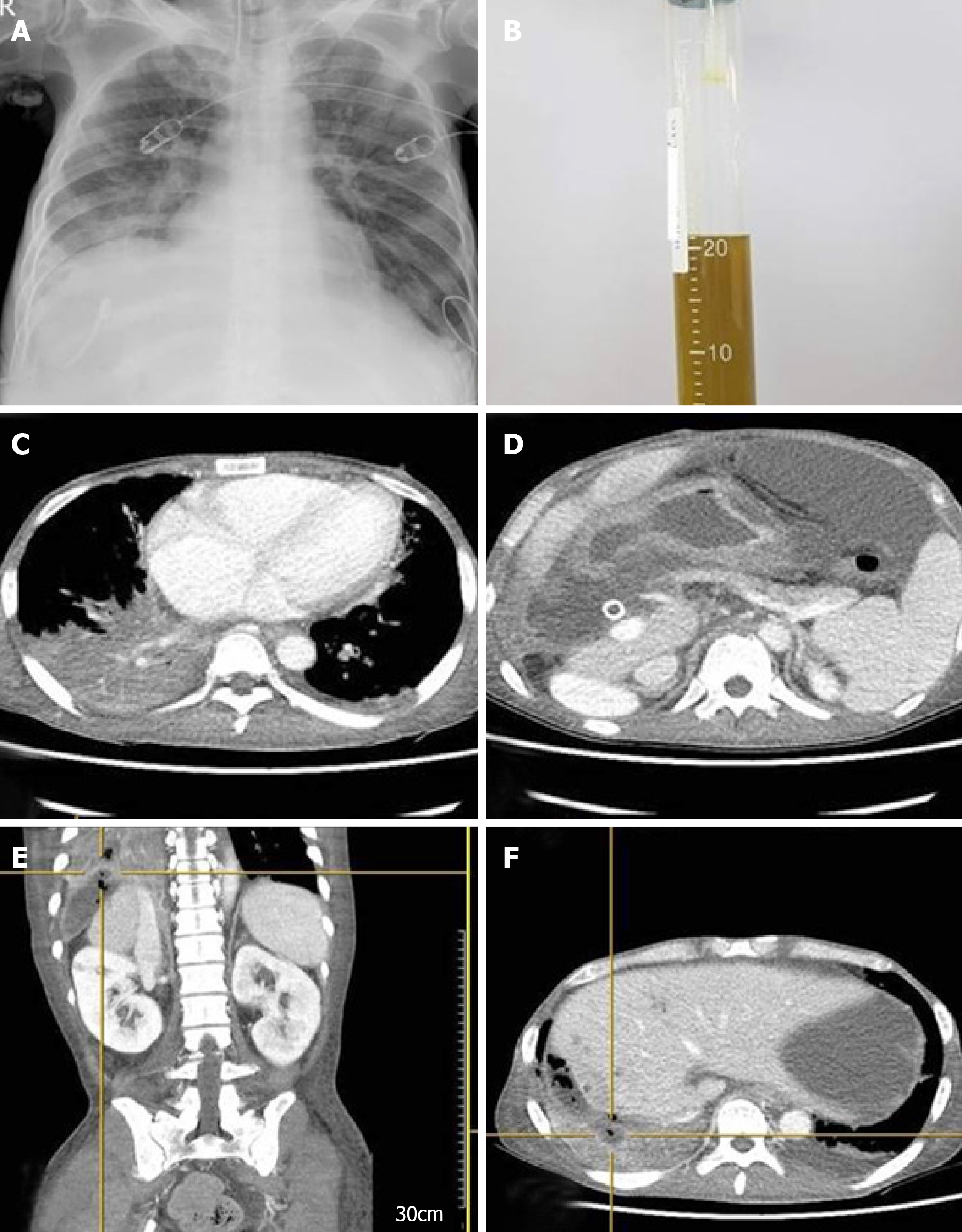
Figure 3 Imaging after emergency room due to respiratory faire.
A: Chest X-ray imaging after emergency room admission revealed pneumonic infiltration in the right lower lobe. B: Greenish bilious sputum was observed after intubation. C and D: Thorax and abdomen computed tomography (CT) showed pneumonic infiltration of the right lower lobe and free air in the perihepatic area, accompanied by fluid collection. E and F: Perforation of the diaphragm was also seen on CT, and bronchobiliary fistula was suspected.
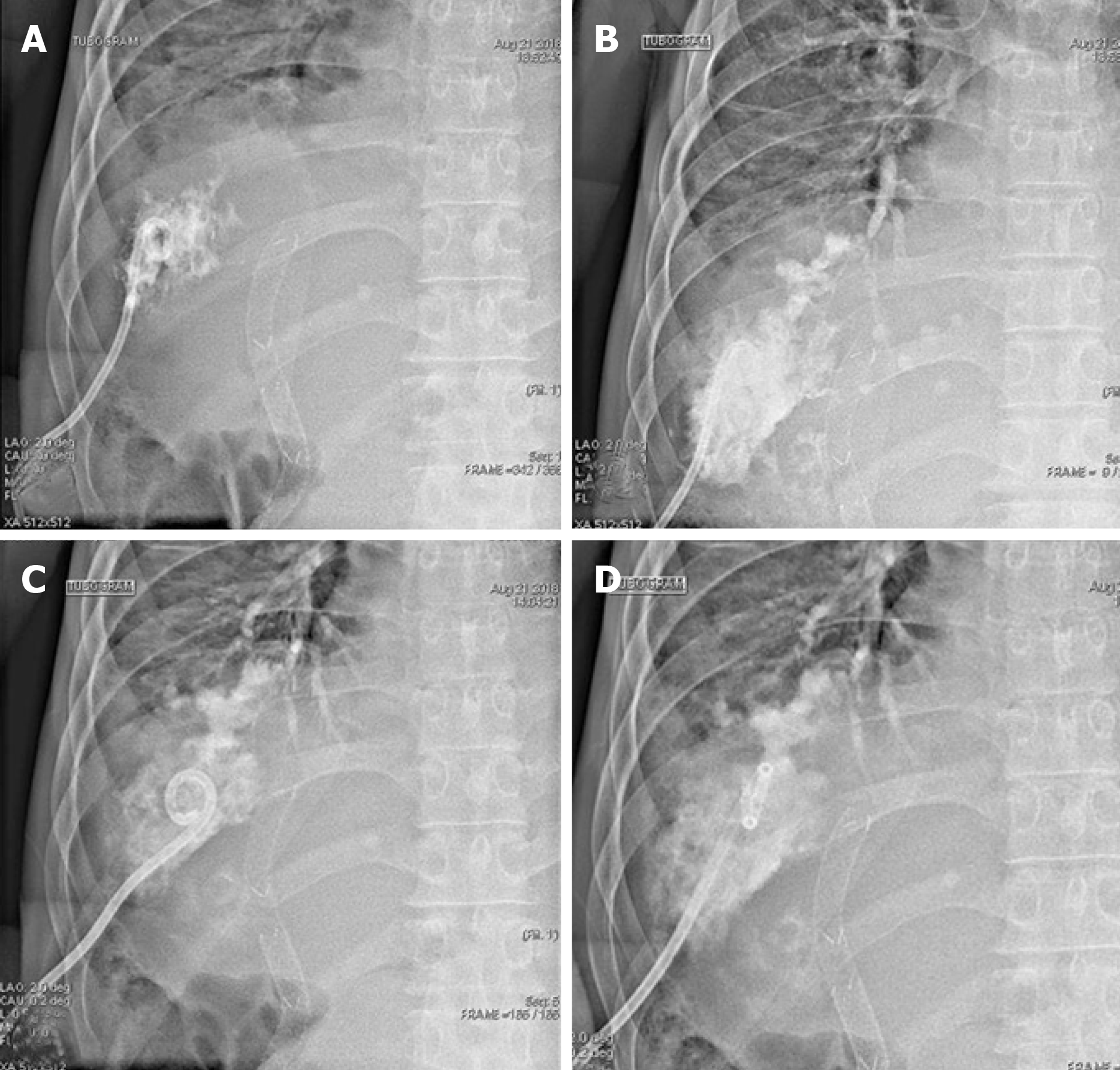
Figure 4 During percutaneous drainage, a tubogram of the perihepatic area showed bile juice leaking from the biliary tract, passing the diaphragm, and forming a fistula directly with the bronchus, confirming the diagnosis of bronchobiliary fistula (A–D).
- Citation: Kim HB, Na YS, Lee HJ, Park SG. Bronchobiliary fistula after ramucirumab treatment for advanced gastric cancer: A case report. World J Clin Cases 2019; 7(19): 3039-3046
- URL: https://www.wjgnet.com/2307-8960/full/v7/i19/3039.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i19.3039