Copyright
©The Author(s) 2023.
World J Clin Cases. Jun 16, 2023; 11(17): 4133-4141
Published online Jun 16, 2023. doi: 10.12998/wjcc.v11.i17.4133
Published online Jun 16, 2023. doi: 10.12998/wjcc.v11.i17.4133
Figure 1 The intraoperative timeline for the patient.
CVC: Central intravenous; CTPA: Computed tomography pulmonary angiography; CPCR: Cardiopulmonary cerebral resuscitation; ECMO: Extracorporeal membrane oxygenation; TEE: Trans-esophageal echocardiogram; PICU: Pediatric intensive care unit; EtCO2: End-tidal carbon dioxide.
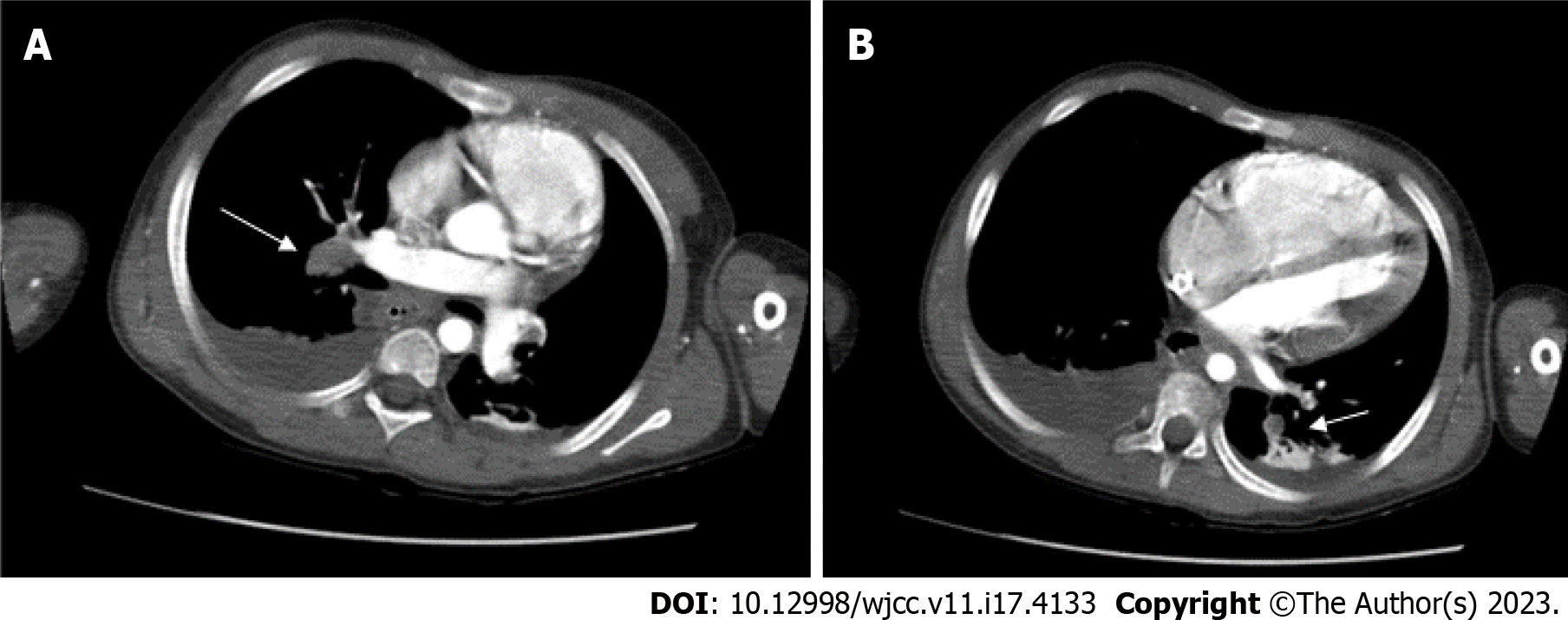
Figure 2 Pulmonary artery embolism.
The intraluminal filling defects are noted in A: The right interlobar; B: The left truncus. Bilateral posterior pleural effusions are noted with posterior passive atelectasis of both lungs.
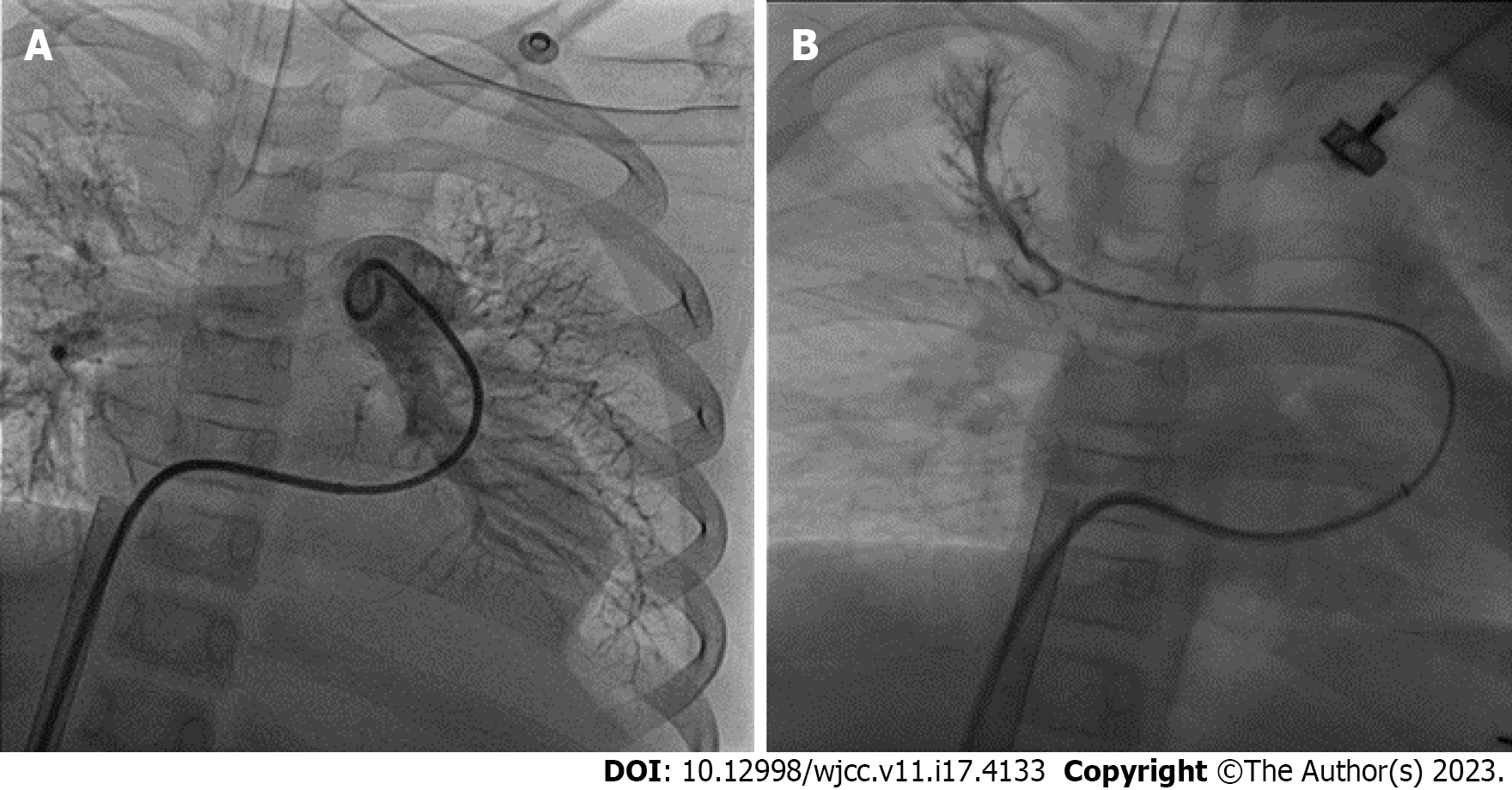
Figure 3 Catheter thrombolysis.
Ekosonic Endovascular System-directed thrombolysis was advanced to, A: The left truncus; B: The right upper pulmonary artery.
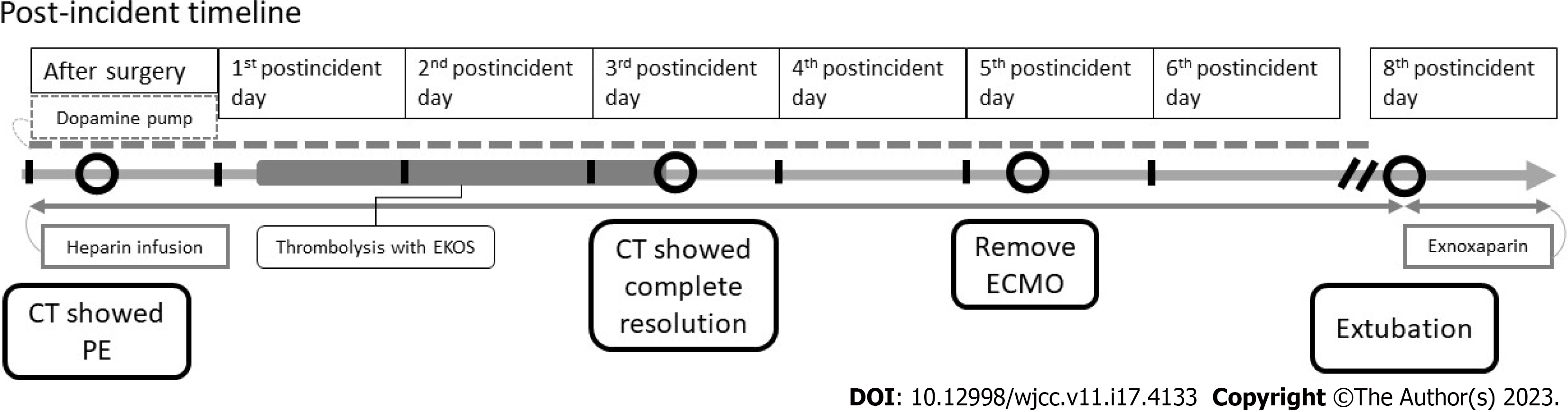
Figure 4 The post-incident timeline for the patient.
CT: Computed tomography; ECMO: Extracorporeal membrane oxygenation; PE: Pulmonary embolism.
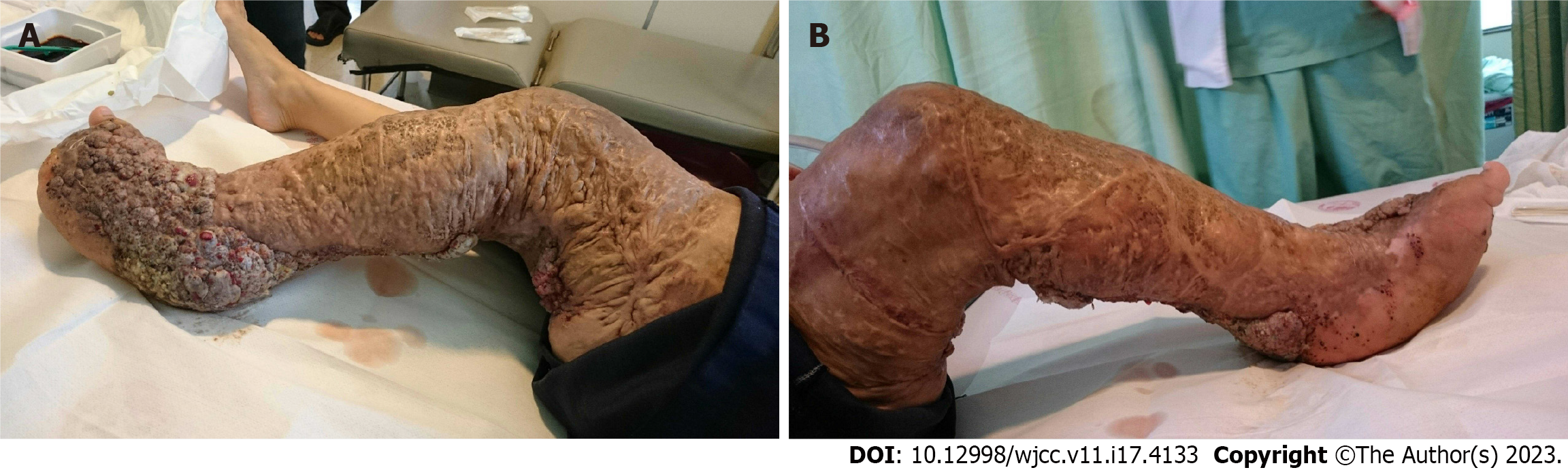
Figure 5 Clinical photograph of the patient showing hypertrophy of the left lower limb.
A: The lateral view: B: The medial view.
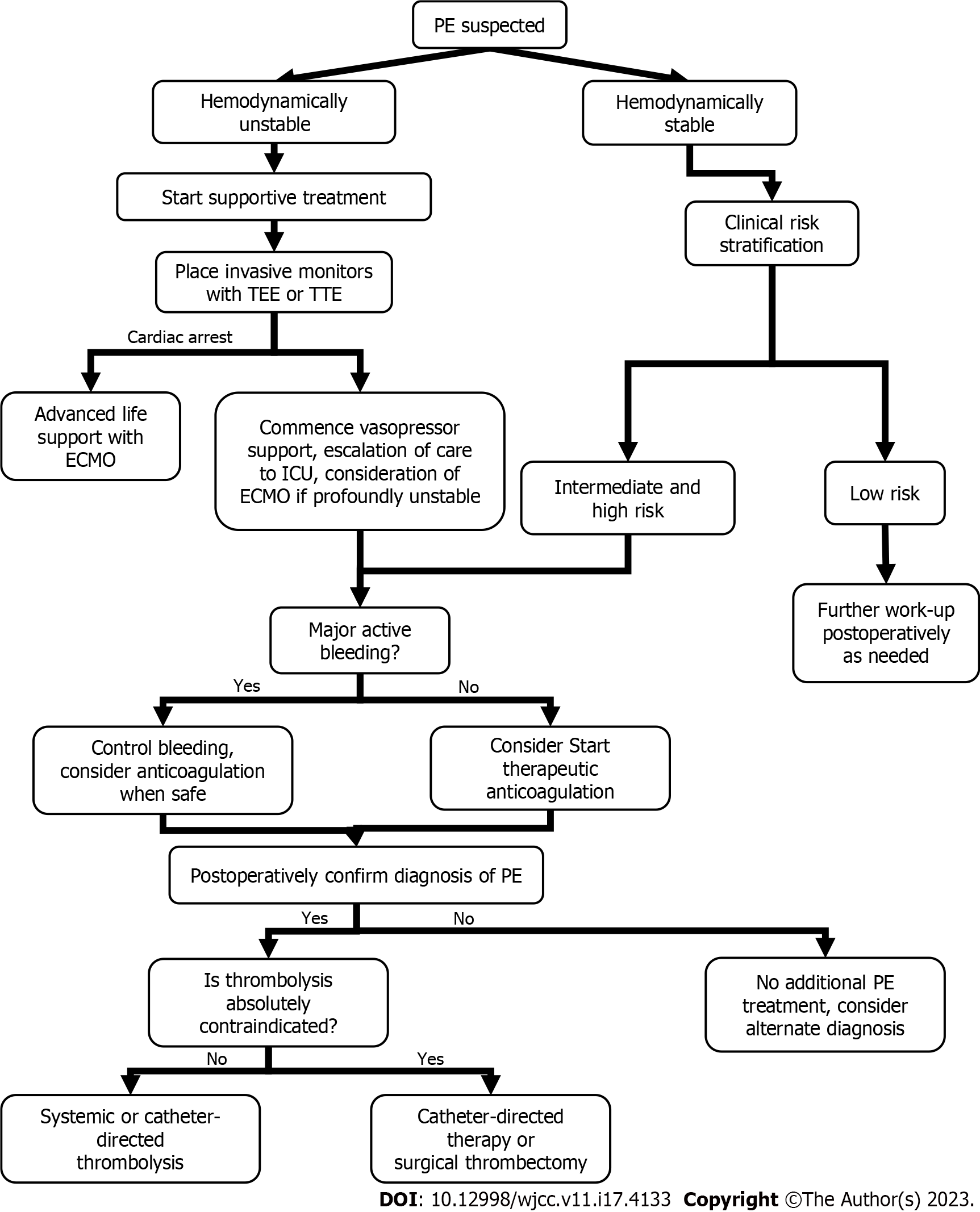
Figure 6 Algorithm for effective intraoperative decision-making while managing a patient with a pulmonary embolism.
ECMO: Extracorporeal membrane oxygenation; TEE: Trans-esophageal echocardiogram; TTE: transthoracic echocardiography; PE: Pulmonary embolism; ICU: Intensive care unit.
- Citation: Lo CY, Chen KB, Chen LK, Chiou CS. Massive pulmonary embolism in Klippel-Trenaunay syndrome after leg raising: A case report. World J Clin Cases 2023; 11(17): 4133-4141
- URL: https://www.wjgnet.com/2307-8960/full/v11/i17/4133.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i17.4133