Copyright
©The Author(s) 2018.
World J Clin Cases. Oct 6, 2018; 6(11): 459-465
Published online Oct 6, 2018. doi: 10.12998/wjcc.v6.i11.459
Published online Oct 6, 2018. doi: 10.12998/wjcc.v6.i11.459
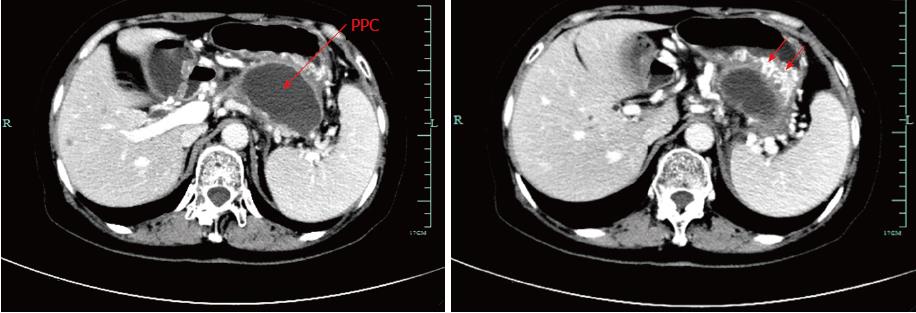
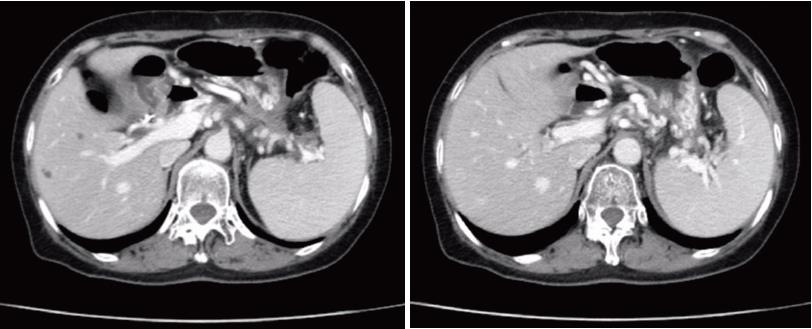
Figure 1 Pre-procedural contrast-enhanced computed tomography image.
Computed tomography (CT) scan of the upper abdomen images revealed a 7.4 cm × 6.2 cm pancreatic pseudocyst in the tail of the pancreas, which was in close contact with the posterior wall of the stomach. Notably, splenic vein occlusion, splenomegaly and gastric varices were also observed.
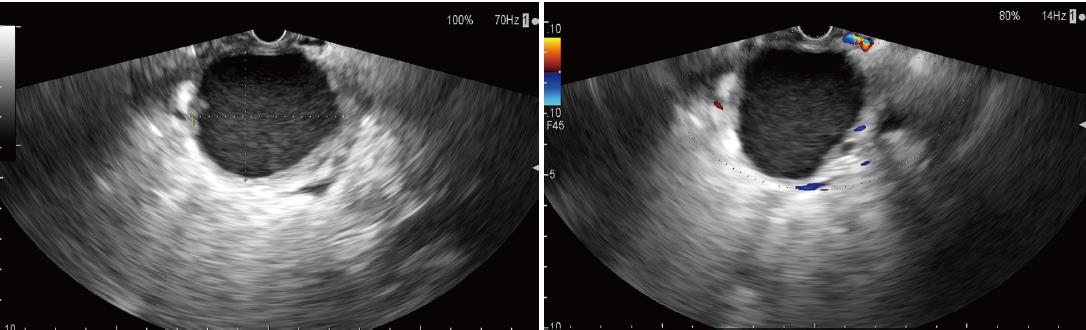
Figure 2 Endoscopic ultrasound image.
These revealed a homogeneous pseudocyst mass, and the cyst wall had a thickness of approximately 10 mm. Good adhesion was noted between the cyst wall and the posterior gastric wall.
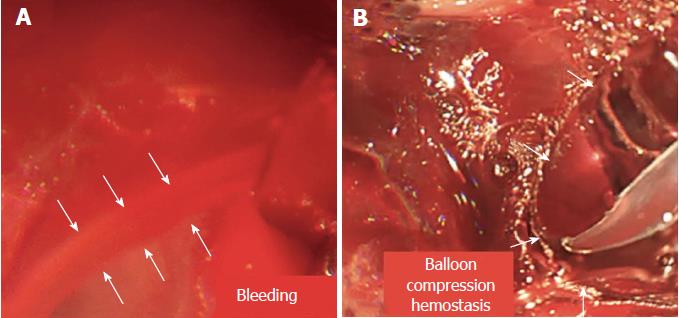
Figure 3 Endoscopic images.
A: Endoscopic images during the procedure revealed acute and massive bleeding surrounding the fistula, and the blood flowed like a stream; B: Endoscopic images revealed that the massive bleeding was stopped via the compression of balloon dilator to achieve effective hemostasis, significantly impacting the patient’s condition.
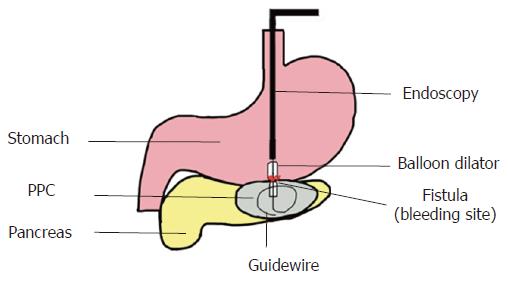
Figure 4 Schematic diagram of the procedure.
A small balloon was expanded to 1 cm using a pressure pump, and contrast agent was administered. We used the balloon dilator to compress the bleeding area and achieve effective hemostasis.
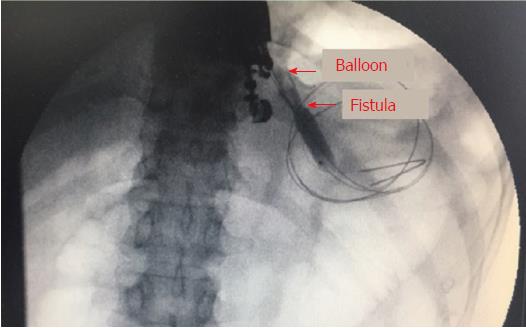
Figure 5 Image of digital subtraction angiography.
It revealed a balloon dilator compressing the bleeding area. The digital subtraction angiography (DSA) guided and ensured that the balloon was in the correct location surrounding the fistula. DSA imaging also revealed balloon dilation of the tract.
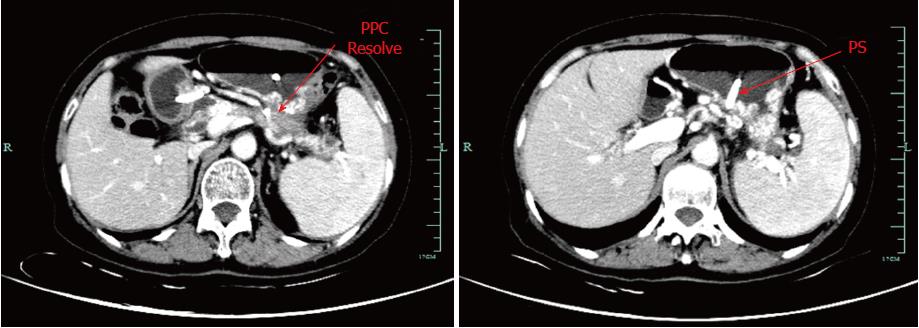
Figure 6 Follow-up contrast-enhanced computed tomography images.
Computed tomography scan of the abdomen revealing a significant decrease in the size of the pseudocyst with a double pig plastic stent in position two months after endoscopy ultrasound-guided placement of a visible plastic stent between the stomach and residual pancreatic pseudocyst. The stent also effectively drained the pseudocyst and relieved the severely affected collateral vessels.
Figure 7 Follow-up contrast-enhanced computed tomography scan images.
Contrast-enhanced computed tomography of the abdomen demonstrating that the pseudocyst was completely resolved three months after stent removal. No reoccurrence was noted, as indicated by the significant resolution of the serious perisplenic and gastric varices.
- Citation: Wang BH, Xie LT, Zhao QY, Ying HJ, Jiang TA. Balloon dilator controls massive bleeding during endoscopic ultrasound-guided drainage for pancreatic pseudocyst: A case report and review of literature. World J Clin Cases 2018; 6(11): 459-465
- URL: https://www.wjgnet.com/2307-8960/full/v6/i11/459.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i11.459