Copyright
©The Author(s) 2023.
World J Clin Cases. Feb 26, 2023; 11(6): 1299-1309
Published online Feb 26, 2023. doi: 10.12998/wjcc.v11.i6.1299
Published online Feb 26, 2023. doi: 10.12998/wjcc.v11.i6.1299
Figure 1 Clinical mandibular advancement appliance as worn by patients.
A: Right interoral occlusion; B: Frontal interoral occlusion; C: Left interoral occlusion.
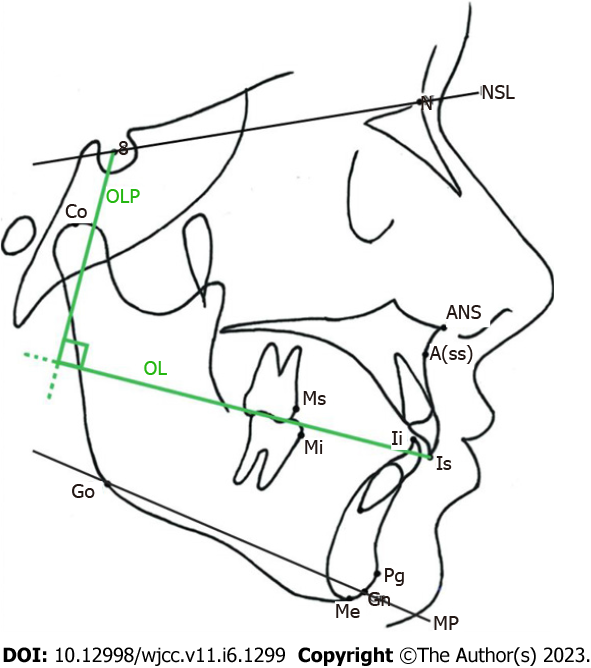
Figure 2 Mark points and reference planes of cephalometric measurement by Pancherz analysis.
S: Sella; N: Nasion; NSL: SN plane, the line connecting the S point and N point; ANS: Anterior nasal spine; Co: Condylion; OL: Occlusal line; OLP: Occlusal line perpendicular; Ms: Molar superius; Mi: Molar inferius; Ii: Incision inferius; Is: Incision superius; Pg: Pogonion; Me: Menton; Gn: Gnathion; Go: Gonion; A(ss): A.subspinale; MP: MP plane, the line connecting the gonion point and gnathion point.
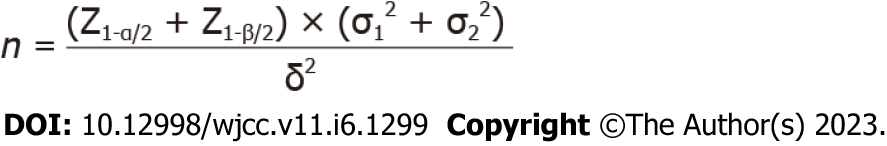
Figure 3 Formula for calculating sample size.
In the formula: Z1-α/2 = 1.96, Z1-β/2 = 0.84; σ1 = 3.25; σ2 = 4.53, δ = 72.55-75.68.
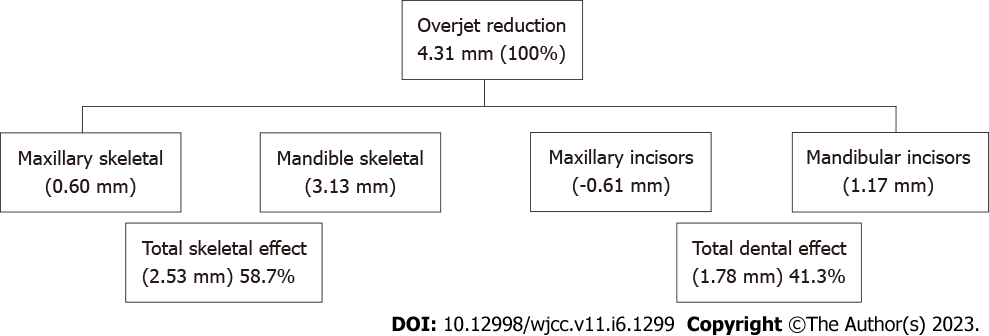
Figure 4 Changes in coverage relationship and proportion of dental and skeletal effect after mandibular advancement treatment.
According to calculation and measurement, the proportion of skeletal factors in the total sagittal displacement overjet is 58.7%, the proportion of dental factors is 41.3%. Minus (“-”) indicates the position moves backward, positive value indicates the position moves forward.
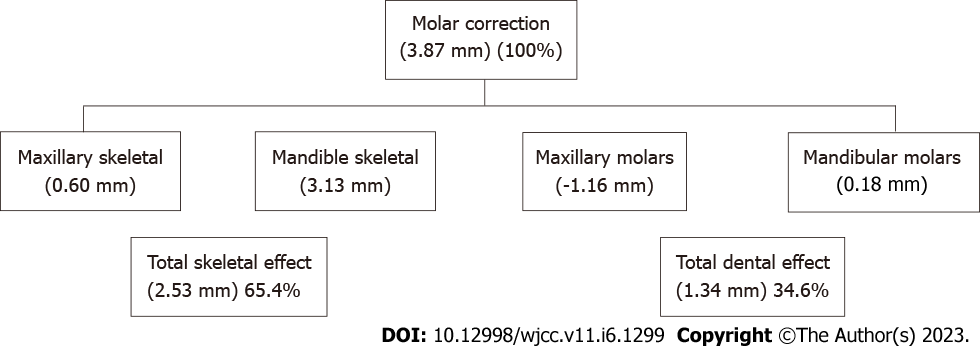
Figure 5 Molar relationship changes and the proportion of dental and skeletal effect after mandibular advancement treatment.
According to calculation and measurement, the proportion of skeletal factors in the total sagittal displacement molar correction is 65.4%, the proportion of dental factors is 34.6%.
- Citation: Kong L, Liu XQ. Efficacy of invisible advancement correction for mandibular retraction in adolescents based on Pancherz analysis. World J Clin Cases 2023; 11(6): 1299-1309
- URL: https://www.wjgnet.com/2307-8960/full/v11/i6/1299.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i6.1299