Copyright
©The Author(s) 2024.
World J Clin Cases. Jul 26, 2024; 12(21): 4842-4852
Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4842
Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4842
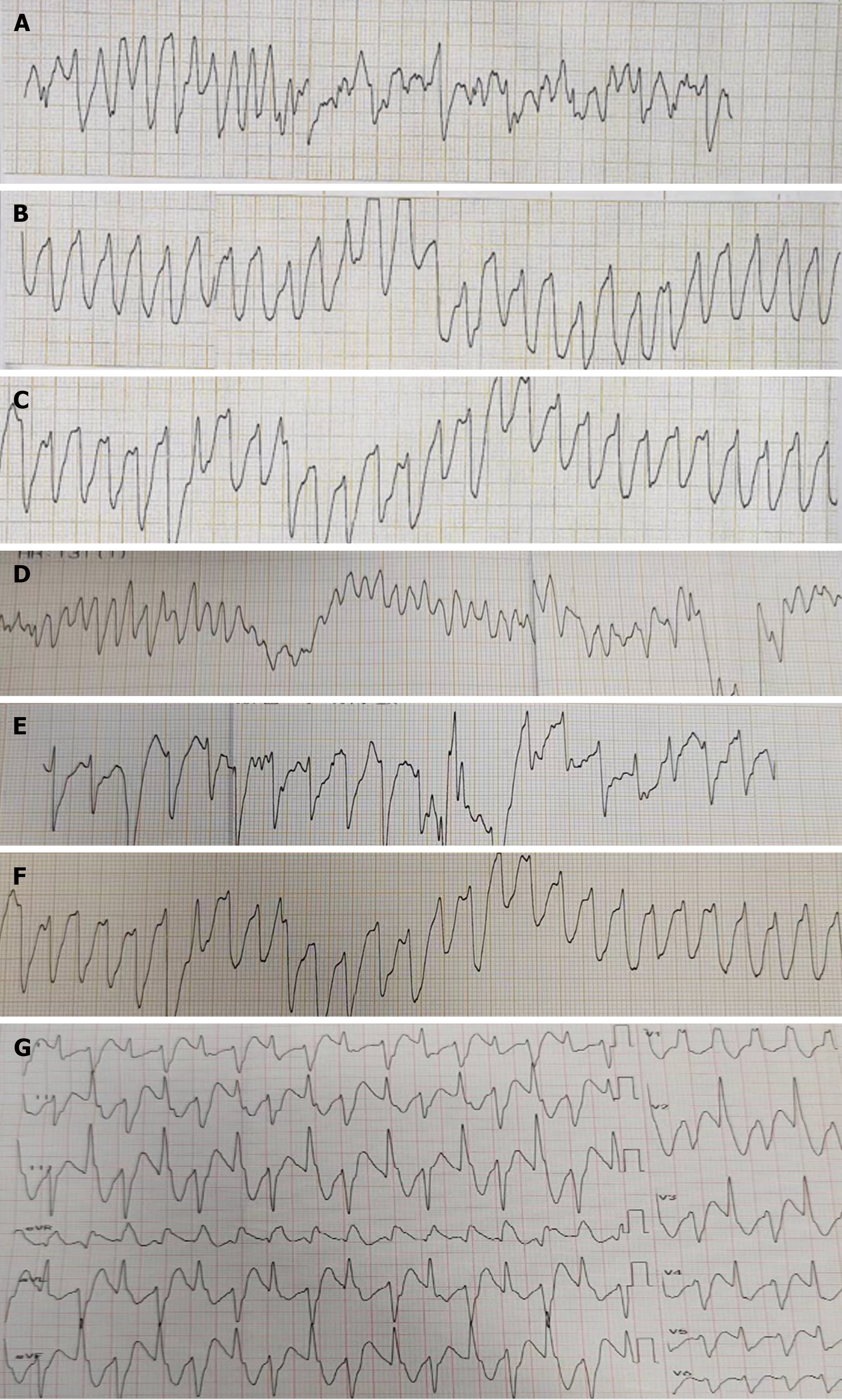
Figure 1 The patient's electrocardiogram and cardiac monitoring changes after entering the hospital.
A: Ventricular fibrillation and ventricular tachycardia on electrocardiogram 1 (September 8, 2022 16:27-17:06); B: Ventricular fibrillation and ventricular tachycardia on electrocardiogram 1 (September 8, 2022 16:59); C: Ventricular fibrillation and ventricular tachycardia on electrocardiogram 1 (September 8, 2022 17:06); D: Ventricular fibrillation and ventricular tachycardia on electrocardiogram 2 (September 8, 2022 17:22); E: Ventricular fibrillation and ventricular tachycardia on electrocardiogram 2 (September 8, 2022 17:24); F: Ventricular fibrillation and ventricular tachycardia on electrocardiogram 2 (September 8, 2022 17:26); G: Electrocardiogram 3 after resuscitation (September 8, 2022 16:35).
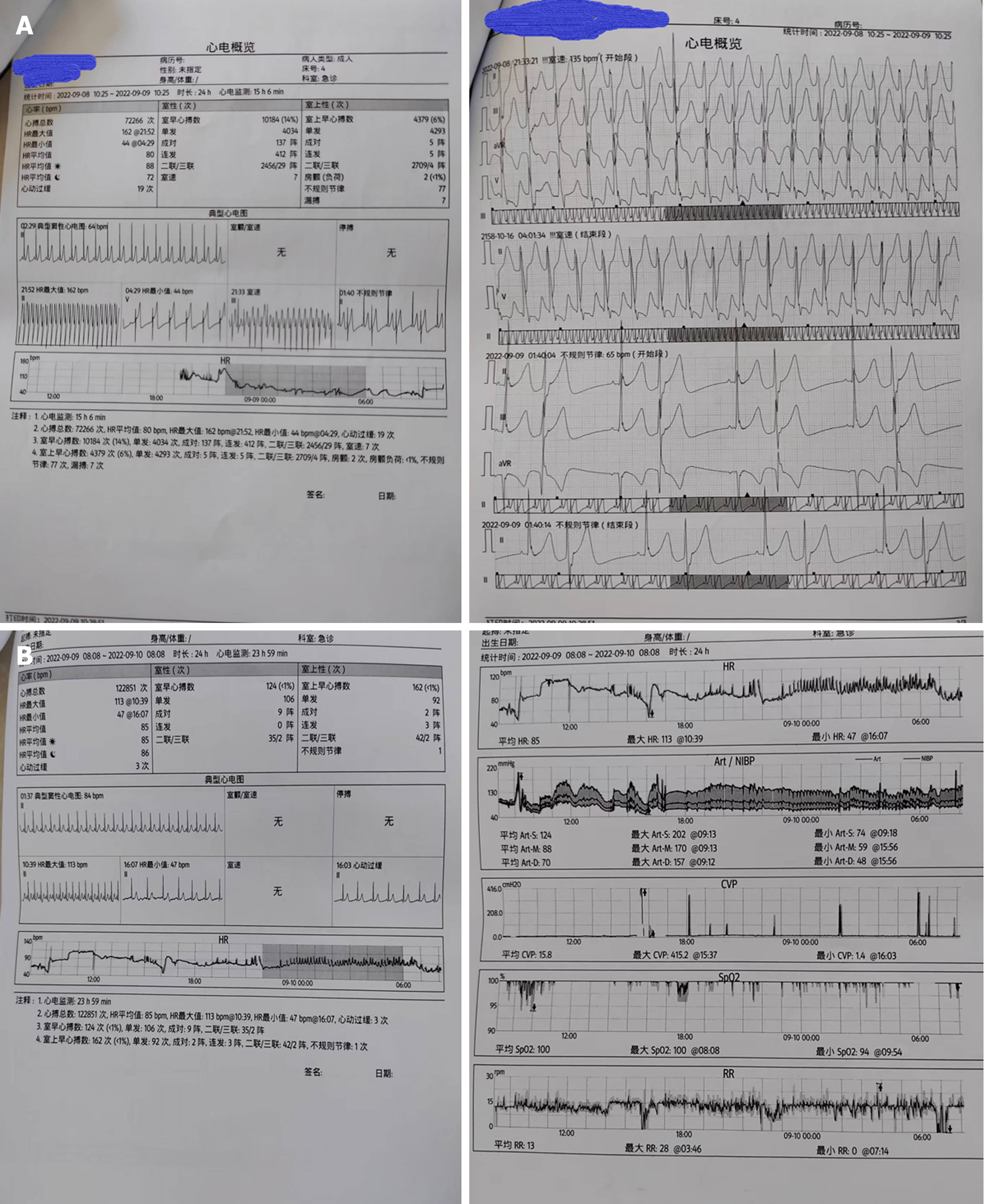
Figure 2 Electrocardiogram overview on days 2-3 and 5-8.
A: An overview of the ECG monitoring: From 19:00 on September 8, 2022 to 8:00 on September 9, 2022, electrocardiogram monitoring for 15 hours, 6 minutes, and 2 seconds. Total number of heartbeats: 72266 times, average heart rate: 80 beats per minute (bpm), maximum heart rate: 162 bpm, minimum heart rate: 44 bpm, tachycardia: 19 times. Ventricular premature beats: 10184 times (14%), single: 4034 times, in pairs: 137 episodes, in triplets: 412 episodes, couplets/triple beats: 2456/29 episodes, ventricular tachycardia: 7 times. Supraventricular premature beats: 4379 times (6%), single: 4293 times, in pairs: 5 episodes, in triplets: 5 episodes, couplets/triple beats: 2709/4 episodes, atrial fibrillation: 2 times, irregular rhythm: 77 times, missed beats: 7 times; B: An overview of the electrocardiogram monitoring: From 8:00 on September 9, 2022 to 8:00 on September 10, 2022, electro
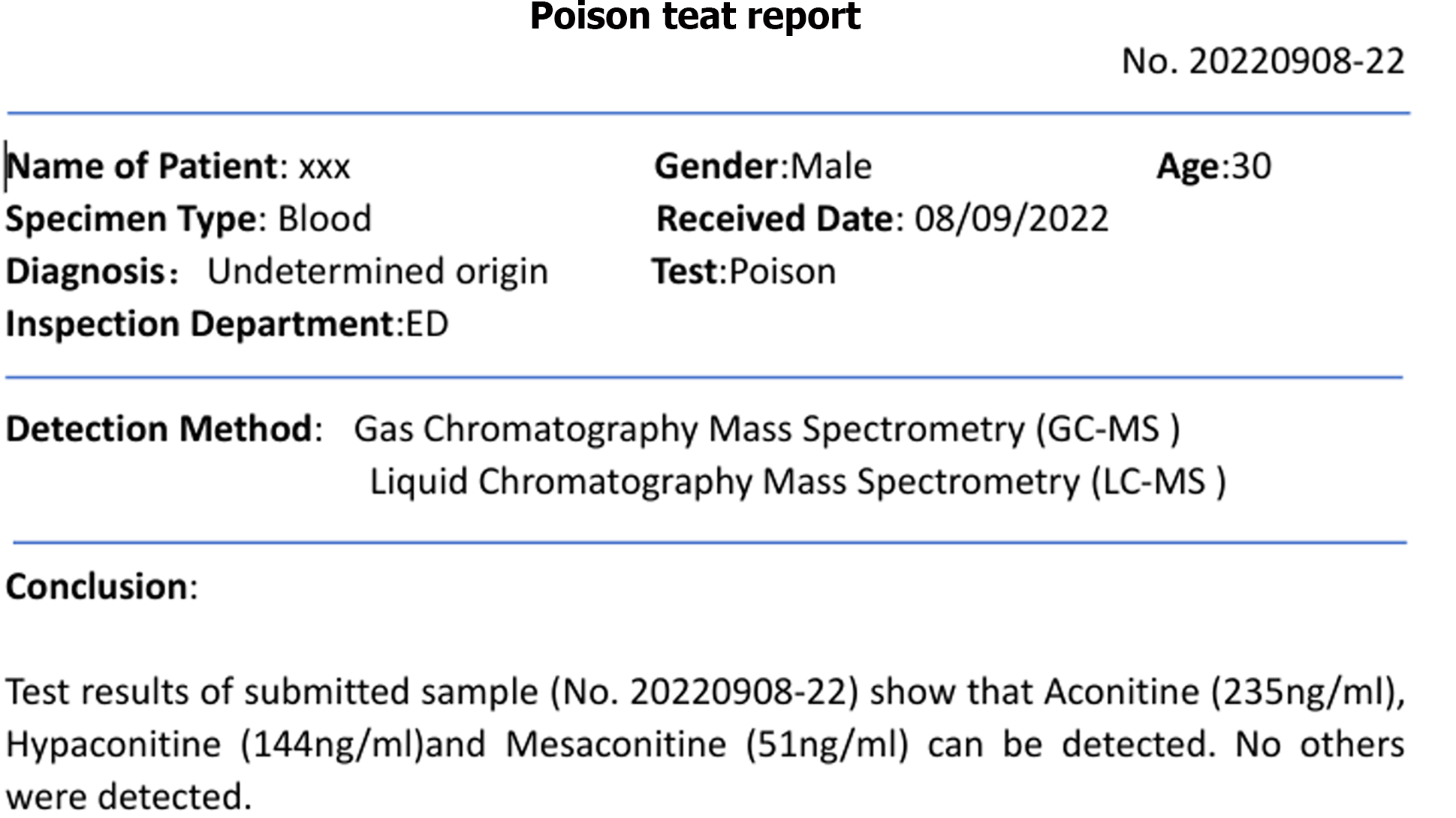
Figure 3 Toxic substance detection report (September 8, 2022).
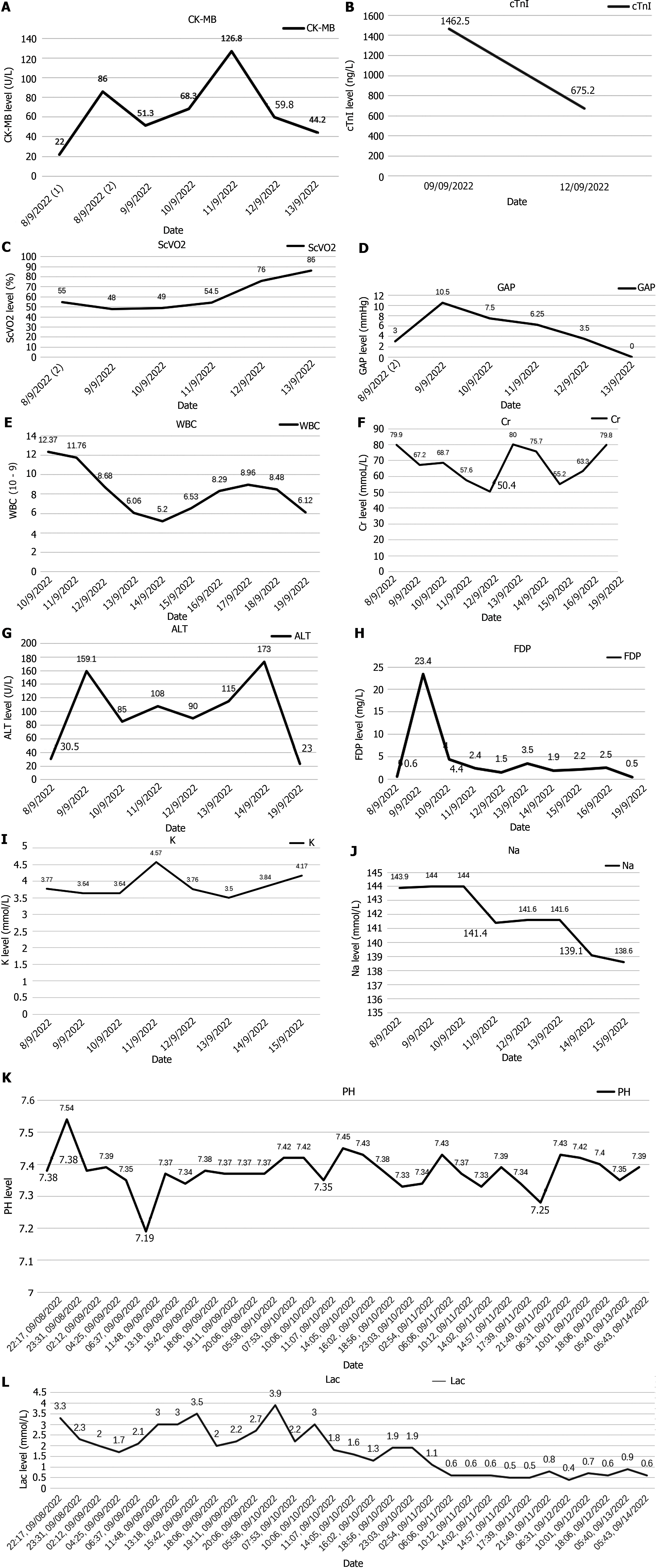
Figure 4 The patient's electrocardiogram and cardiac monitoring changes after entering the hospital.
A: Trend in creatine kinase-MB change. After admission to the hospital, the patient showed an increasing trend in creatine kinase-MB levels, indicating myocardial injury. As the patient's cardiac rhythm stabilized, the levels of cardiac enzymes gradually decreased; B: Trend in cTnI change. After being admitted to the hospital, the patient's elevated cTnI levels indicated myocardial injury. As the patient's cardiac rhythm stabilized, the cTnI levels decreased; C: Trend in Central venous oxygen saturation (ScVO2) change. The patient's ScVO2 was low in the early stages, and as the cardiac function gradually stabilized, the ScVO2 levels gradually increased; D: Trend in venoarterial carbon dioxide partial pressure difference change. The patient's glycated albumin levels gradually decreased as cardiac rhythm and function recovered; E: Trend in white blood cell (WBC) count change. The patient's WBC count gradually decreased with the change in the stress state; F: Trend in creatinine (Cr) change. The patient's Cr levels gradually decreased with early support from continuous renal replacement therapy (CRRT) and extracorporeal membrane oxygenation. After the gradual withdrawal of life support and blood purification equipment, the Cr levels rebounded. At the time of discharge, the patient's Cr levels were stable at an increased level; G: Trend in alanine aminotransferase change. The patient's transaminase levels gradually decreased after the stabilization of cardiac function, and on the 14th day, the transaminase levels increased without treatment but returned to normal on their own; H: Trend in fibrin (ogen) degradation products (FDP) change. The patient's FDP levels showed a significant increase on the 9th. Subsequently, with the adjustment of anticoagulation strategies, extracorporeal membrane oxygenation support, and the gradual stabilization of cardiac function, the patient's FDP levels gradually decreased to normal levels; I: Trend in serum potassium (K) change. The patient’s K levels have remained stable; J: Trend in serum sodium (Na) change. The patient’s Na levels have remained stable; K: Trend in potential of hydrogen (pH) change. The patient exhibited an excessively high pH on the 8th due to the administration of sodium bicarbonate to correct acidosis during cardiopulmonary resuscitation. On the morning of the 9th, a drop in pH was observed following a cardiac arrest. After adjusting the CRRT alkali supplementation strategy, the pH has been consistently maintained above 7.35, and the patient did not experience prolonged acidosis; L: Trend in lactic acid (Lac) change. The patient's Lac levels were relatively stable after extracorporeal membrane oxygenation treatment. However, there were fluctuations in lactate levels during the sympathetic storm events that occurred repeatedly from the 8th to the 10th. As the patient's cardiac function and rhythm gradually stabilized after the 10th, the patient's lactate levels gradually decreased. cTnl: cTnI change; ScVO2: Central venous oxygen saturation; GAP: Glycated Albumin; WBC: White blood cell; Cr: Creatinine; ALT: Alanine aminotransferase; FDP: Fibrin (ogen) Degradation Products; K: Serum potassium; Na: Serum sodium; Lac: Lactic acid; pH: Potential of Hydrogen.
- Citation: Bian YY, Hou J, Khakurel S. Treatment of a patient with aconitine poisoning using veno-arterial membrane oxygenation: A case report. World J Clin Cases 2024; 12(21): 4842-4852
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4842.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4842