Copyright
©The Author(s) 2023.
World J Clin Cases. Jun 6, 2023; 11(16): 3837-3846
Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3837
Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3837
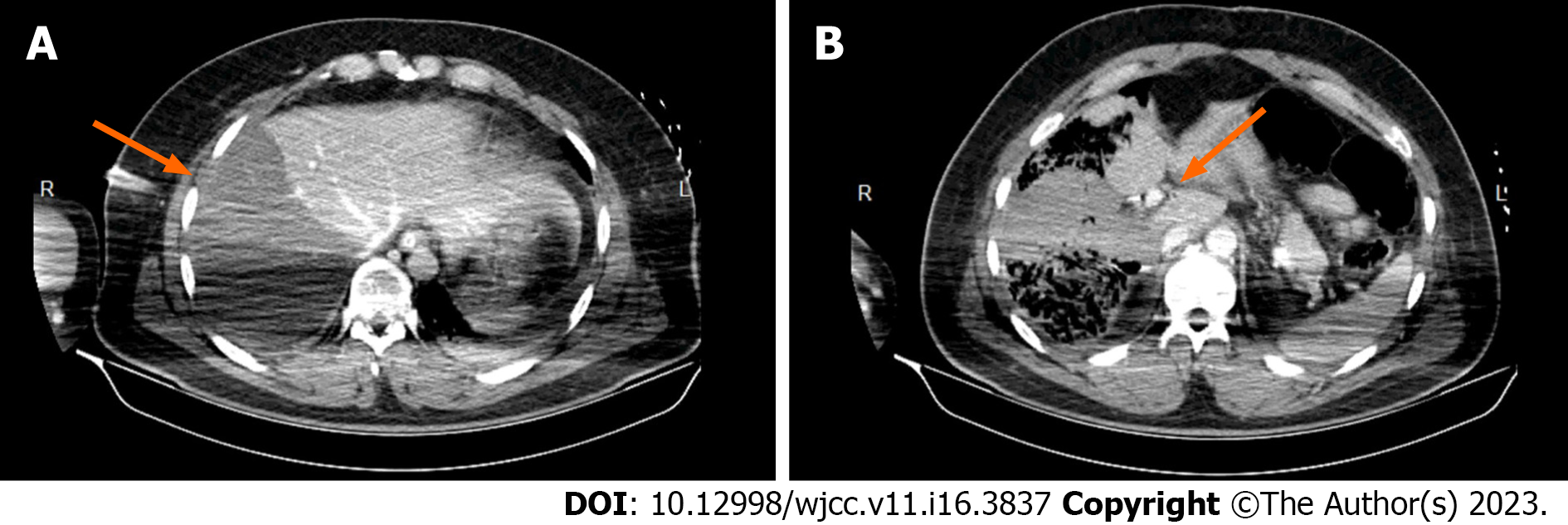
Figure 1 Preoperative computed tomography scan image performed upon admission in our tertiary hepato-bilio-pancreatic referral center.
A: Ischemic right hemiliver post-right hepatic pedicle ligation upon damage control surgery; B: Right hepatic pedicle ligated proximally.
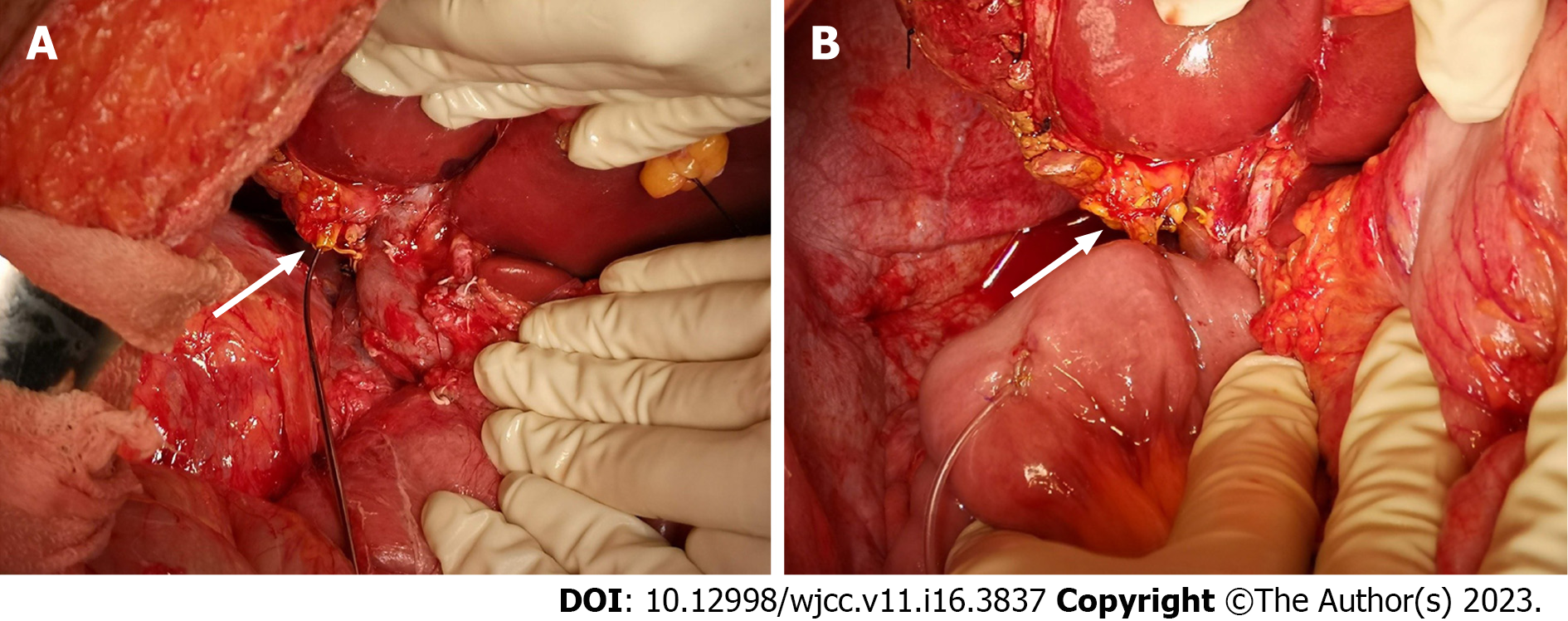
Figure 2 Intraoperative aspect.
A: Sectioned common hepatic duct, prepared for the hepaticojejunostomy; B: Finished hepaticojejunostomy.
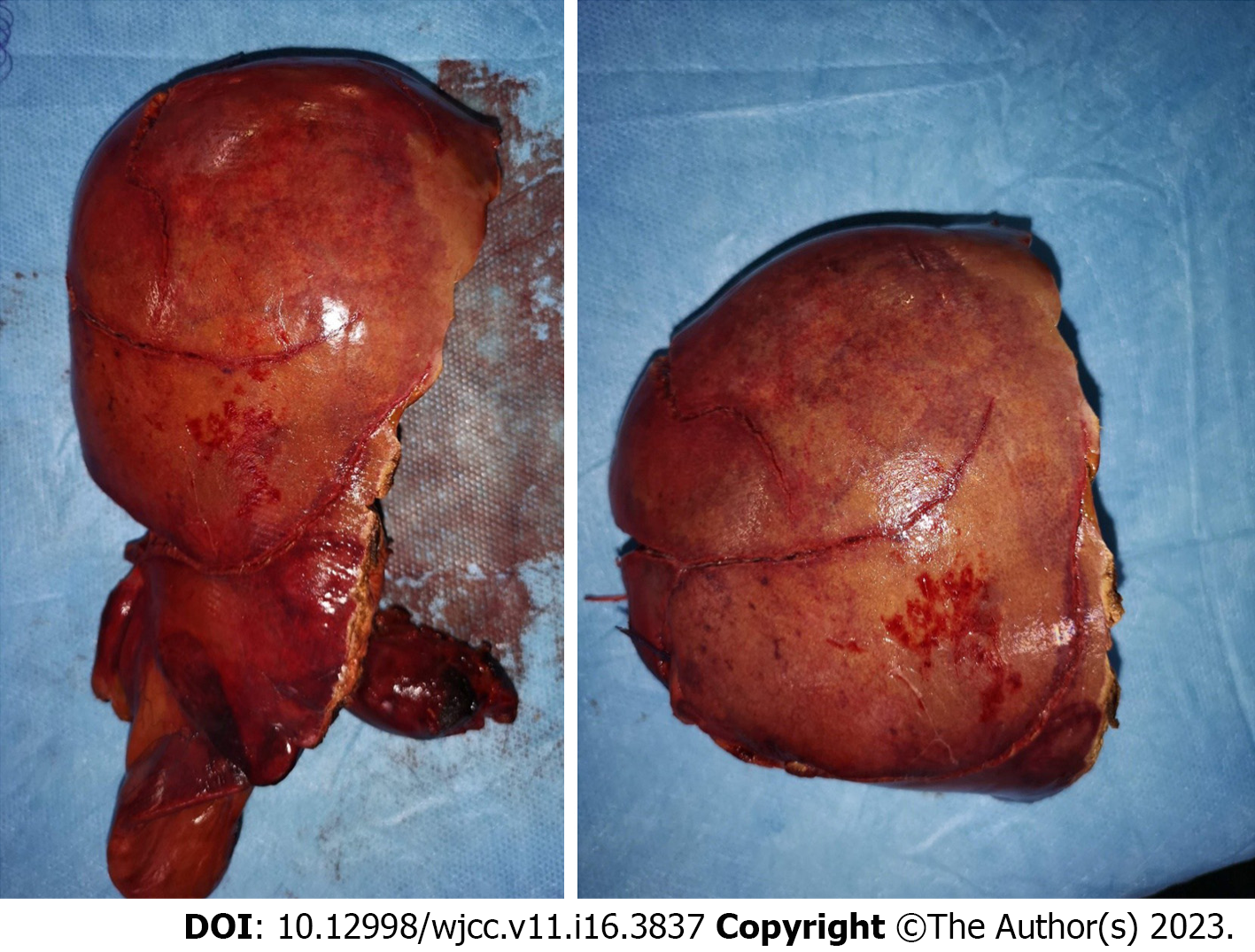
Figure 3 Gross pathology of the resected right hemiliver.
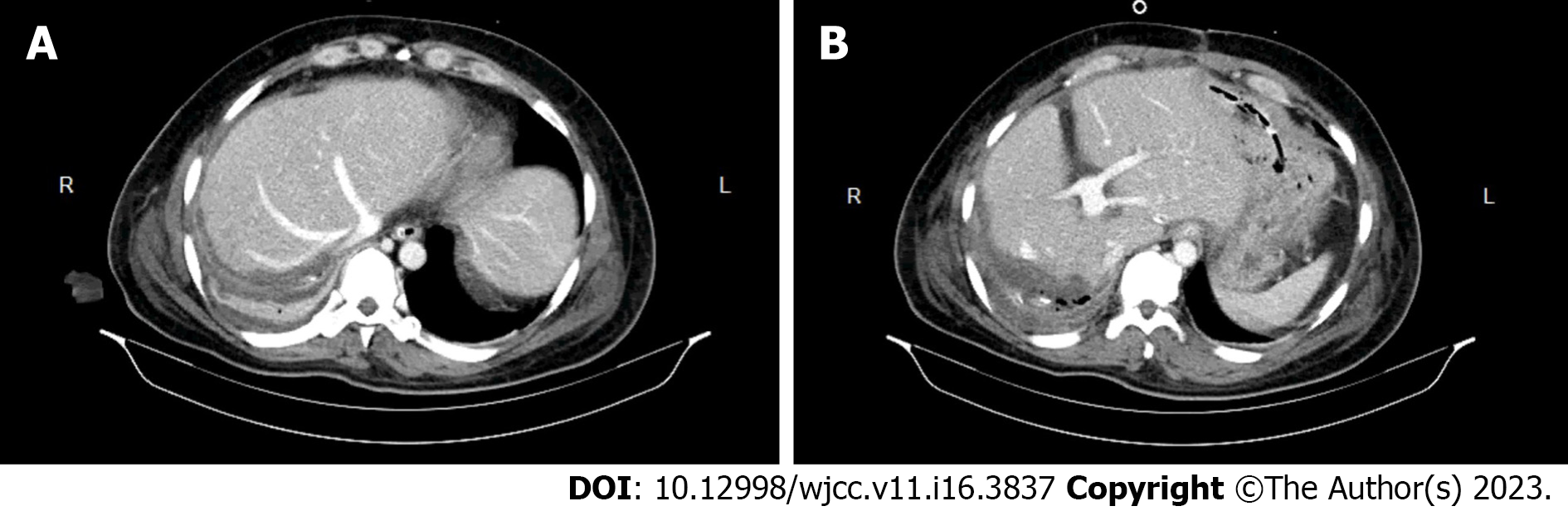
Figure 4 Postresection computed tomography scan image.
A: Remnant left hemiliver showing no ischemic regions; B: Image showing the left portal vein branches.
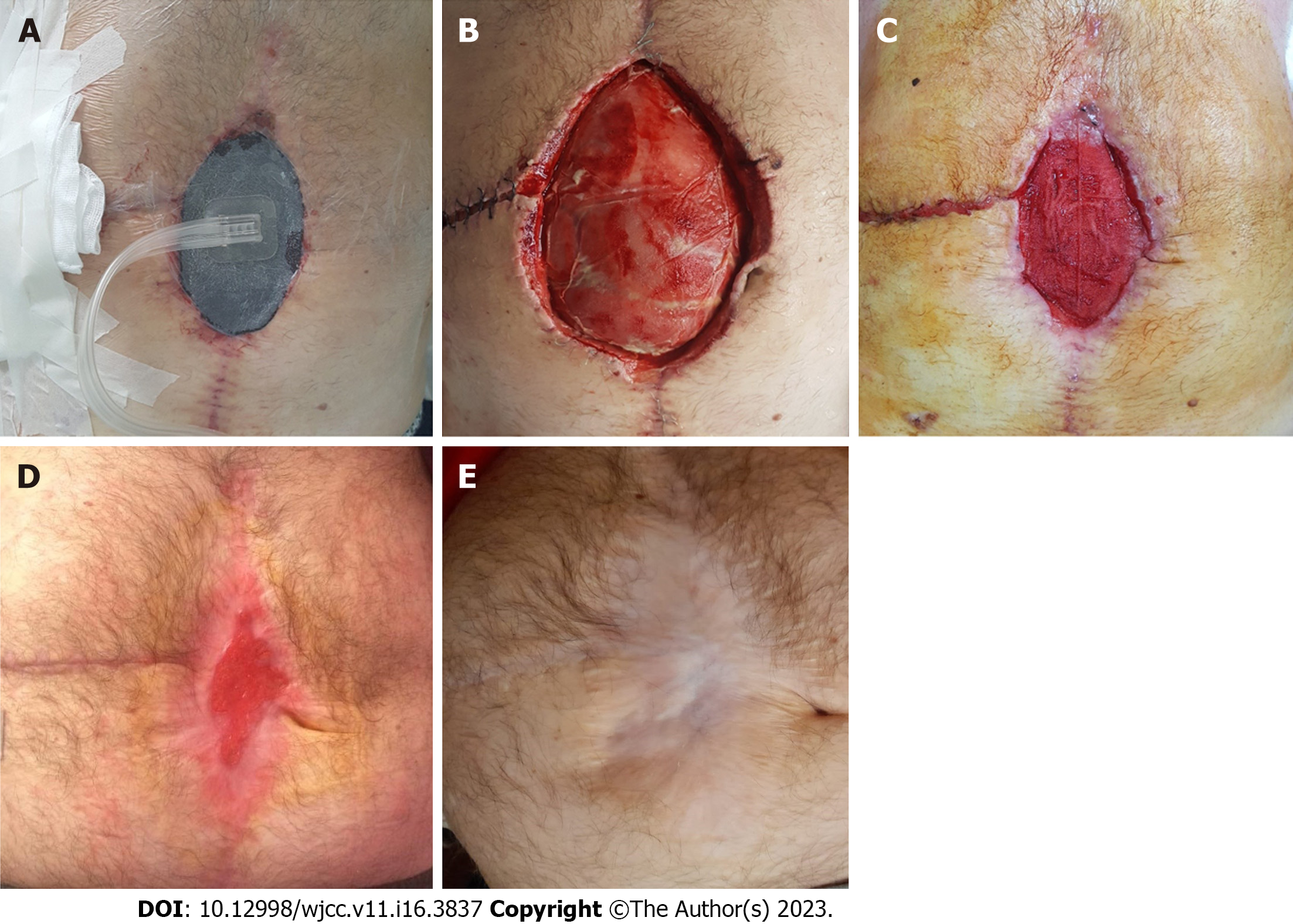
Figure 5 Postoperative aspect.
A: The surgical incisional site evisceration managed by negative-pressure wound therapy on the 48th postoperative day (POD); B: 18th POD aspect showing the surgical incisional site evisceration; C: 48th POD aspect showing the surgical incisional site evisceration managed by negative-pressure wound therapy; D: 4 mo postoperative aspect showing the chronological evolution of the surgical incisional site evisceration managed by negative-pressure wound therapy; E: 55 mo postoperative aspect showing the chronological evolution of the surgical incisional site evisceration following negative-pressure wound therapy.
- Citation: Mitricof B, Kraft A, Anton F, Barcu A, Barzan D, Haiducu C, Brasoveanu V, Popescu I, Moldovan CA, Botea F. Severe liver trauma with complex portal and common bile duct avulsion: A case report and review of the literature. World J Clin Cases 2023; 11(16): 3837-3846
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3837.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3837