Copyright
©The Author(s) 2018.
World J Clin Cases. Nov 6, 2018; 6(13): 624-631
Published online Nov 6, 2018. doi: 10.12998/wjcc.v6.i13.624
Published online Nov 6, 2018. doi: 10.12998/wjcc.v6.i13.624
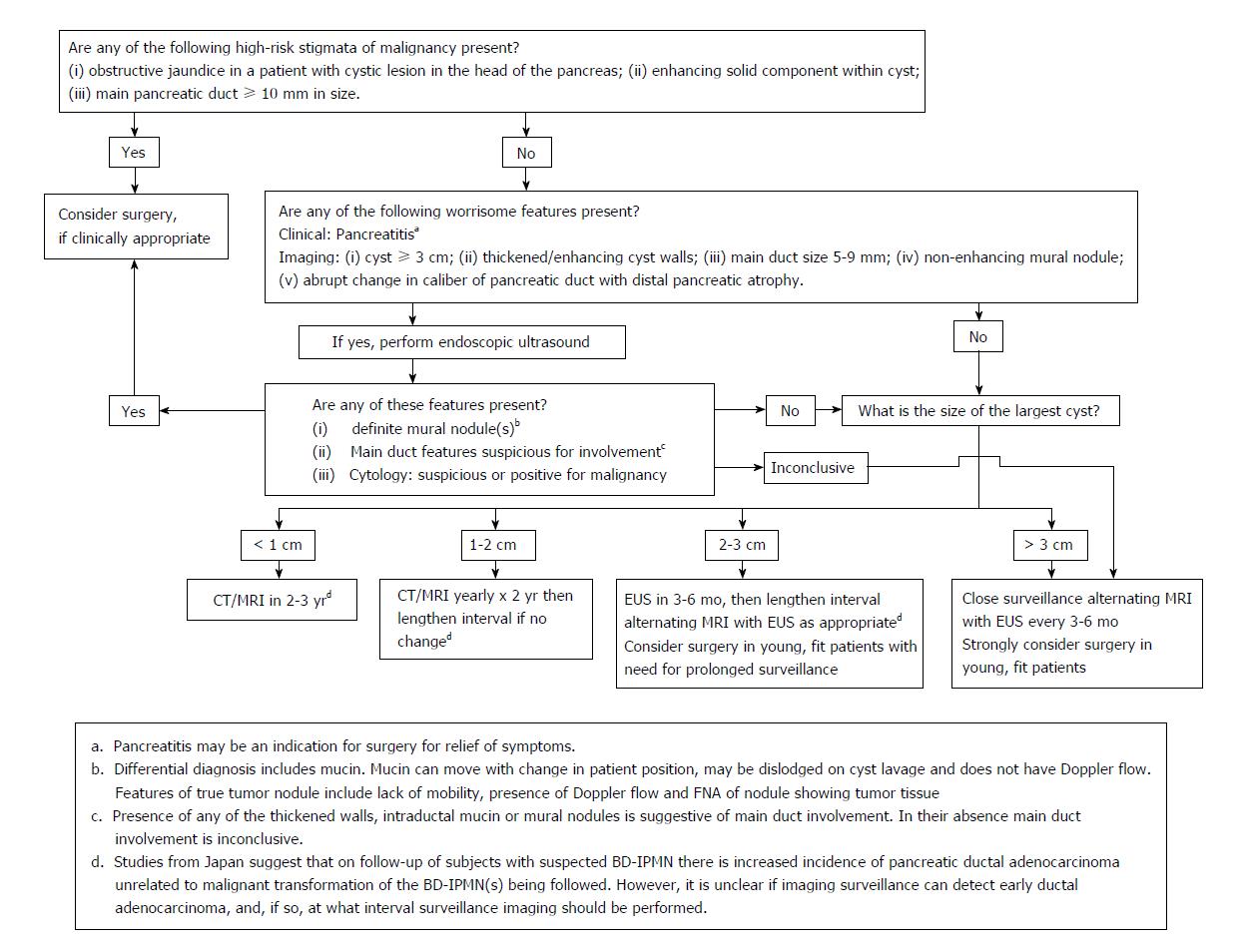
Figure 1 Fukuoka algorithm for the management of pancreatic cystic lesions (suspected branchduct-intraductal papillary mucinous neoplasms)[8].
CT: Computed tomography; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography; FNA: Fine-needle aspiration; BD-IPMN: Branch duct-intraductal papillary mucinous neoplasm.
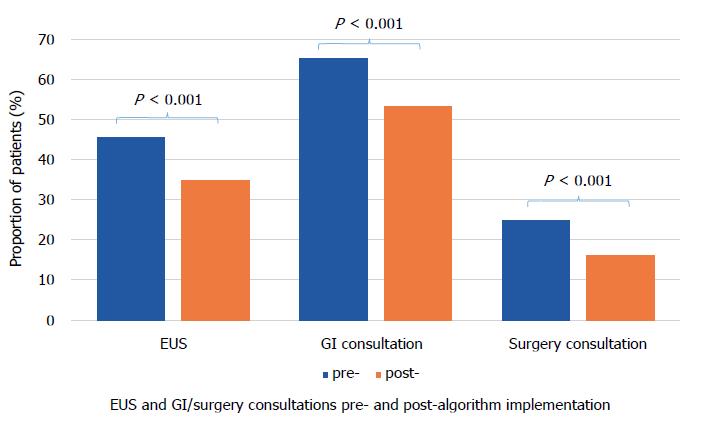
Figure 2 Endoscopic ultrasound and gastroenterology/surgery consultations pre- and post-algorithm.
EUS: Endoscopic ultrasound; GI: Glycemic Index.
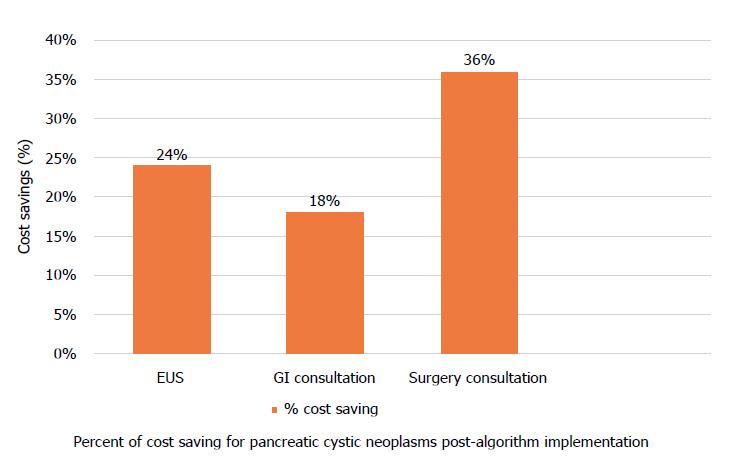
Figure 3 Cost savings for endoscopic ultrasound and gastroenterology/surgery consultations post-algorithm.
EUS: Endoscopic ultrasound; GI: Glycemic Index.
- Citation: Nguyen AK, Girgis A, Tekeste T, Chang K, Adeyemo M, Eskandari A, Alonso E, Yaramada P, Chaya C, Ko A, Burke E, Roggow I, Butler R, Kawatkar A, Lim BS. Effect of a region-wide incorporation of an algorithm based on the 2012 international consensus guideline on the practice pattern for the management of pancreatic cystic neoplasms in an integrated health system. World J Clin Cases 2018; 6(13): 624-631
- URL: https://www.wjgnet.com/2307-8960/full/v6/i13/624.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i13.624