Copyright
©The Author(s) 2023.
World J Clin Cases. Sep 6, 2023; 11(25): 5954-5961
Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.5954
Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.5954
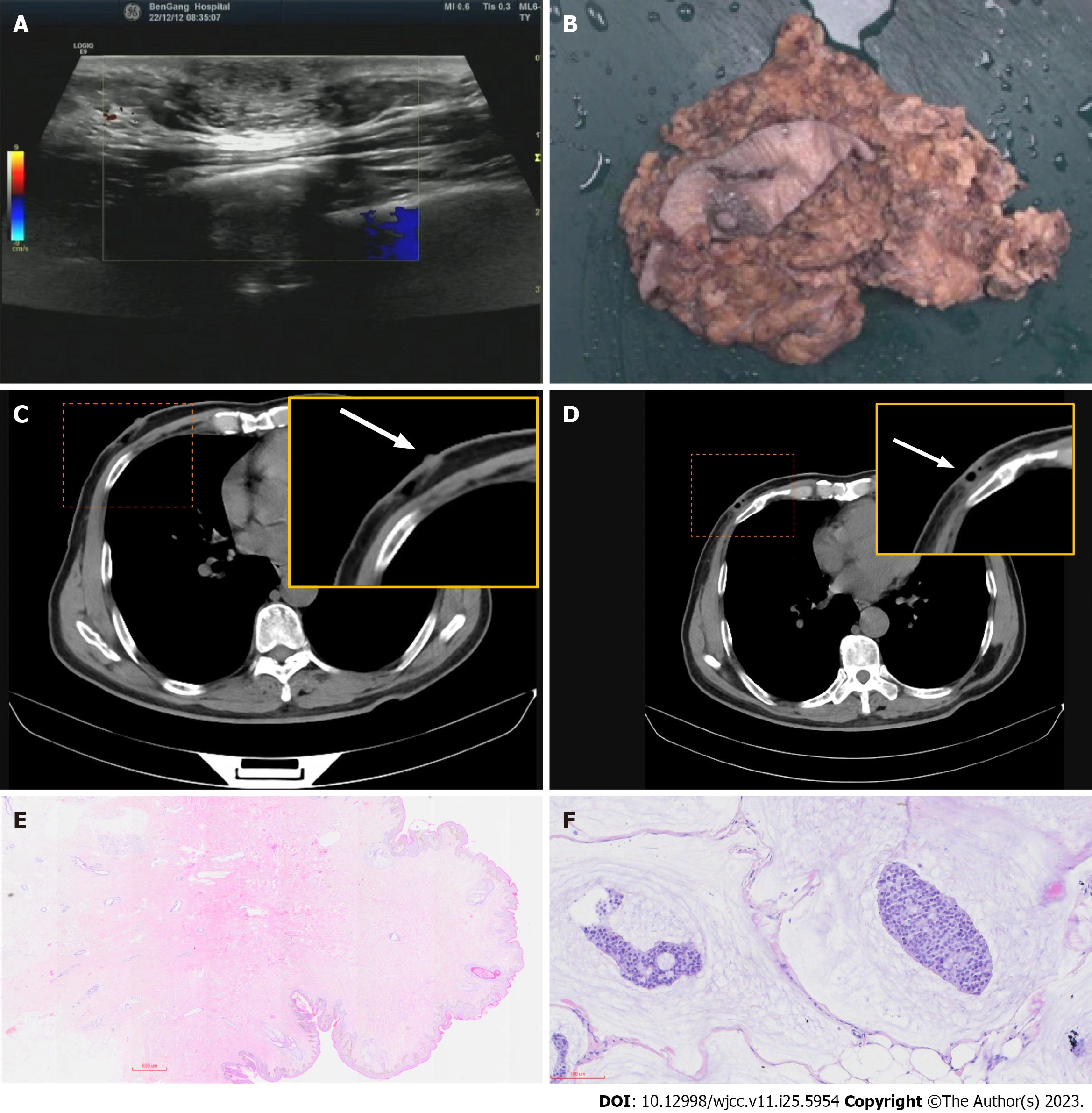
Figure 1 Preoperative and postoperative imaging corresponding surgical specimen and pathology analysis.
A: Ultrasound image of the left breast region at the upper outer area of the nipple demonstrating a 1.88-cm oval, parallel isoechoic mass; B: Surgical specimens showing the position of the surgical scar; C: Computerized tomography reveals posterior nipple glands (the arrow points to the position where the back of the nipple is located); D: Postoperative defects from outpatient surgery (the arrow points to the location of the residual cavity after removal of the mass); E: Histopathological examination of the excised breast tissue showing a nodular lesion with relatively clear borders in the breast. Homogeneous clusters of tumor cells containing small nuclei together with slightly larger round nuclei were suspended in abundant mucus material (mucus lake). The tumor invaded the surrounding adipose tissue and muscle tissue and did not invade the skin or subcutaneous tissue. The ductal tissue of the breast was visible in the periphery, and no intraductal cancer changes were seen (hematoxylin-eosin, 200 ×); F: Pathology of the nipple and posterior nipple, and no cancerous tissue invasion was seen in the nipple and subpapillary ducts, and Paget’s changes were not seen in the skin (hematoxylin-eosin, 20 ×).
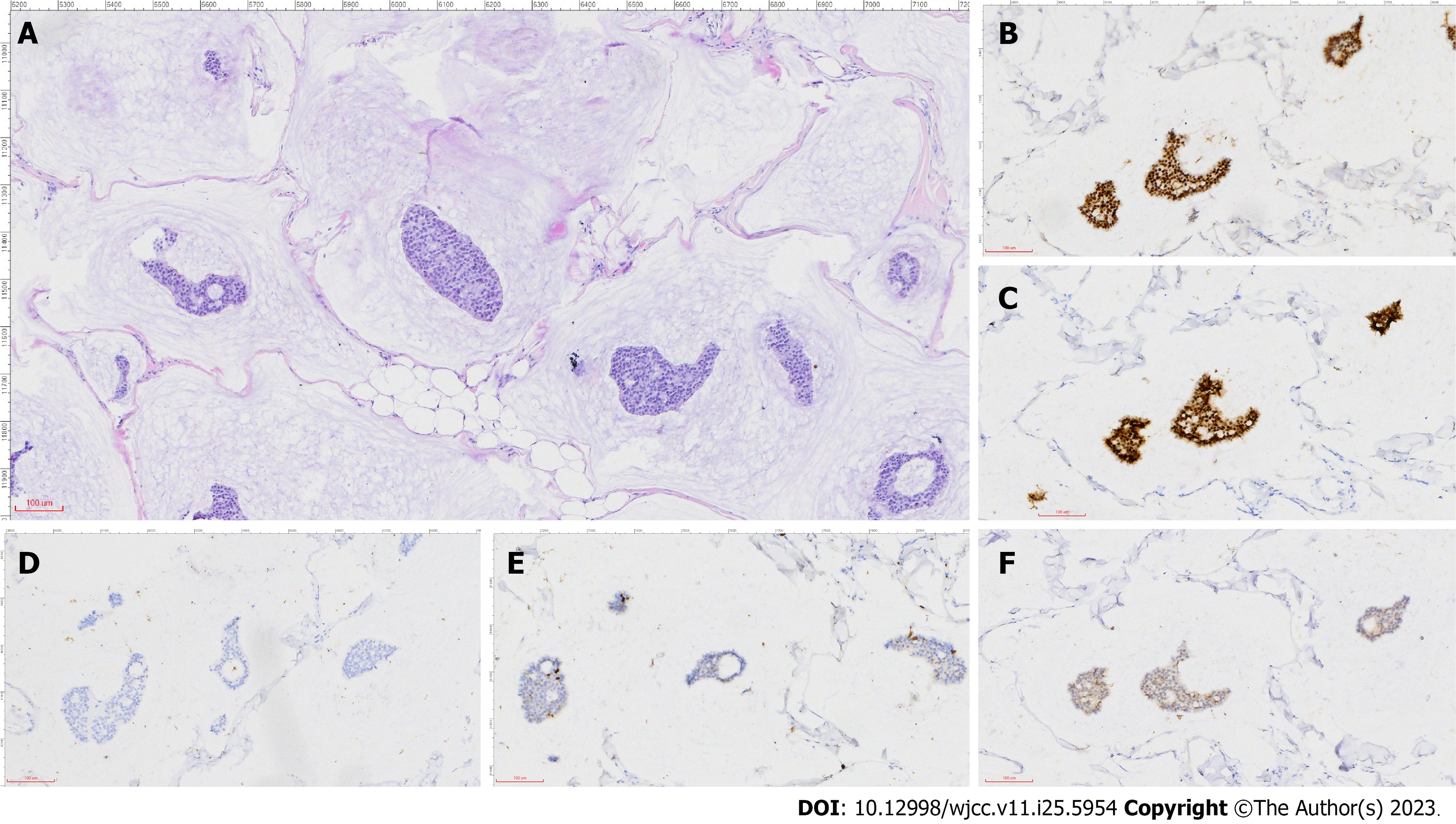
Figure 2 Pathology and immunohistochemistry analysis.
A: Image showing clusters of tumor cells suspended in abundant extracellular mucin and separated by ciliated fibrous intervals containing capillaries; B: Estrogen receptor (2+); C: Progesterone receptor (2+); D: AR (−); E: Ki-67 (5%); F: CerbB-2 (−) (scale: 100 μm; 200 ×).
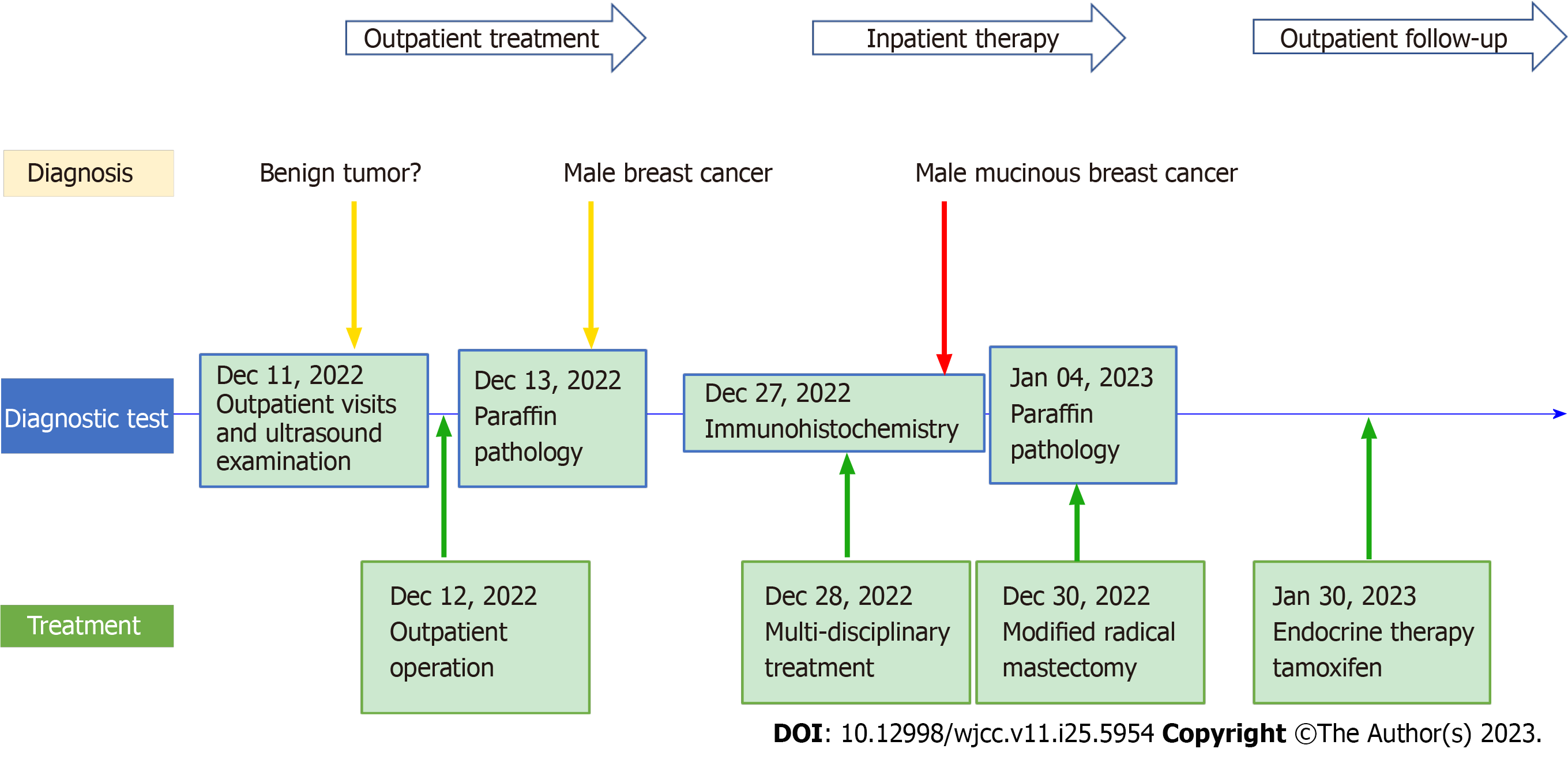
Figure 3 Timeline of disease course.
- Citation: Sun Q, Liu XY, Zhang Q, Jiang H. Non-retroareolar male mucinous breast cancer without gynecomastia development in an elderly man: A case report. World J Clin Cases 2023; 11(25): 5954-5961
- URL: https://www.wjgnet.com/2307-8960/full/v11/i25/5954.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i25.5954