Copyright
©The Author(s) 2018.
World J Clin Cases. Oct 6, 2018; 6(11): 472-476
Published online Oct 6, 2018. doi: 10.12998/wjcc.v6.i11.472
Published online Oct 6, 2018. doi: 10.12998/wjcc.v6.i11.472
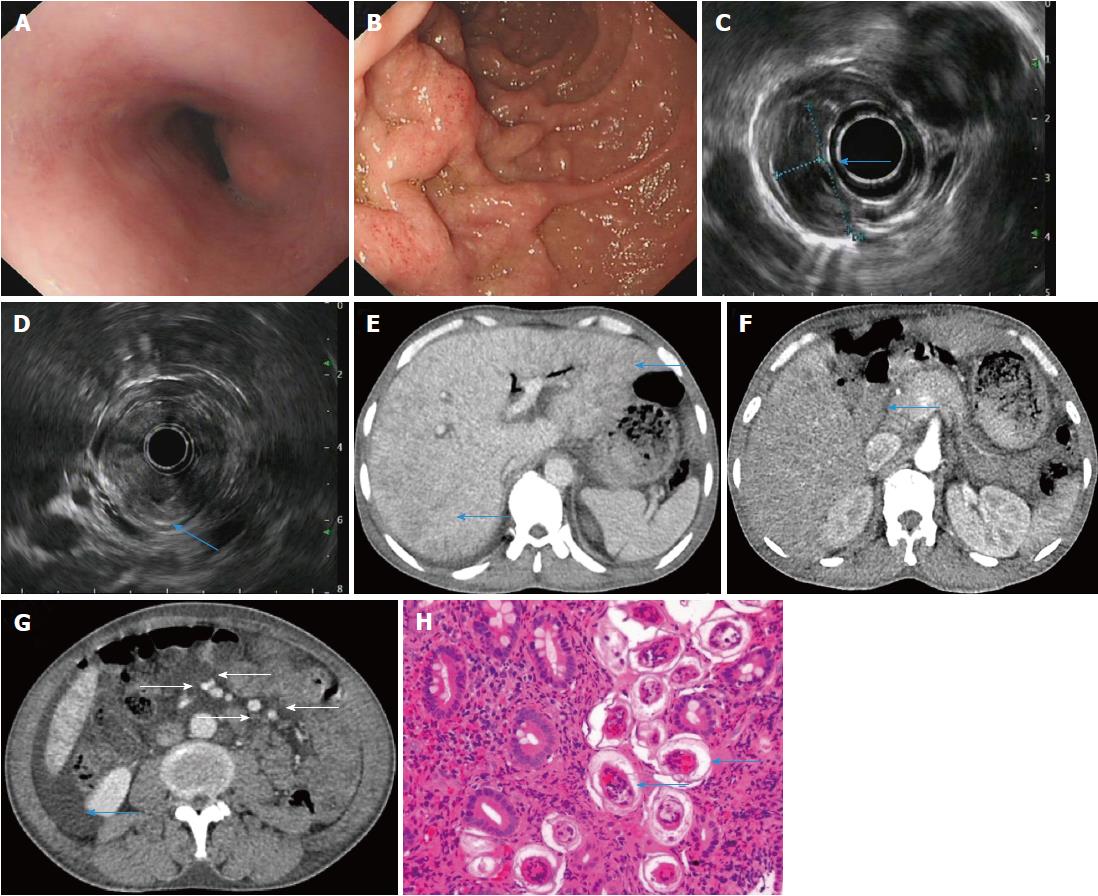
Figure 1 A 47-year-old male patient with acute Schistosoma japonicum infection underwent endoscopic examination, endoscopic ultrasonography and dynamic computed tomography scanning at the baseline visit.
A, B: Upper gastrointestinal endoscopy showing protrusive lesions in the esophagus (A), swollen mucosa and protrusive lesions in the descending duodenum (B); C, D: Endoscopic ultrasonography revealing a hypoechoic mass in the muscularis mucosa of the esophagus (C, arrow), thickening of the descending duodenal wall, and destruction of the descending duodenal wall (D, arrow); E-G: Dynamic computed tomography showing heterogeneous hypointensity in the liver (E, arrow), thickening of the descending duodenal wall (F, arrow), swollen mesentery around the arteries (G, arrow), and ascites; H: Biopsy of the descending duodenum showing deposition of Schistosoma eggs.
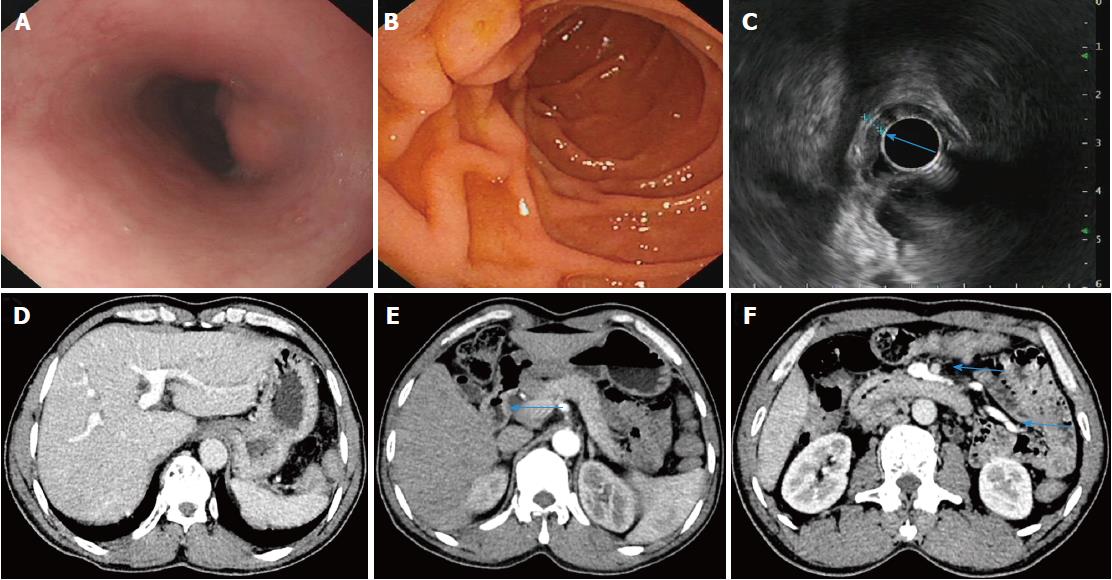
Figure 2 Following administration of praziquantel, the patient with acute Schistosoma japonicum infection received a complete check-up at the follow-up visit.
A, B: Upper gastrointestinal endoscopy showing protrusive lesions of the esophagus (A) and normal mucosa in the descending duodenum (B); C: Endoscopic ultrasonography revealing slight thickening and normal layer of the descending duodenal wall; D-F: Dynamic abdominal computed tomography showing homogeneous hepatic perfusion on the portal phase (D), slight thickening of the descending wall (E, arrow), shrinkage of the swollen mesentery to normal size (F, arrow), and disappearance of ascites.
- Citation: Xiao ZL, Xu KS, Song YH. Unusual cause of lesions in the descending duodenum and liver: A case report and review of literature. World J Clin Cases 2018; 6(11): 472-476
- URL: https://www.wjgnet.com/2307-8960/full/v6/i11/472.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i11.472