Copyright
©The Author(s) 2023.
World J Clin Cases. Sep 16, 2023; 11(26): 6252-6261
Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6252
Published online Sep 16, 2023. doi: 10.12998/wjcc.v11.i26.6252
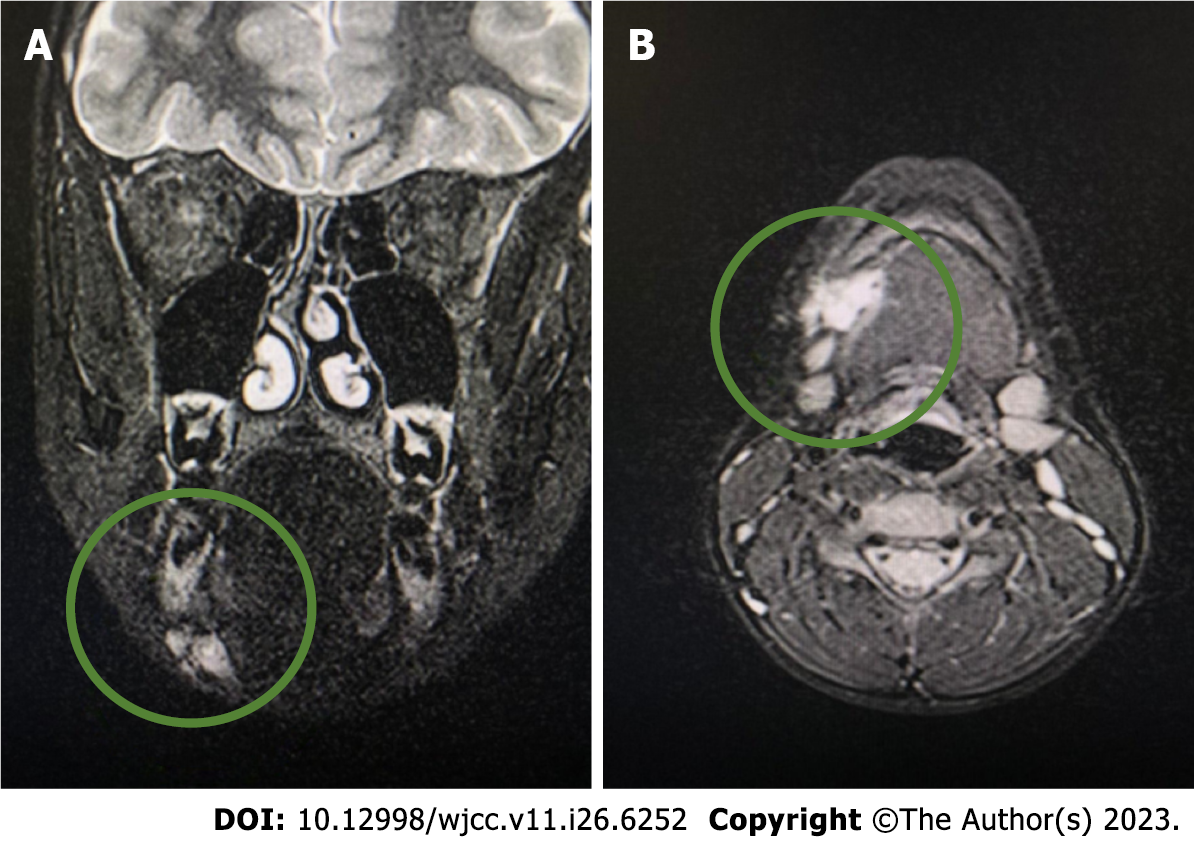
Figure 1 Computed tomography.
A: Focal change on the right side of the submandibular space initially diagnosed as a venous malformation; B: Visible irregular outline of a moderately hyperintense area of 18 mm × 25 mm × 13 mm.
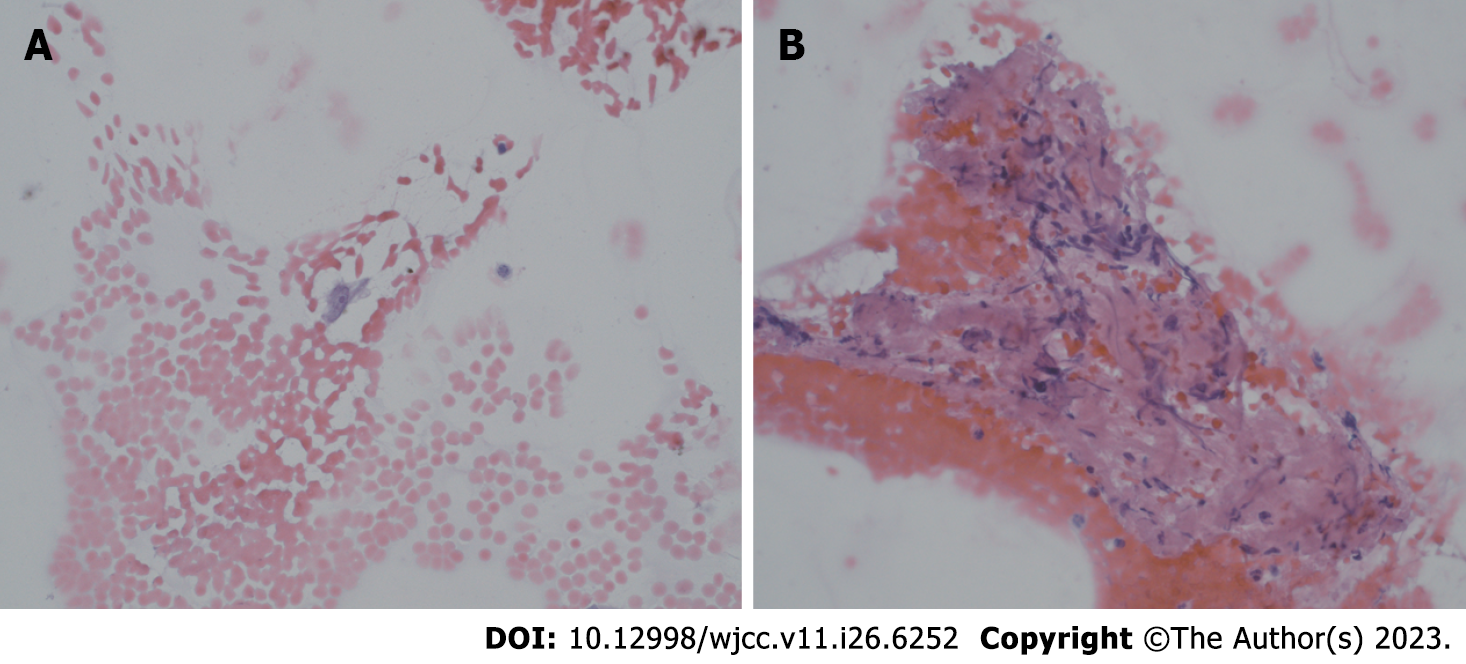
Figure 2 Fine needle aspiration at high magnification (400 ×, hematoxylin and eosin staining).
A: Single bland cell with oval nucleus, smooth nuclear membranes, and conspicuous nucleolus; B: Spindle bland cells within an eosinophilic background.
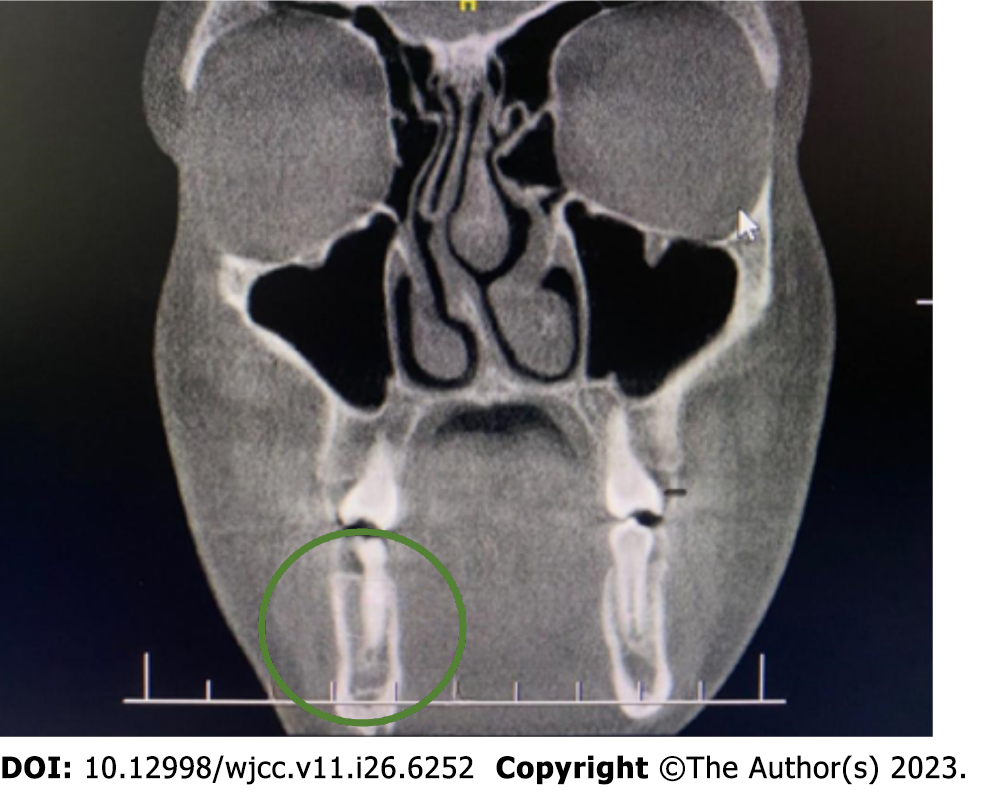
Figure 3 A smooth contoured 3 mm defect in the cortical layer of the inner mandible on the right side near the border of the scan.
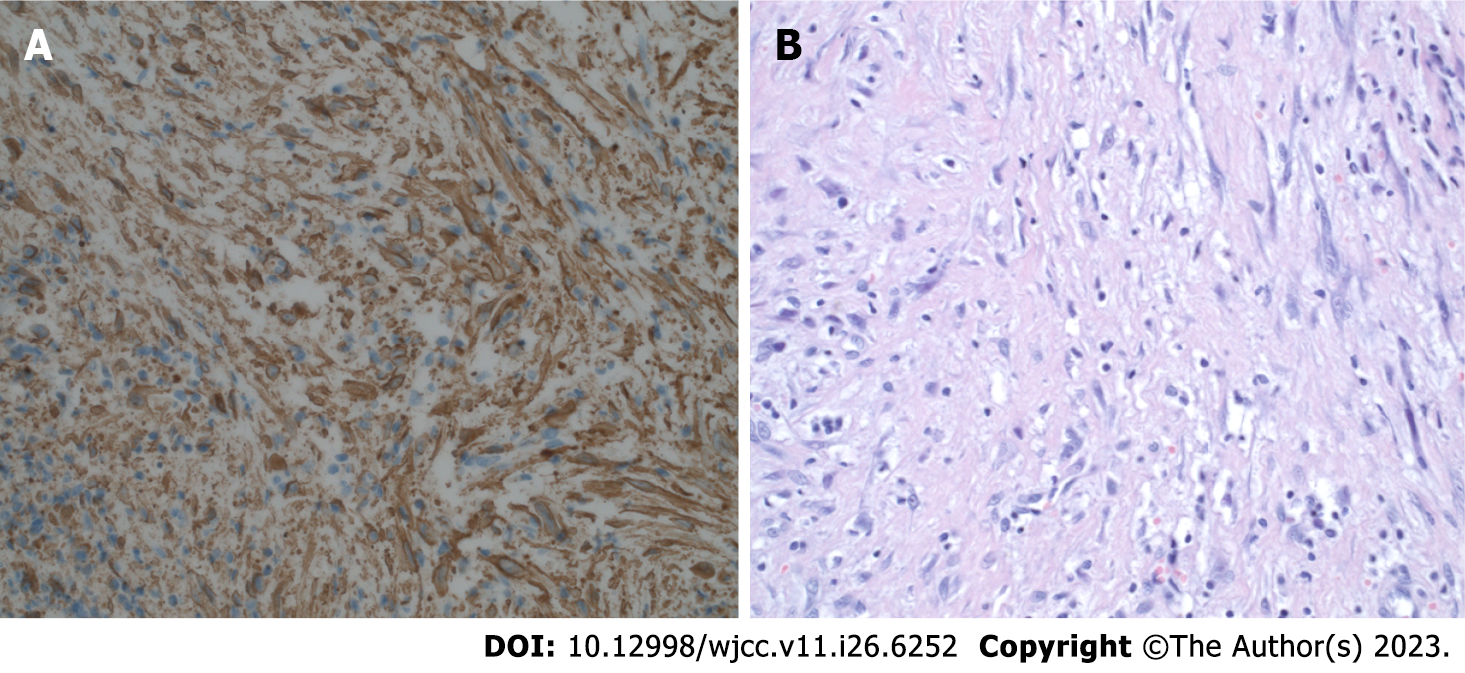
Figure 4 Histopathological diagnosis.
A: Diffuse expression of smooth muscle actin. Excision, magnification 400 ×; B: Excision (400 ×, hematoxylin and eosin staining). Short spindled myoid and ovoid, histiocyte-like cells within a somewhat myxoid background.
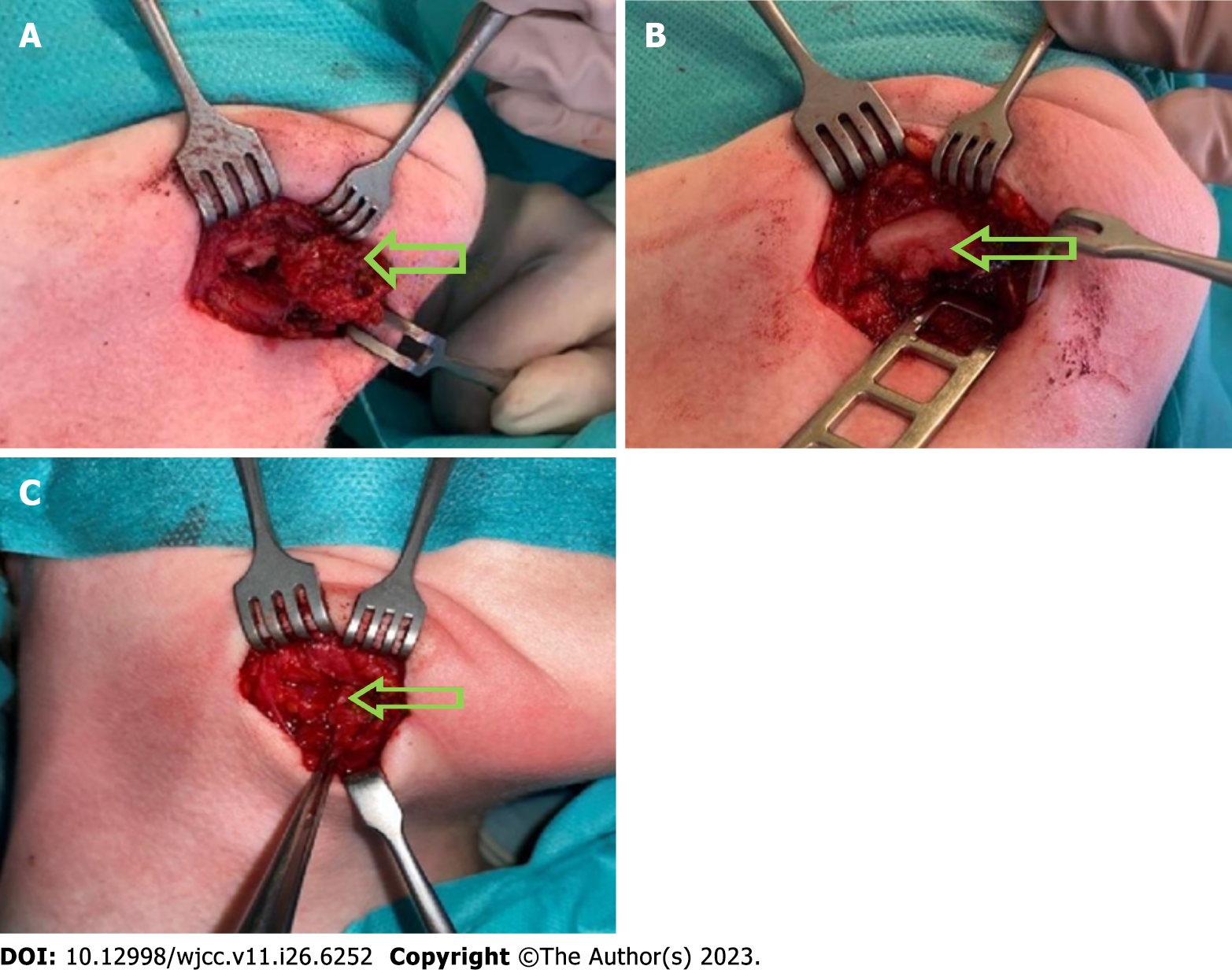
Figure 5 Intraoperative picture.
A: Intraoperative picture of submandibular, angiomatoid fibrous histiocytoma, tumor is marked with an arrow; B: Intraoperative picture of a destroyed external layer of the mandible, it is marked with an arrow; C: Intraoperative view of the second procedure, no AFH irregularities were found. Tissue scar are marked with arrows.
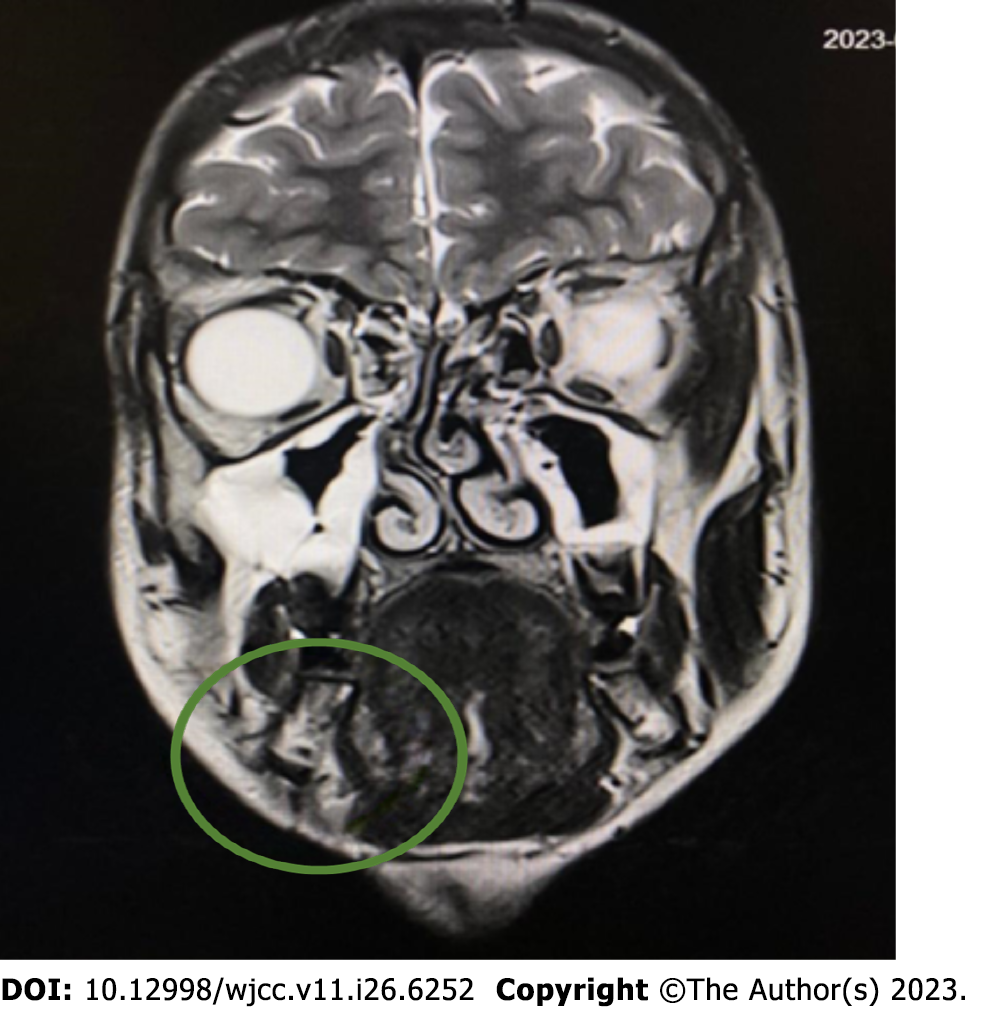
Figure 6 Magnetic resonance imaging before second surgical procedure.
Just below the outline of the body of the mandible, a lesion suspected of a residual tumor mass of 4 mm × 8 mm × 4 mm is visible.
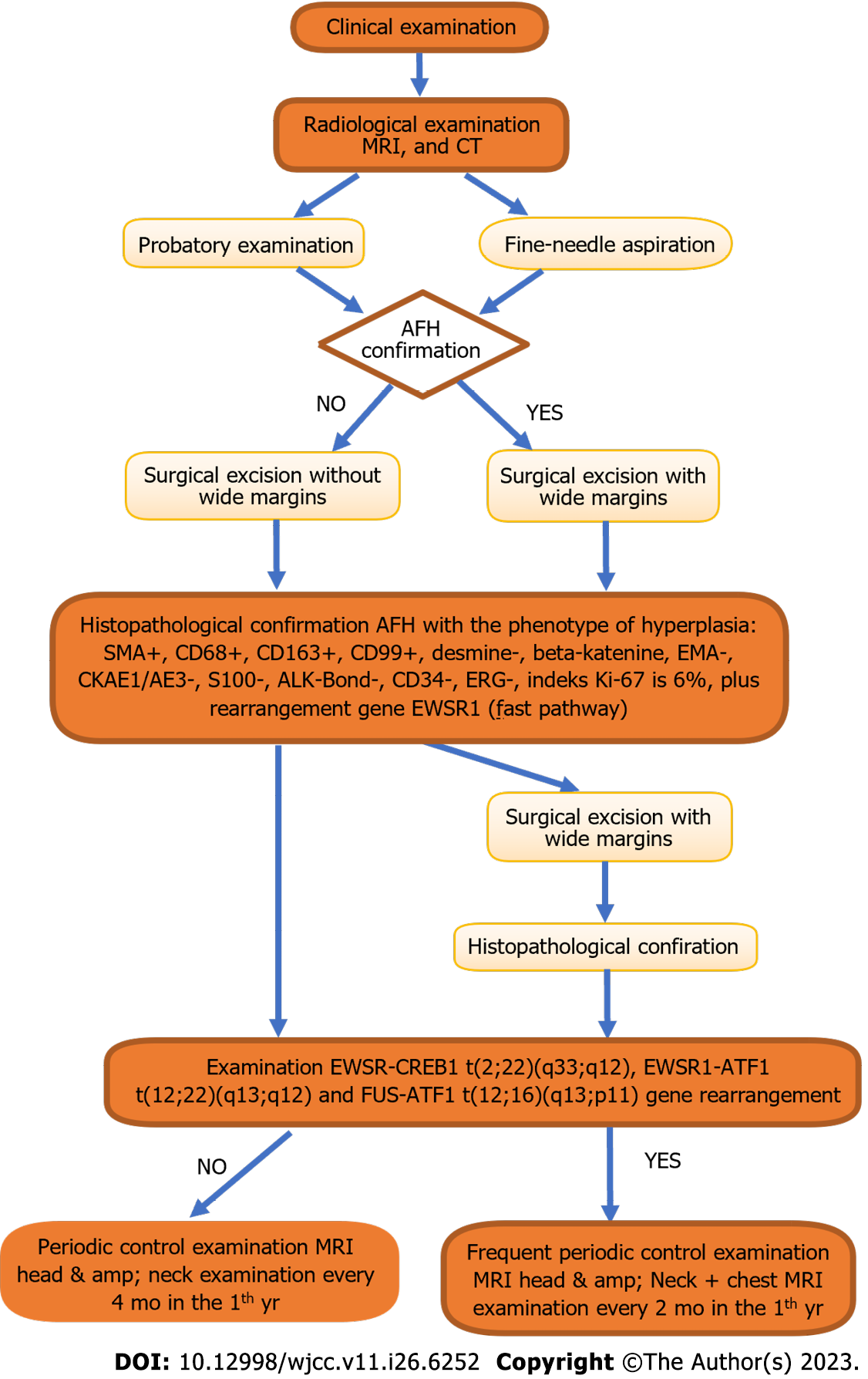
Figure 7 Proposed diagnostic and therapeutic path.
AFH: Angiomatoid fibrous histiocytoma; CT: Computed tomography MRI: Magnetic resonance imaging.
- Citation: Michcik A, Bień M, Wojciechowska B, Polcyn A, Garbacewicz Ł, Kowalski J, Drogoszewska B. Difficulties in diagnosing angiomatoid fibrous histiocytoma of the head and neck region: A case report. World J Clin Cases 2023; 11(26): 6252-6261
- URL: https://www.wjgnet.com/2307-8960/full/v11/i26/6252.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i26.6252