Copyright
©The Author(s) 2023.
World J Clin Cases. Jul 6, 2023; 11(19): 4458-4476
Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4458
Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4458
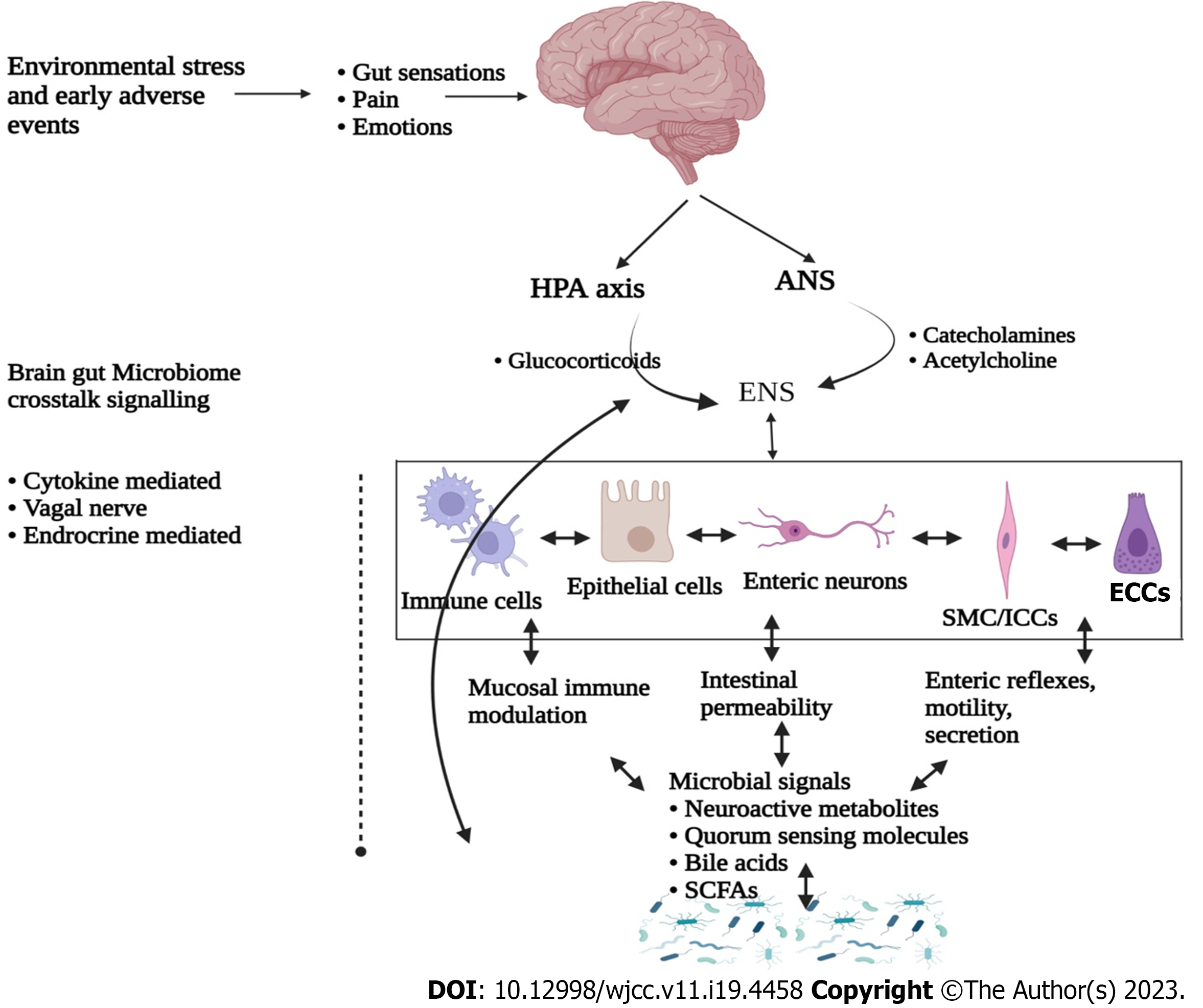
Figure 1 Regulatory cross talk between gut and brain.
The central nervous system and enteric nervous system mainly communicate through vagal and autonomic pathways to control various gastrointestinal functions in a bidirectional approach. These signalling cascades are also regulated through mood and cognitive processes and significantly affected by environmental factors and early adverse events. These signalling crosstalks are significantly altered in irritative bowel syndrome (IBS) thus resulting in abnormal gastrointestinal motility, visceral hypersensitivity and bowel movements. Perturbations in the gut microbiome composition and diversity through various sources alter this cross talk, thus resulting in interceptive feedback to brain and causing functional and neuroplastic changes. Microbial metabolites released from various microbial populations have critical role in these crosstalks, thus having therapeutic values for the management of IBS. ANS: Autonomic nervous system; HPA: Hypothalamic-pituitary-adrenal axis; ECC: Enterochromaffin cells; ICC: Interstitial cells of Cajal; SMC: Smooth muscle cells; SCFAs: Short chain fatty acids; ENS: Enteric nervous system.
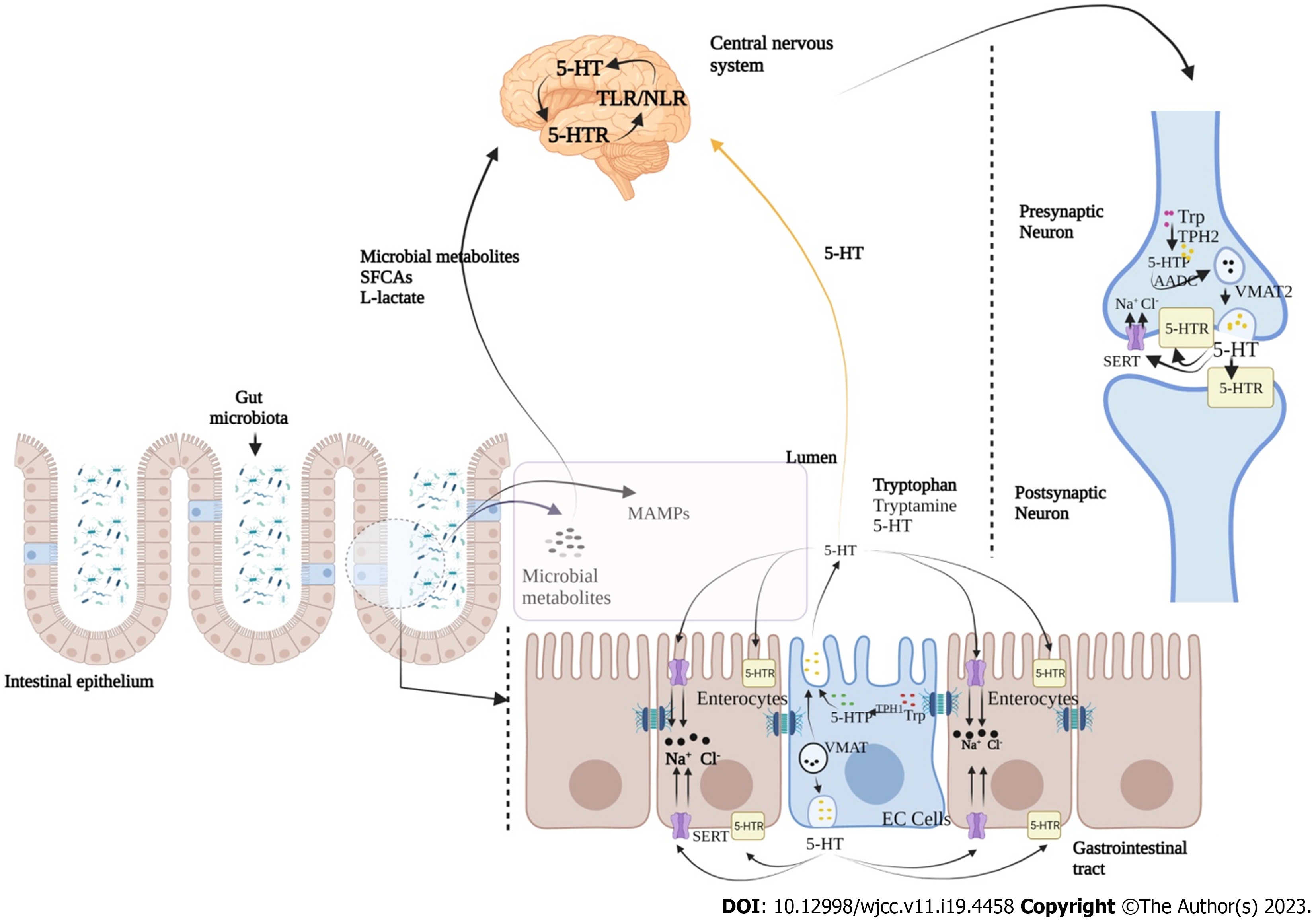
Figure 2 Serotonin mediated bidirectional cross talk between gut microbiota and brain.
Serotonin (5-HT) plays a key role in microbiota-gut-brain communications to modulate gastrointestinal (GI) and central nervous system (CNS) functions. Serotonin action is mediated through various signalling mechanisms between 5-HT receptors located in postsynaptic and presynaptic neurons at CNS and intestinal serotonergic neurons, and in different cell types of GI tract. Serotonin is synthesized by enterochromaffin cells (EC) in the gut and serotonergic neurons in the CNS. Microbial associated molecular patterns from microbiota directly affect the serotonergic system, mainly through modulating the activity and expression of serotonin transporter (SERT) and serotonin receptors (5-HTRs), as well as the synthesis of 5-HT in GI tract. Stored into vesicles forms through the vesicular monoamine transporter (VMAT; VMAT1 in EC cells and VMAT2 in neurons), 5-HT is further released into the extracellular space where its binds to different serotonin receptors (5-HTR). At the same place taken up by the neurons, enterocytes or platelets through the SERT limit the 5-HT mediated signalling crosstalk. 5-HT: 5-Hydroxytryptamine; TLR: Toll-like receptors; NLR: NOD-like receptors; SFCA: Short-chain fatty acids; MAMP: Molecular patterns from microbiota; SERT: Serotonin transporter; VMAT: Vesicular monoamine transporter.
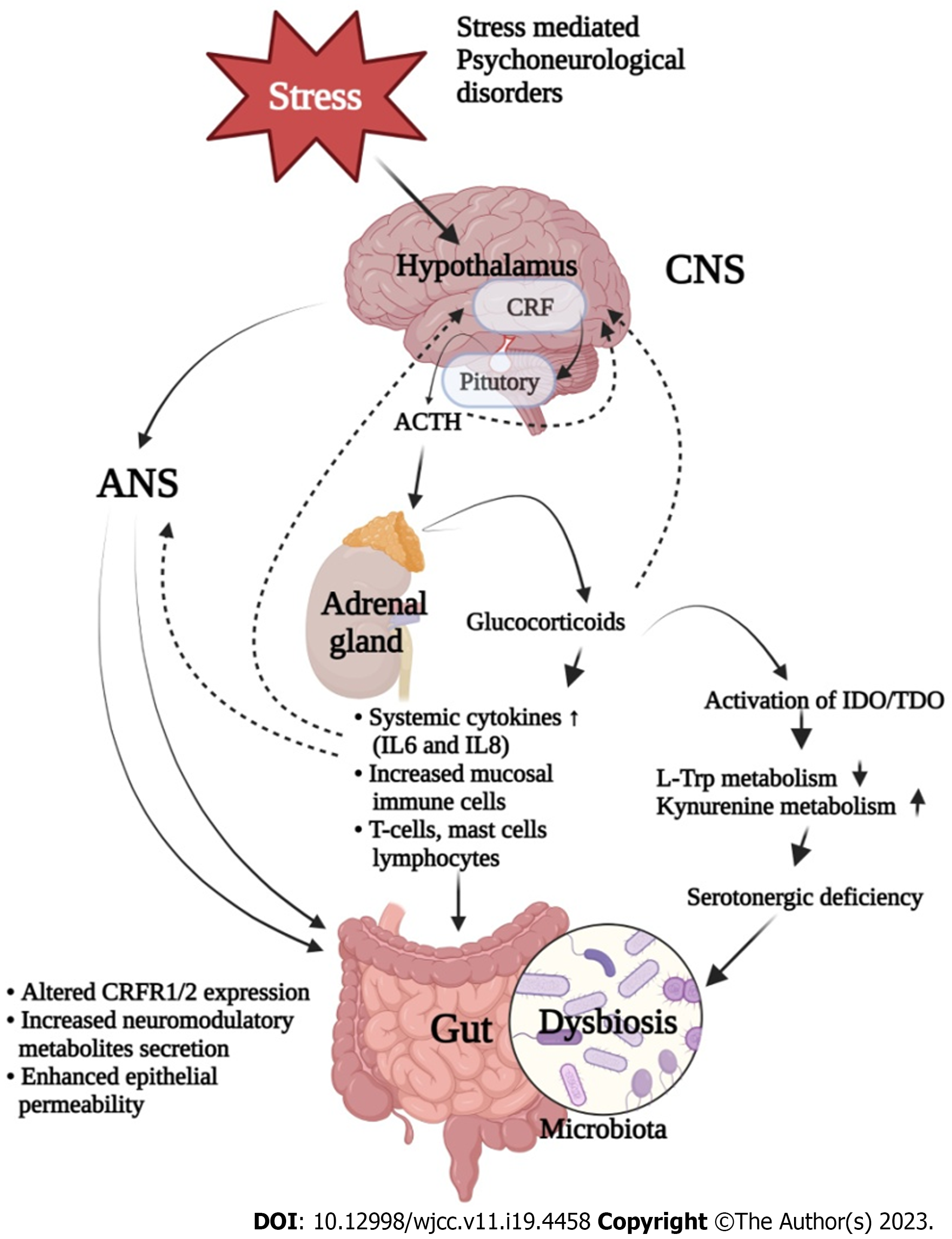
Figure 3 Impact of stress on irritable bowel syndrome.
A bidirectional signalling has been identified between brain and gut, under stress condition in irritable bowel syndrome (IBS). Stress induces the activation of hypothalamic-pituitary-adrenal axis which results in the release of various stress factors such as corticotropin-releasing factor from hypothalamus, thus causing the release of glucocorticoids from adrenal glands. This collectively alters bowel function and stimulates the upregulation of immune system, which directly or indirectly regulates gut function. In addition to this, stress also modulates the tryptophan metabolism by up-regulating kynurenine pathway which generates neurotoxic and neuroprotective metabolites. Enzymes responsible for the degradation of tryptophan are significantly affected by immune pathways (indoleamine-2,3-dioxygenase) and stress levels (tryptophan-2,3-dioxygenase). Under stressed conditions and due to excess availability of kynurenine and its metabolites, the activation of these pathways lead to potential serotonergic deficiency along with altered enteric nervous system and central nervous system functionalities, thus leading to microbial dysbiosis, as a classical symptom of IBS. CRF: Corticotropin-releasing factor; ANS: Autonomic nervous system; CNS: Central nervous system; ACTH: Adrenocorticotropic hormone; IDO: Indoleamine-2,3-dioxygenase; TDO: Tryptophan-2,3-dioxygenase.
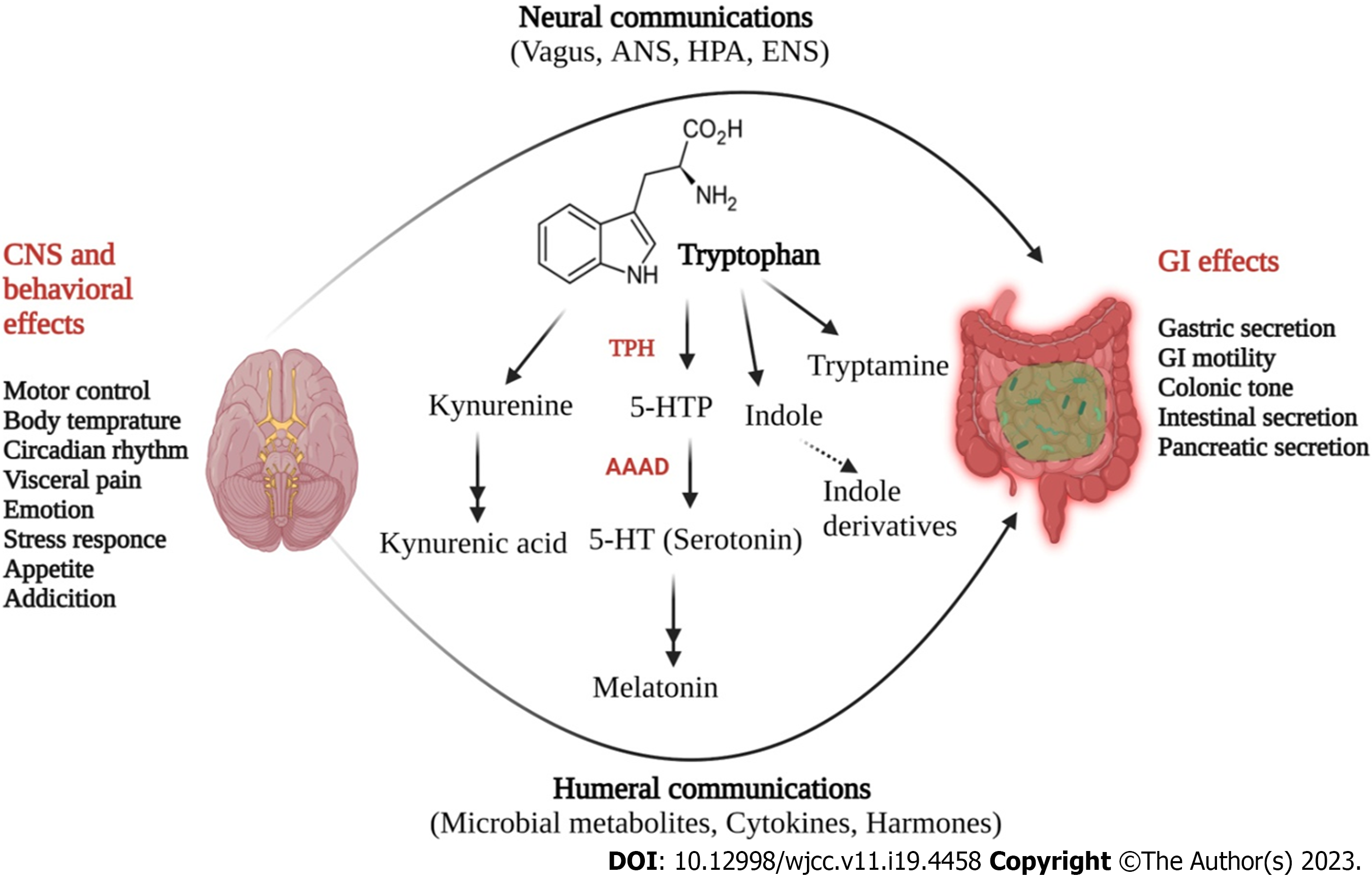
Figure 4 Tryptophan derived serotonergic metabolism in gut brain axis cross talk.
Upon absorption in the gut, L-tryptophan is metabolized through three pathways, particular to bacterial cells (indole pathway) of gut microbiota and mammalian cells (kynurenine and serotonin pathways). Tryptophan is converted to 5-hydoxytryptophan (5-HTP) by tryptophan hydroxylase and thereafter converted to -5-HT by the enzyme aromatic L-amino acid decarboxylase. In addition to this, tryptophan is also metabolized to indole derivatives and kynurenine, which also perform various biological functions. Tryptophan derived 5-HT regulates various functions in central nervous system (including emotion, cognition, stress, and visceral perception) and in enteric nervous system (gastrointestinal motility and secretion). CRF: Corticotropin-releasing factor; ANS: Autonomic nervous system; CNS: Central nervous system; GI: Gastrointestinal; 5-HT: 5-Hydroxytryptamine; HPA: Hypothalamic-pituitary-adrenal.
- Citation: Singh SV, Ganguly R, Jaiswal K, Yadav AK, Kumar R, Pandey AK. Molecular signalling during cross talk between gut brain axis regulation and progression of irritable bowel syndrome: A comprehensive review. World J Clin Cases 2023; 11(19): 4458-4476
- URL: https://www.wjgnet.com/2307-8960/full/v11/i19/4458.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i19.4458