Copyright
©The Author(s) 2023.
World J Clin Cases. Dec 6, 2023; 11(34): 8235-8241
Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8235
Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8235
Figure 1 Magnetic resonance cholangiopancreatography.
A complete obstruction was observed from the right intrahepatic bile duct to the common hepatic duct segment with upstream dilatation of the biliary trees.
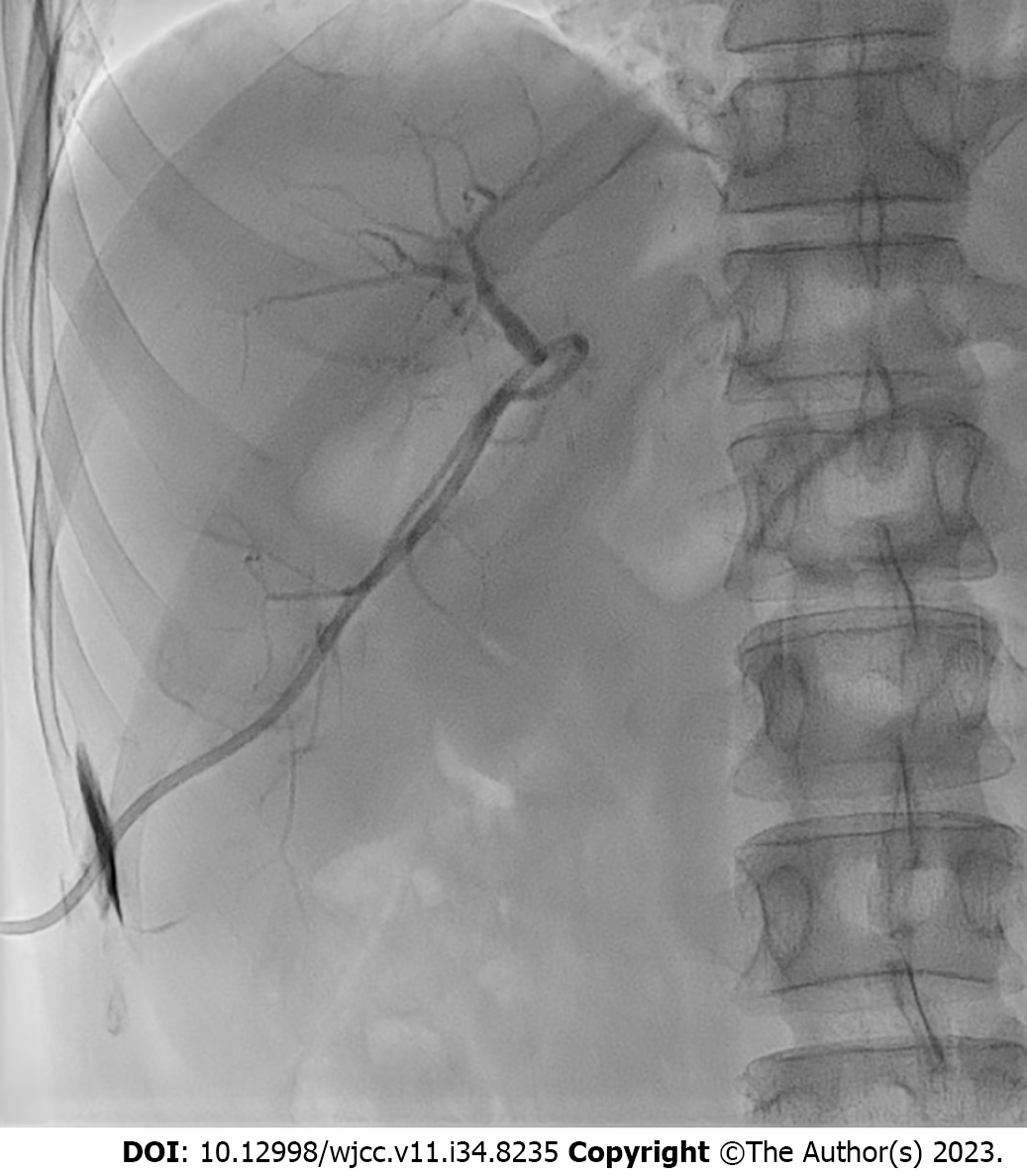
Figure 2 Percutaneous transhepatic biliary drainage.
An obstruction was observed at the confluence of the right intrahepatic bile duct (IHBD). However, the guidewire could not pass through the obstruction. An 8.5 Fr catheter was placed in the right IHBD.
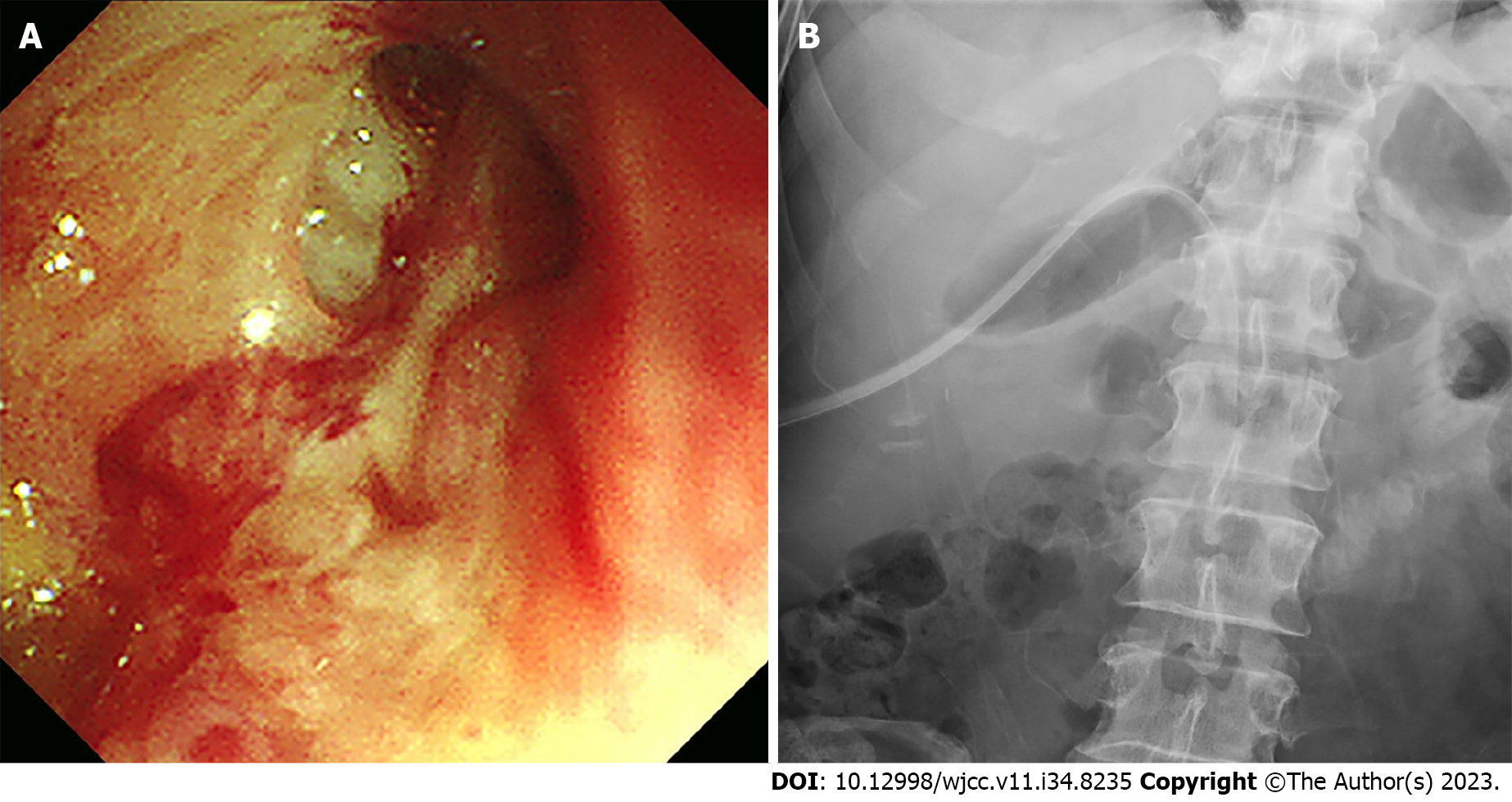
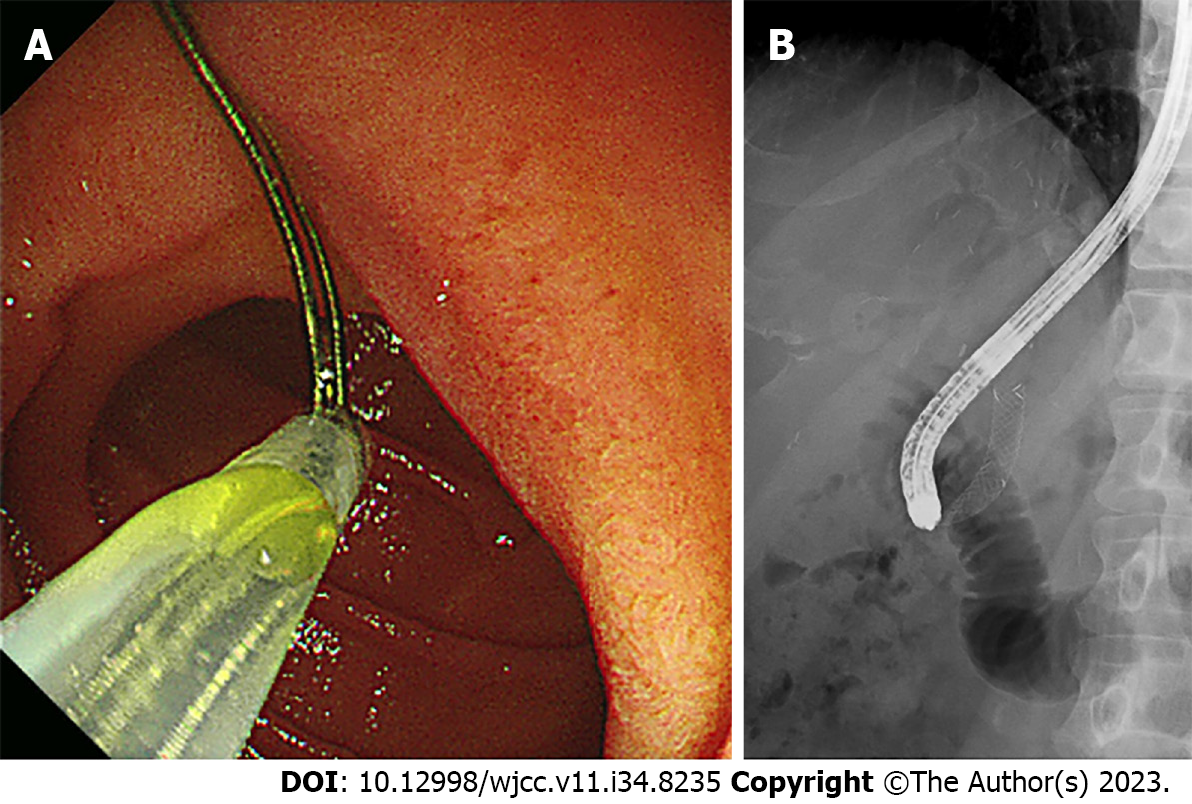
Figure 3 Percutaneous transhepatic cholangioscopy.
A: The slit-like orifice of the right intrahepatic bile duct stricture was detected using percutaneous transhepatic cholangioscopy (PTCS); B: An 18 Fr PTCS catheter was successfully inserted.
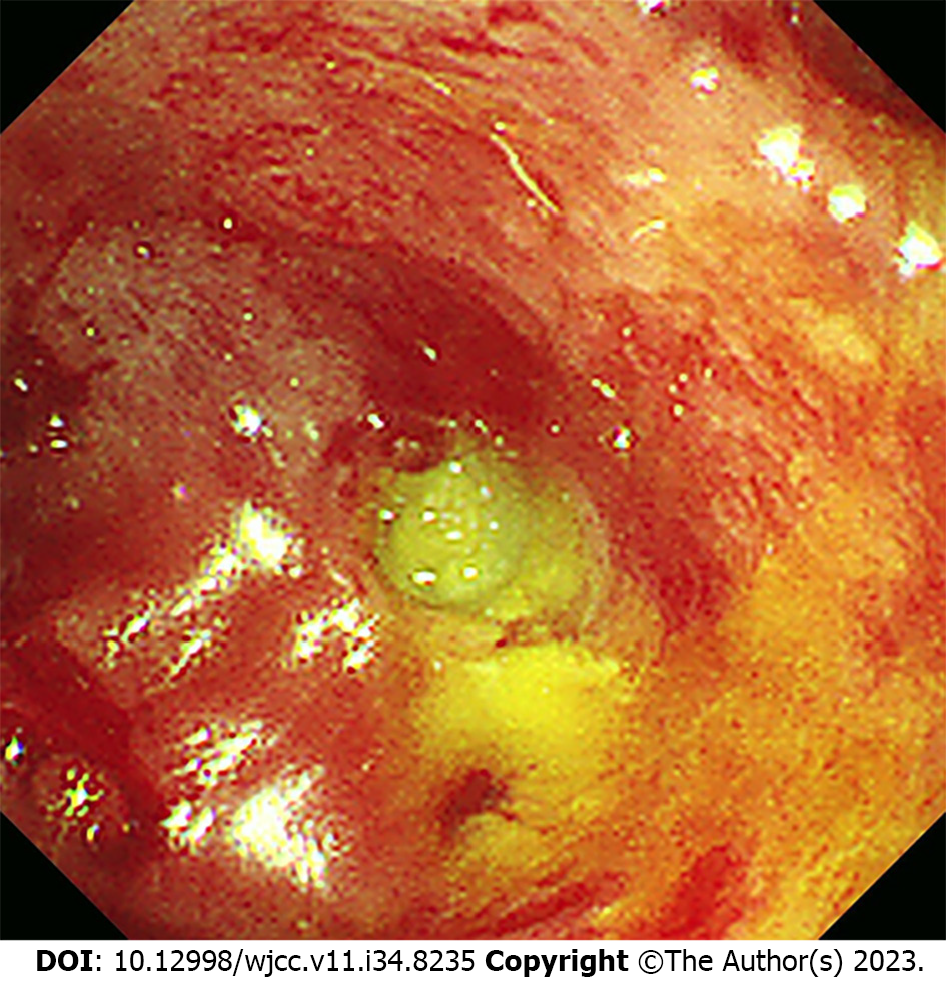
Figure 4 Follow-up percutaneous transhepatic cholangioscopy.
Subsequent cholangioscopy after catheter dislocation displayed almost complete occlusion of the stricture orifice.
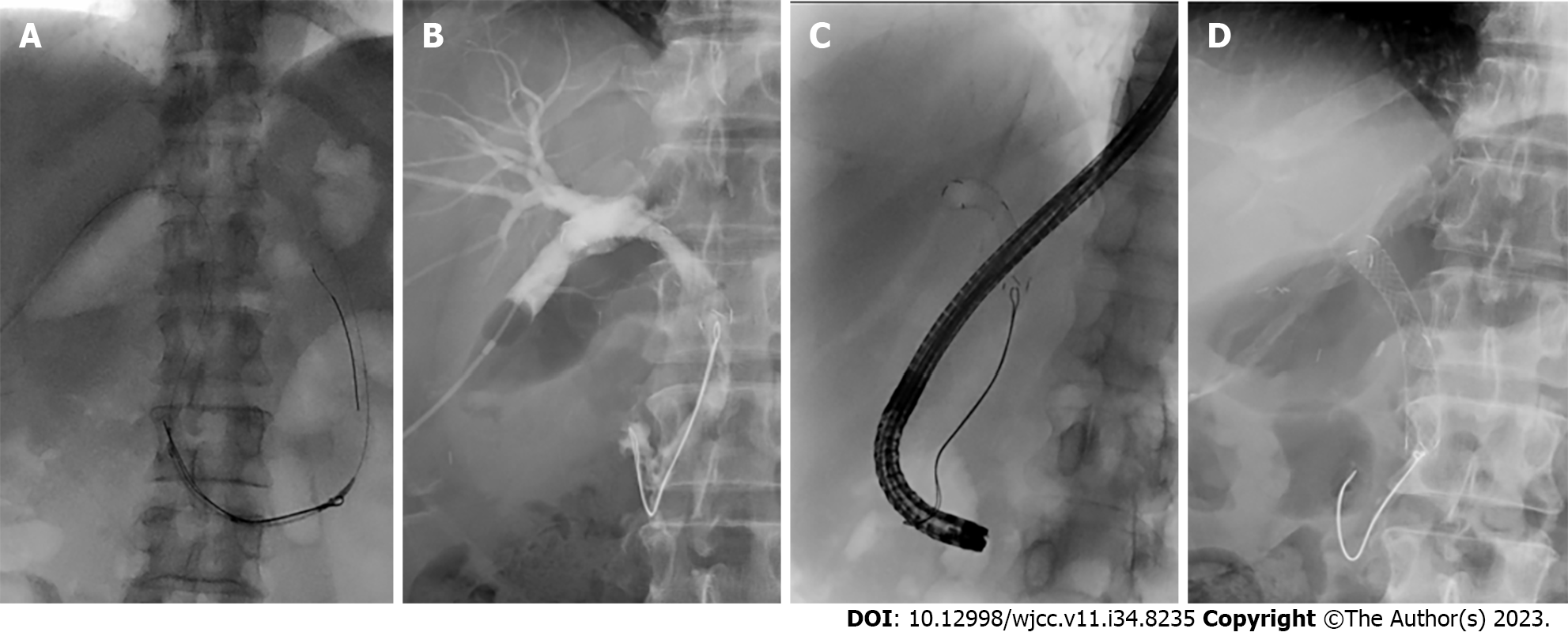
Figure 5 Insertion process of an inverted metallic stent.
A: An inverted metallic stent was pushed sufficiently to allow the string to spread well into the duodenal lumen; B: The first branches of the right intrahepatic bile duct were blocked by the stent end; C: The string was captured using a snare through a gastroscope and pulled carefully; D: Finally, the metallic stent was properly placed into the stricture without peripheral bile duct obstruction.
Figure 6 Removal of the metallic stent.
A: The retrieved string was captured through a forward-viewing gastroscope with a snare; B: And then, the stent was slowly pulled into the stricture site while the position and orientation of the string were maintained.
- Citation: Lee Y, Park CH, Cho E, Kim KH. Management of post-liver transplantation biliary stricture inaccessible by endoscopic retrograde cholangiopancreatography: A case report. World J Clin Cases 2023; 11(34): 8235-8241
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8235.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8235