Copyright
©The Author(s) 2019.
World J Clin Cases. Jun 26, 2019; 7(12): 1410-1420
Published online Jun 26, 2019. doi: 10.12998/wjcc.v7.i12.1410
Published online Jun 26, 2019. doi: 10.12998/wjcc.v7.i12.1410
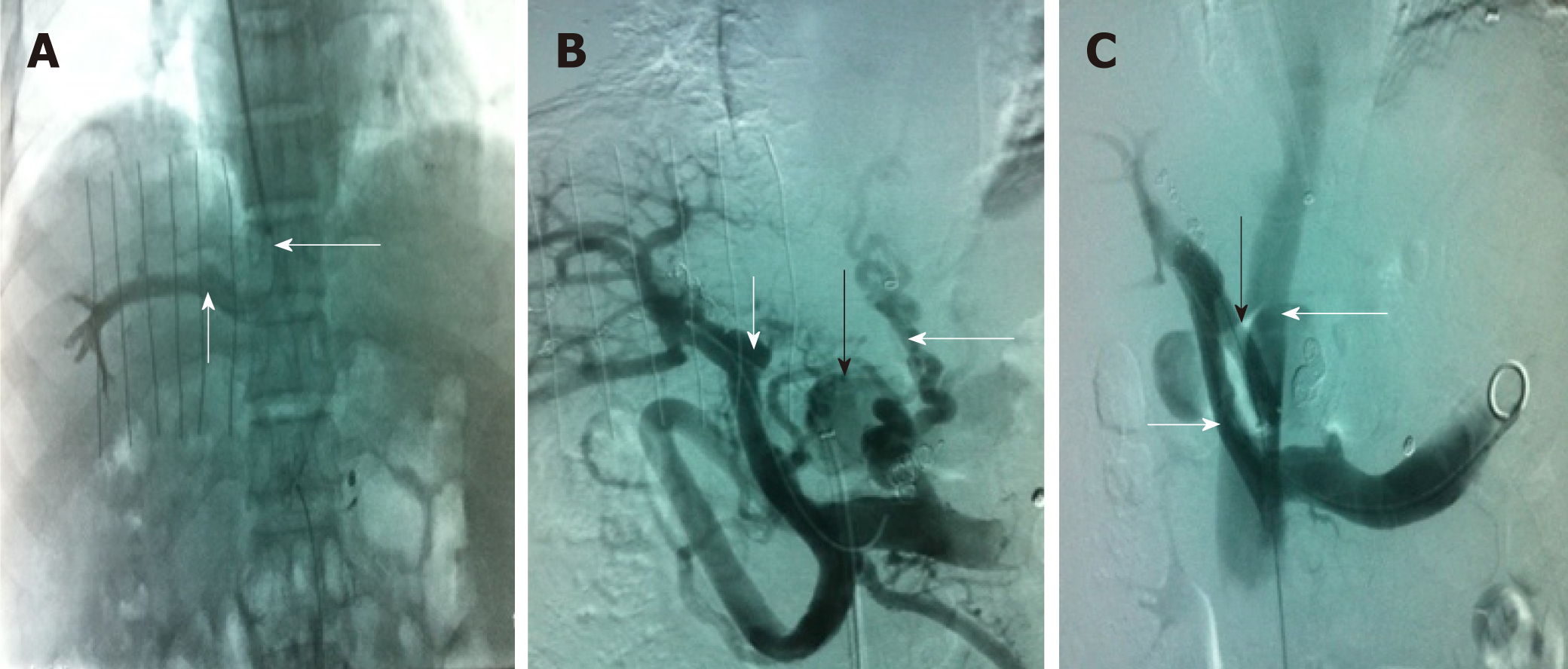
Figure 1 Transjugular intrahepatic portosystemic shunt.
A: Venography of the right hepatic vein via jugular vein catheterization showed that the sharp angles/spatial relationship between the inferior vena cava (long white arrow) and the right hepatic vein (short white arrow) were inappropriate; thus, conventional transjugular intrahepatic portosystemic shunt could not be performed; B: Puncture of the intrahepatic portal vein through the inferior vena cava via femoral vein access and venography. The venogram showed the portal vein (short white arrow), lateral branch (black arrow) and varicose vein (long white arrow); C: The shunt (black arrow) between the portal vein (short white arrow) and the inferior vena cava (long white arrow) was successfully created. Subsequently, the varicose veins and collateral vessels disappeared completely.
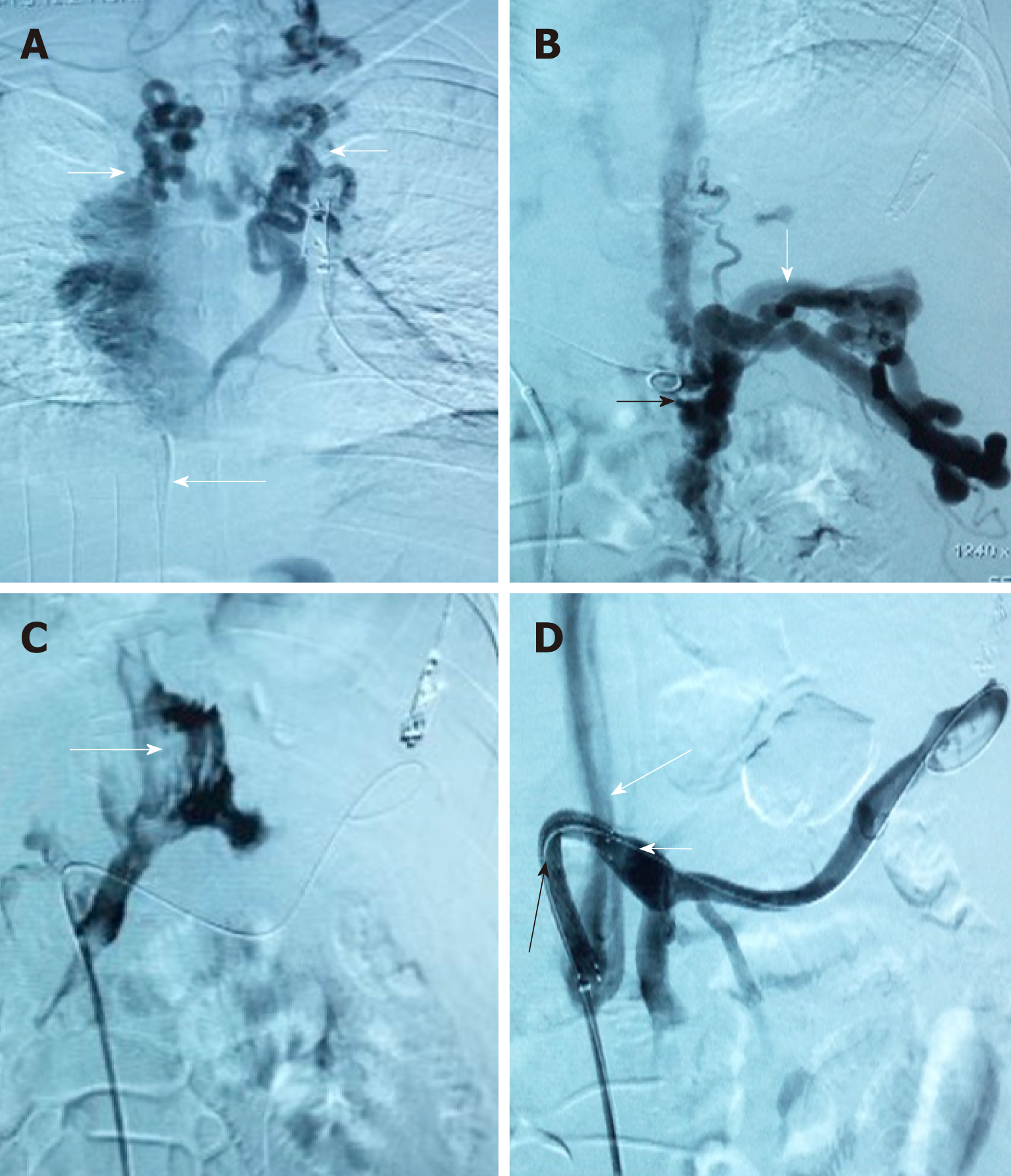
Figure 2 Computed tomography and transjugular intrahepatic portosystemic shunt.
A: Inferior vena cava stent (black long arrow); B: Liver caudate lobe is much bigger due to congestion, which makes the portal vein (black short arrow) become nearer to the abdominal wall. The acute angle between the inferior vena cava and internal portal vein is unorthodox; C: Puncture of the intrahepatic portal vein through the inferior vena cava via femoral vein access and venography. The venogram showed the portal vein (short white arrow) and the varicose vein (long white arrow); D: A Scoop channel between the portal vein (short white arrow) and the inferior vena cava (long white arrow) was successfully established with the stent (black arrow). The varicose veins disappeared completely.
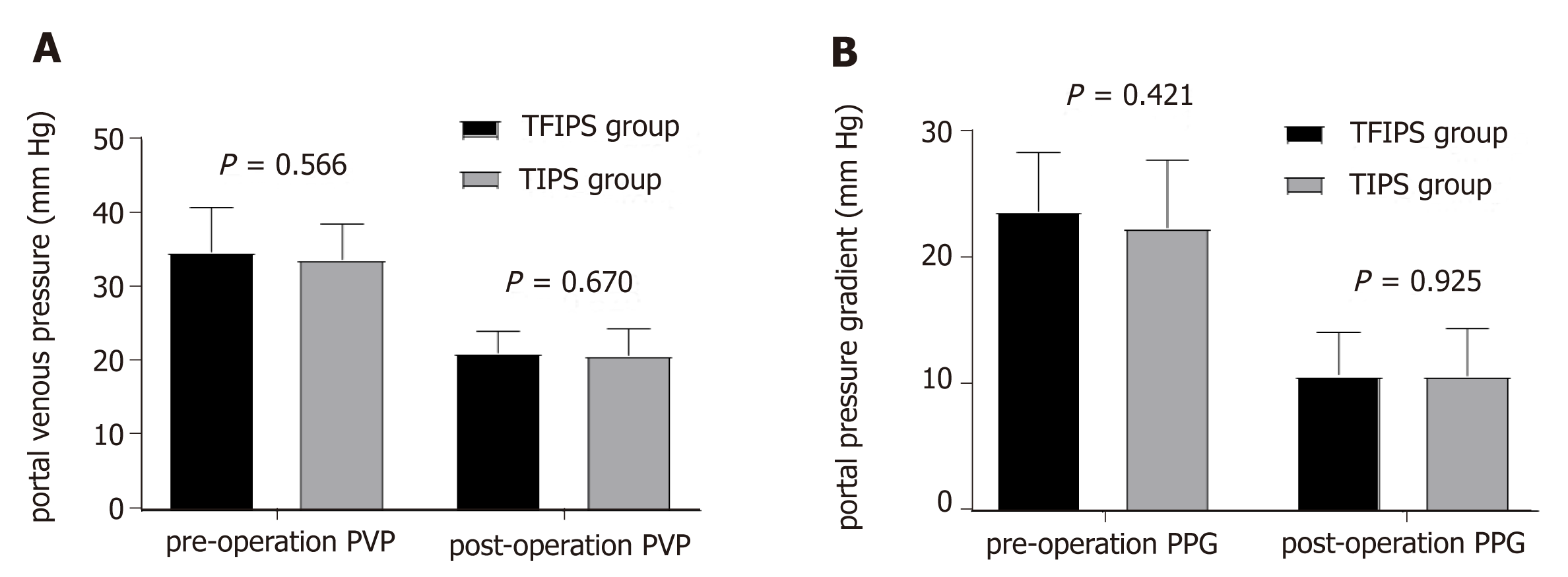
Figure 3 Due to complete occlusion of the bilateral jugular vein and/or superior vena cava, transjugular intrahepatic portosystemic shunt could not be performed in 3 cases.
A: Venogram via jugular vein access indicated that cavernous transformation of the bilateral jugular vein (white short arrow) and superior vena cava was occluded (long white arrow). Thus, conventional transjugular intrahepatic portosystemic shunt could not be performed; B: Puncture of the intrahepatic portal vein through the inferior vena cava via femoral vein access and venography. The venogram showed the angiography catheter in the portal vein (black arrow) and portal vein blood flow reflux into the hepatic varicose veins (long white arrow); C: The venogram showed that the contrast agent infiltrated the abdominal cavity (long white arrow) when the hepatic vein was punctured via the inferior vena cava; D: A semi-arc shunt between the portal vein (short white arrow) and the inferior vena cava (long white arrow) was successfully created using the covered stent (black arrow). Subsequently, the varicose veins disappeared completely.
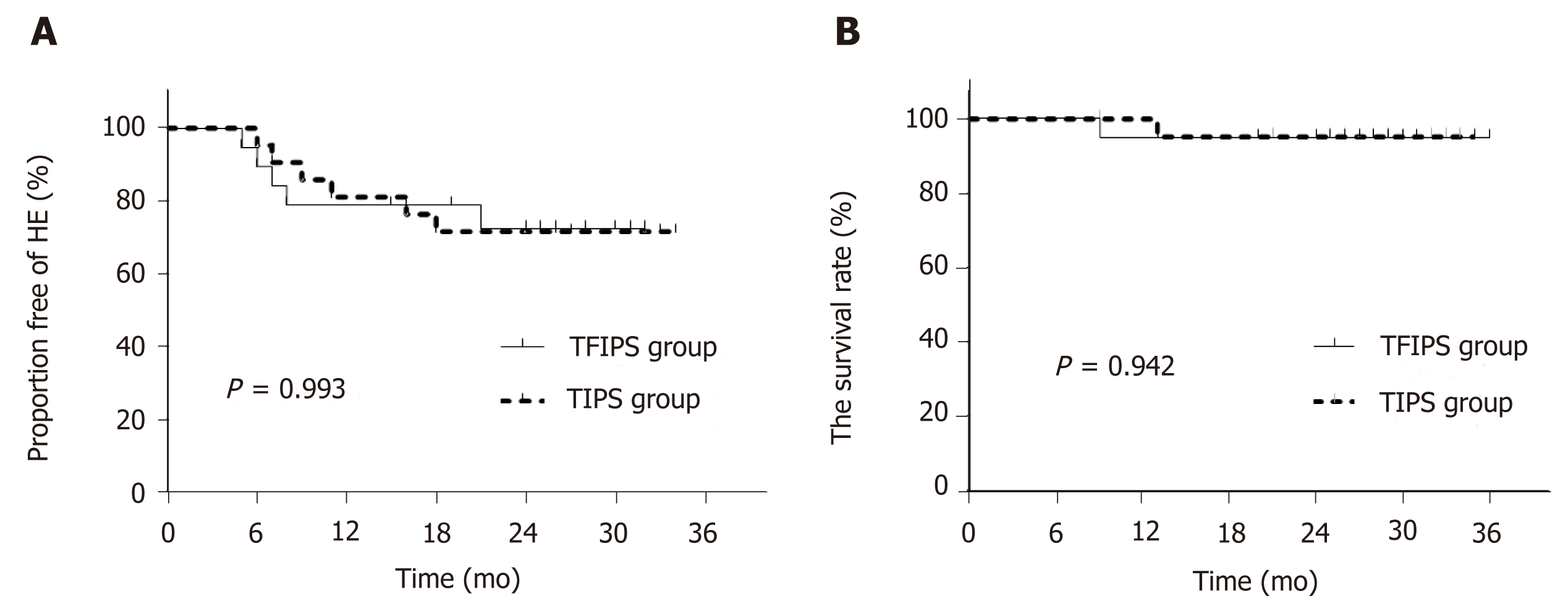
Figure 4 No statistically significant differences were observed between the two groups in terms of portal vein pressure and portal pressure gradient before and after surgery.
PVP: Portal vein pressure; PPG: Portal pressure gradient; TFIPS: Transfemoral intrahepatic portosystemic shunt; TIPS: Transjugular intrahepatic portosystemic shunt.
Figure 5 Time-to-event (Kaplan-Meier) de novo hepatic encephalopathy analysis.
There were no significant differences between the two groups. TFIPS: Transfemoral intrahepatic portosystemic shunt; TIPS: Transjugular intrahepatic portosystemic shunt.
- Citation: Zhang Y, Liu FQ, Yue ZD, Zhao HW, Wang L, Fan ZH, He FL. Safety and efficacy of transfemoral intrahepatic portosystemic shunt for portal hypertension: A single-center retrospective study. World J Clin Cases 2019; 7(12): 1410-1420
- URL: https://www.wjgnet.com/2307-8960/full/v7/i12/1410.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i12.1410