Copyright
©The Author(s) 2016.
World J Clinical Cases. Sep 16, 2016; 4(9): 290-295
Published online Sep 16, 2016. doi: 10.12998/wjcc.v4.i9.290
Published online Sep 16, 2016. doi: 10.12998/wjcc.v4.i9.290
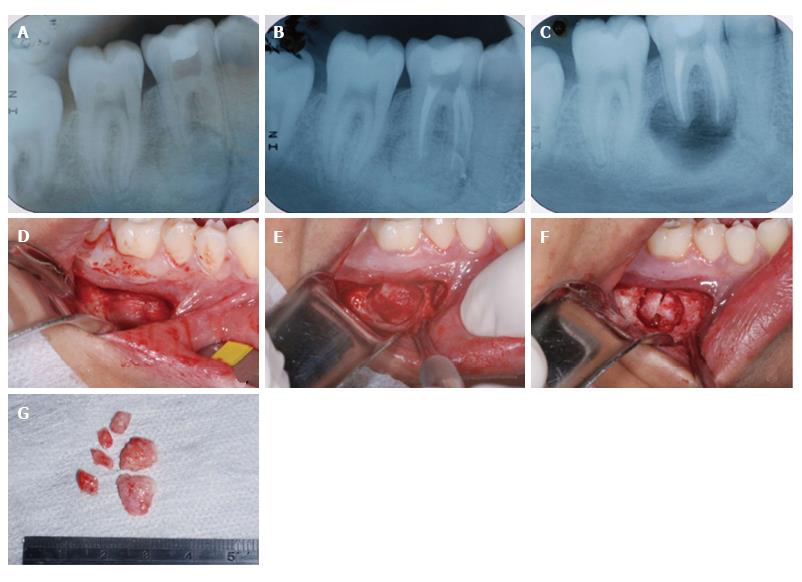
Figure 1 Initial diagnosis and treatment of the lesion.
A: Initial radiographic exam showing radiopaque lesion with radiolucent halo involving the distal root of tooth 46; B: Endodontic treatment; C: Radiographic aspect after the first surgical intervention, with removal of the lesion and apical third of the root involved with the lesion; D: Access to the vestibular region of tooth 46; E: Exposure of the lesion; F: Fragmentation of the lesion to facilitate its removal; G: Aspect of the lesion removed.
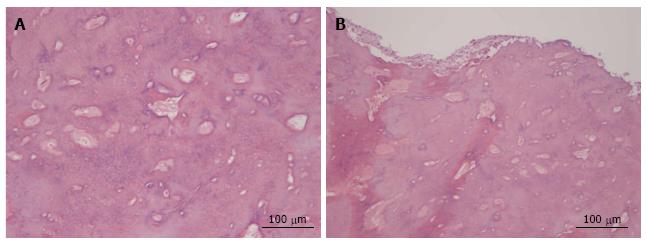
Figure 2 Histological analysis of the lesion.
A: Central region of the lesion, where a cementoid structure with blood vessels was observed, presenting superimposed lamellae and basophilic material; B: Peripheral region of the lesion that presented irregular fibrous tissue, with tissue having a cementoid aspect and presence of blood vessels (HE-50 × magnification).
Figure 3 Tomographic aspect of tooth 46, one year after the first surgical procedure.
A: General panoramic image; B: Image of the sagittal plane, in which tooth 46 is pointed out, with presence of the recurrence of cementoblastoma lesion associated with the distal root; C: Image of the coronal plane in which it is possible to observe a radiopaque alteration associated with tooth 46.
Figure 4 Second surgical intervention and follow-up one year after this procedure.
A: Radiographic aspect after removal of the lesion; B: Radiographic aspect after 1 year, in which it is possible to visualize a normal radiographic aspect around the root of the previously affected tooth.
- Citation: Costa BC, de Oliveira GJPL, Chaves MDGAM, da Costa RR, Gabrielli MFR, Guerreiro-Tanomaru JM, Tanomaru-Filho M. Surgical treatment of cementoblastoma associated with apicoectomy and endodontic therapy: Case report. World J Clinical Cases 2016; 4(9): 290-295
- URL: https://www.wjgnet.com/2307-8960/full/v4/i9/290.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i9.290