Copyright
©The Author(s) 2023.
World J Clin Cases. Apr 26, 2023; 11(12): 2637-2656
Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2637
Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2637
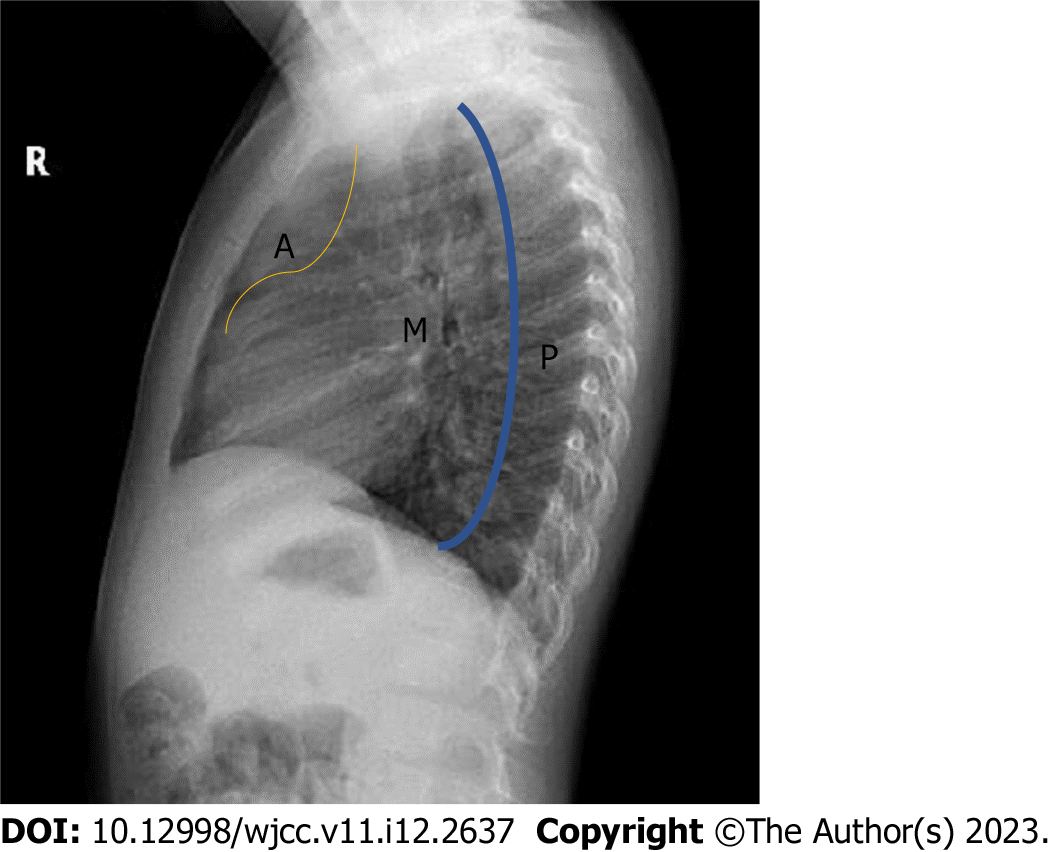
Figure 1 Mediastinal compartment classification on lateral radiograph.
The borders of the mediastineal compartments anterior mediastinum are formed by the sternum anteriorly, the anterior edge of the pericardium posteriorly, the middle mediastinum by the pericardium anteriorly, the line passing 1 cm posterior to the anterior border of the thoracic vertebrae posteriorly, and the posterior mediastinum by the vertebral corpuscles behind this line and the posterior transverse processes. A (yellow line): Anterior; M: Middle; P (blue line): Posterior.
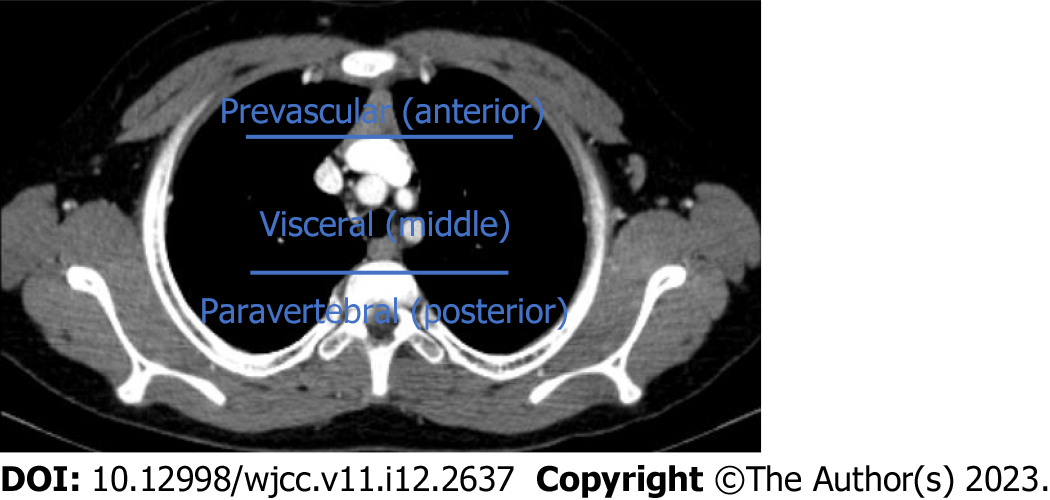
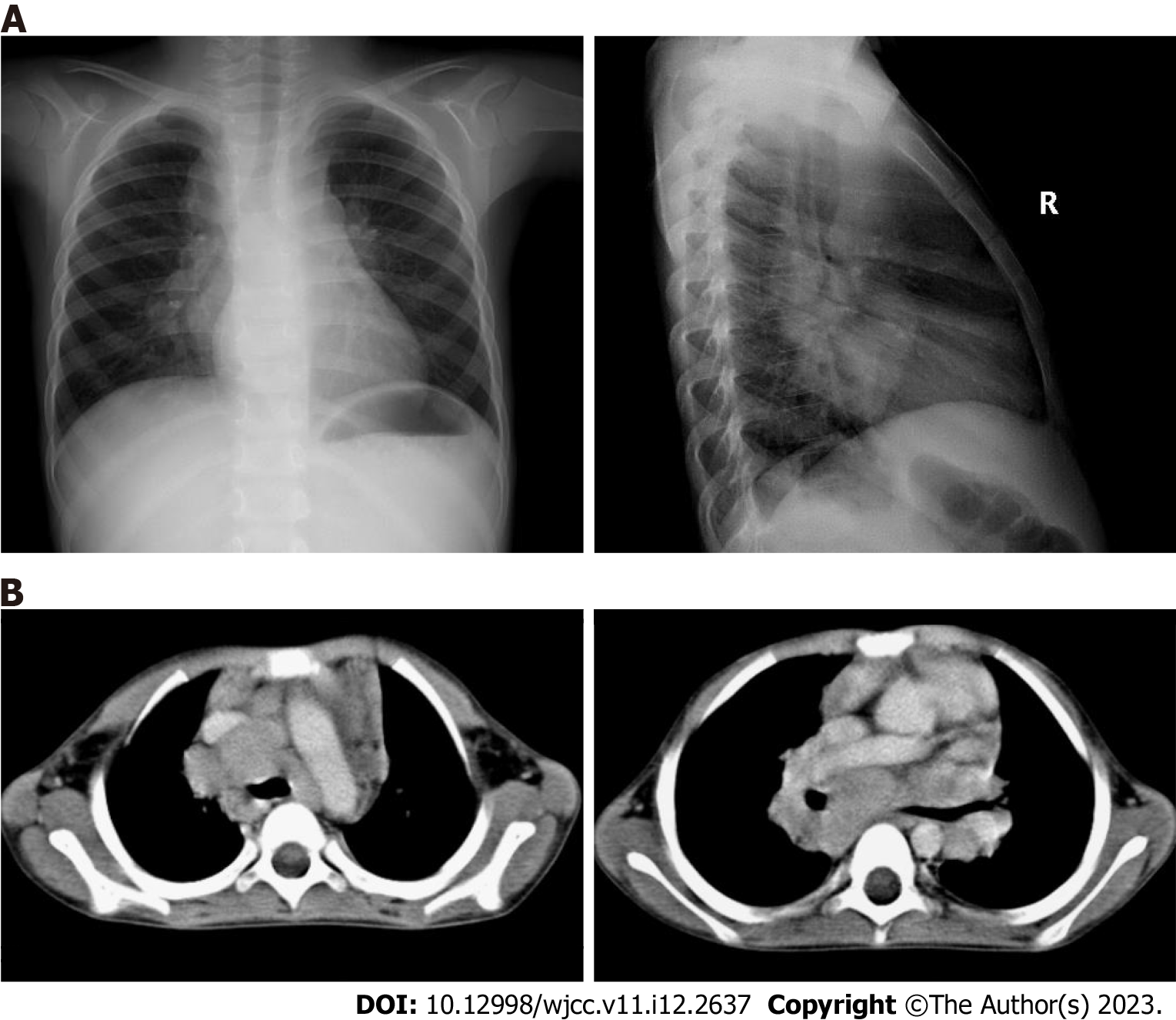
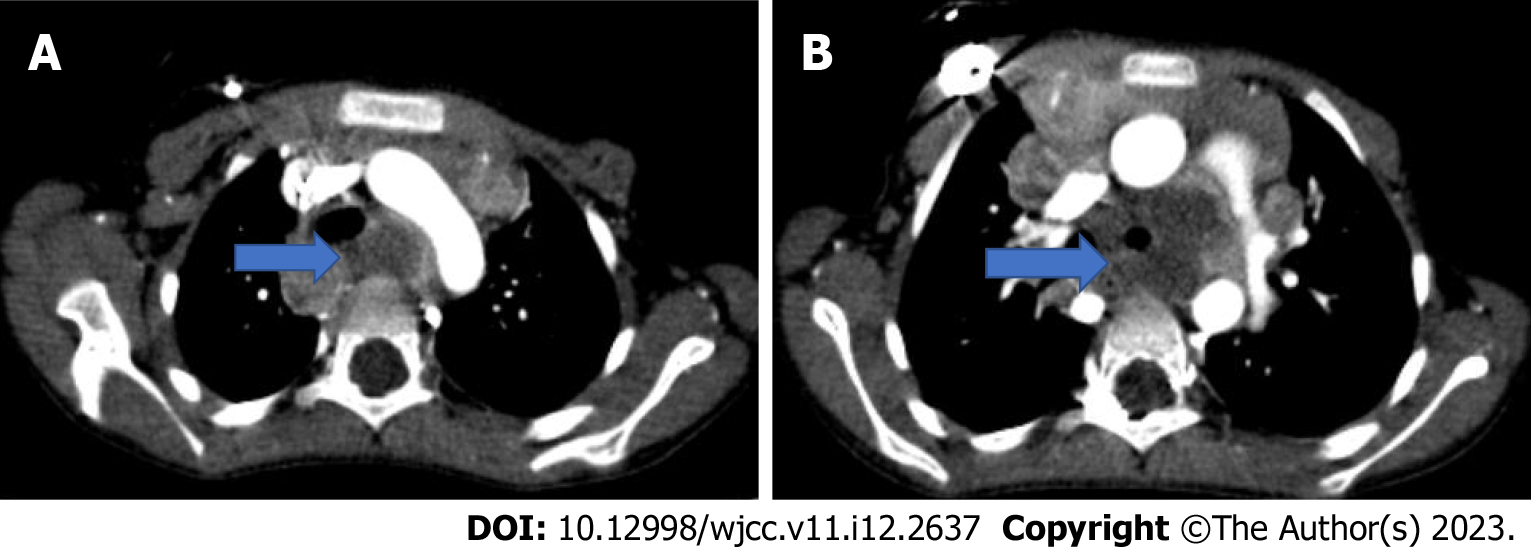
Figure 2 International Thymic Malignant Interest Group classification.
In the axial computed tomography section passing through the superior aortic arch, the area between the sternum and the pericardium is the prevascular distance, the area between the pericardium and the line passing 1 cm distal to the anterior part of the vertebral corpus is the visceral distance, and the area posterior to this line is the paravertebral distance has been defined as.
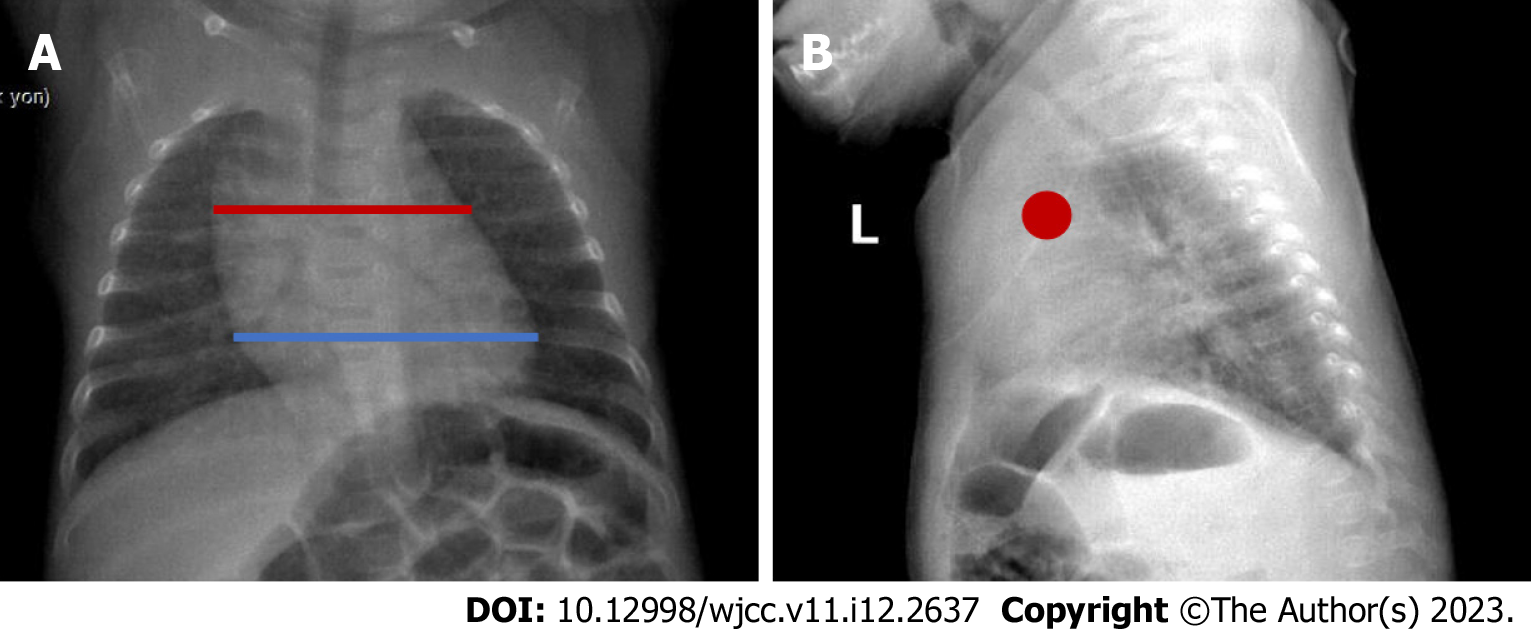
Figure 3 A 3-year-old boy normal thymus.
A: The red line shows the thymus and the blue line shows the heart in the posteroanterior chest radiograph. In infants, the thymus erases the heart contours, and because it is superposed with the hiluses, the hiluses cannot be clearly distinguished. It also does not create a compression effect. B: Anterior location of the thymus is observed with a red dot on the lateral radiograph.
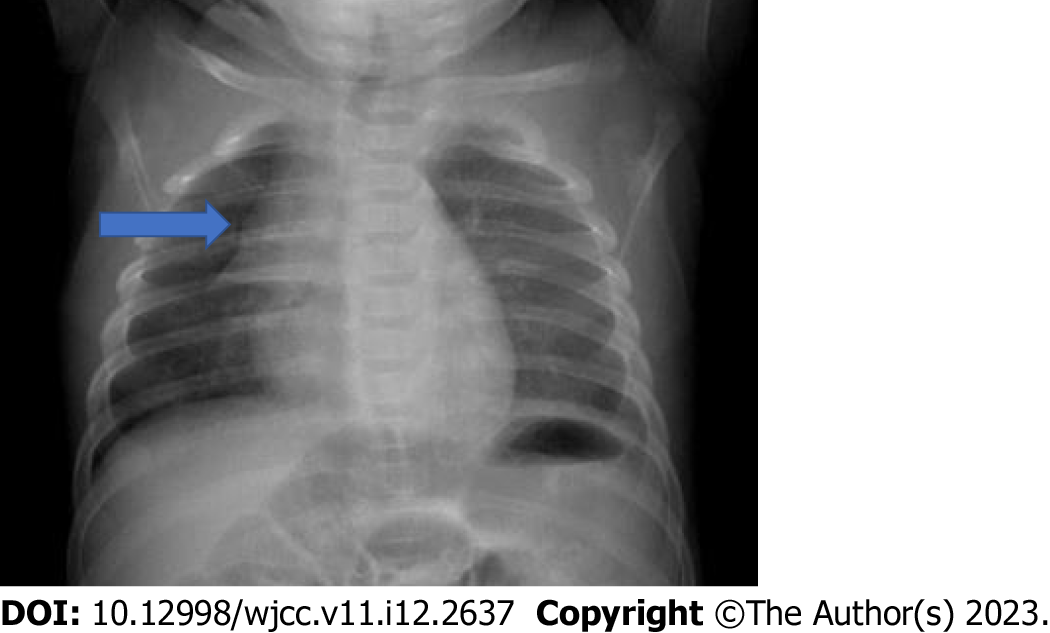
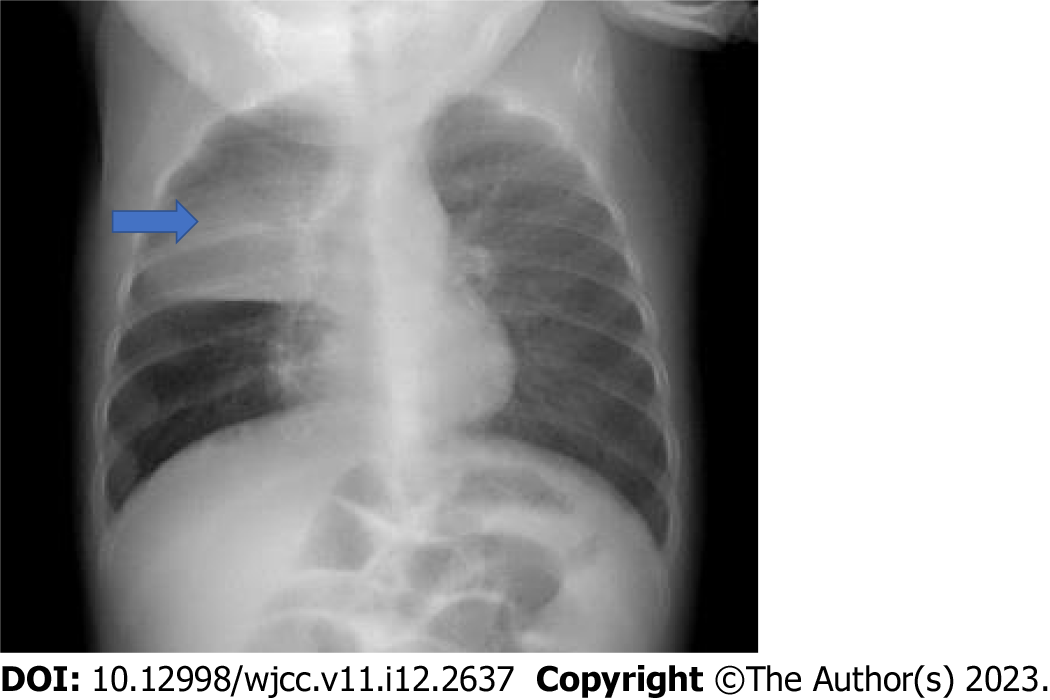
Figure 4 The wave sign (blue arrow) is the corrugation view of the right lobe of the thymus due to its abutment to the ribs.
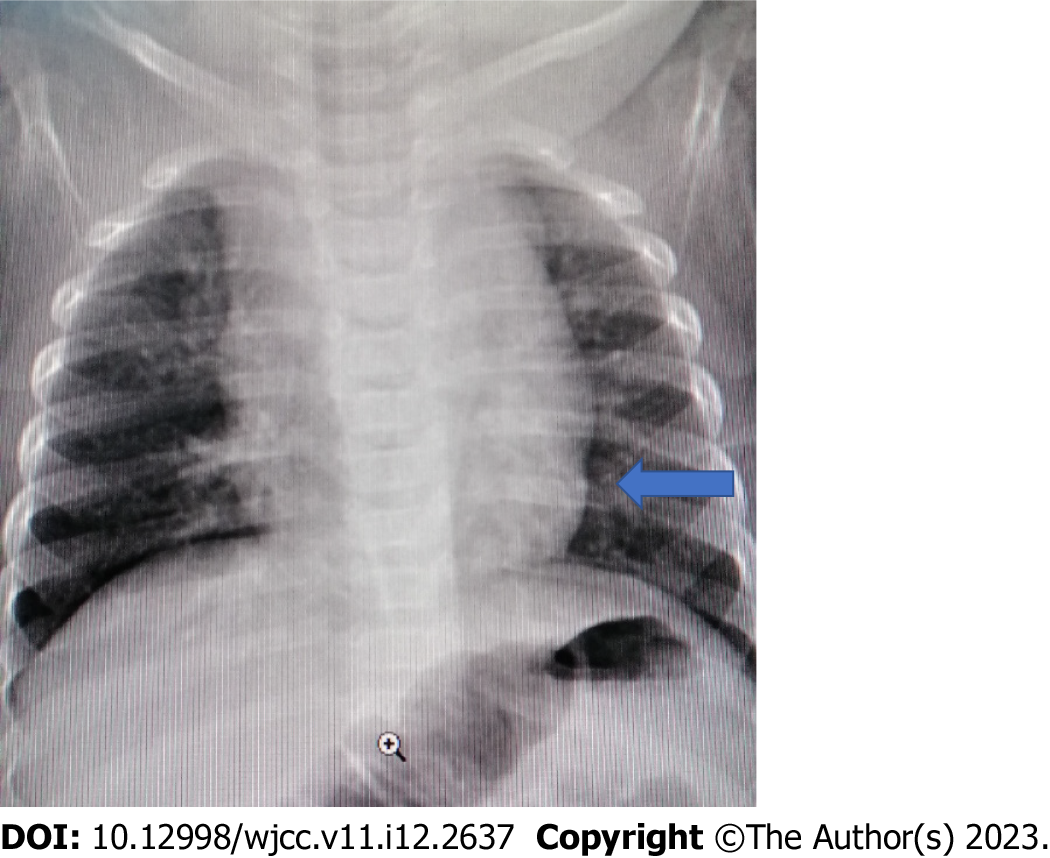
Figure 5 Sail sign (blue arrow) is the triangular shape of the right lobe of the thymus and the minor fissure forming its lower border.
Figure 6 The contour (blue arrow) formed at the junction of the thymus with the heart is the cardiothymic notch.
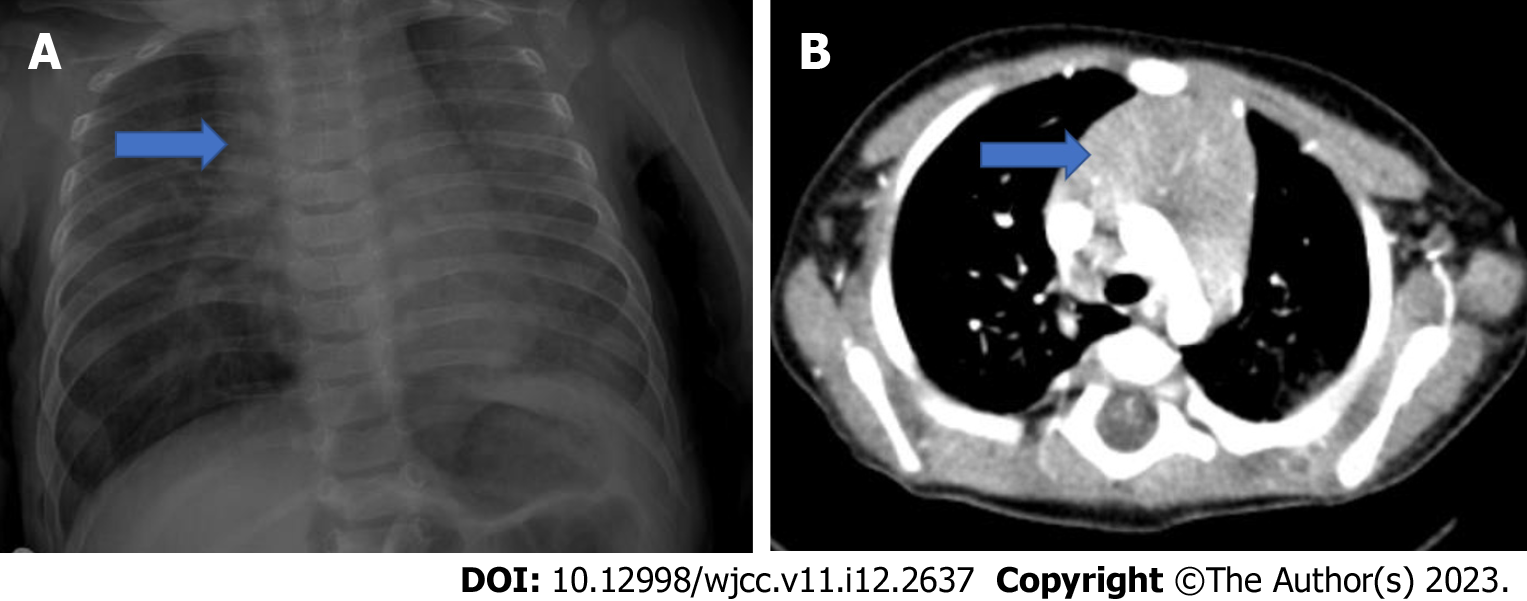
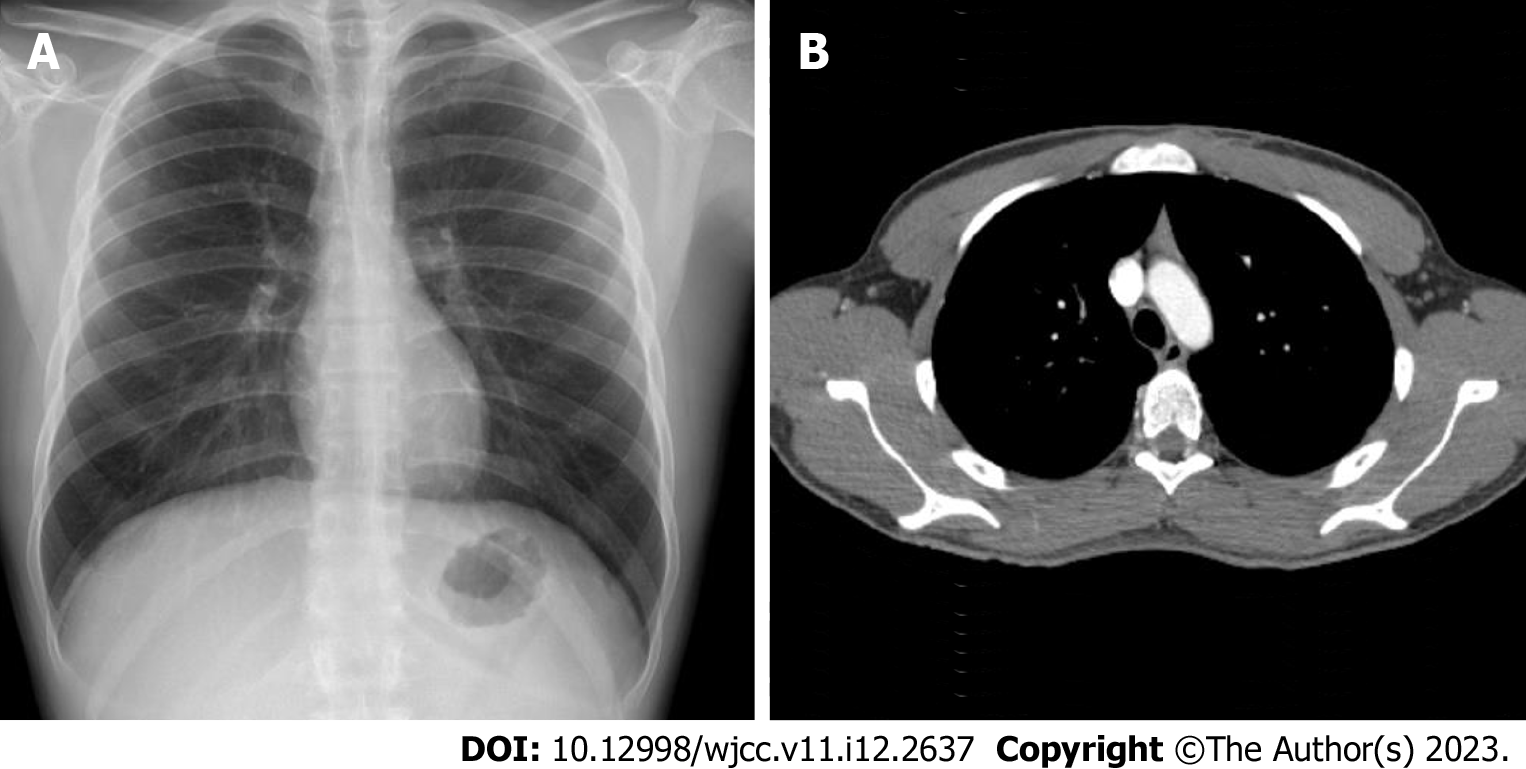
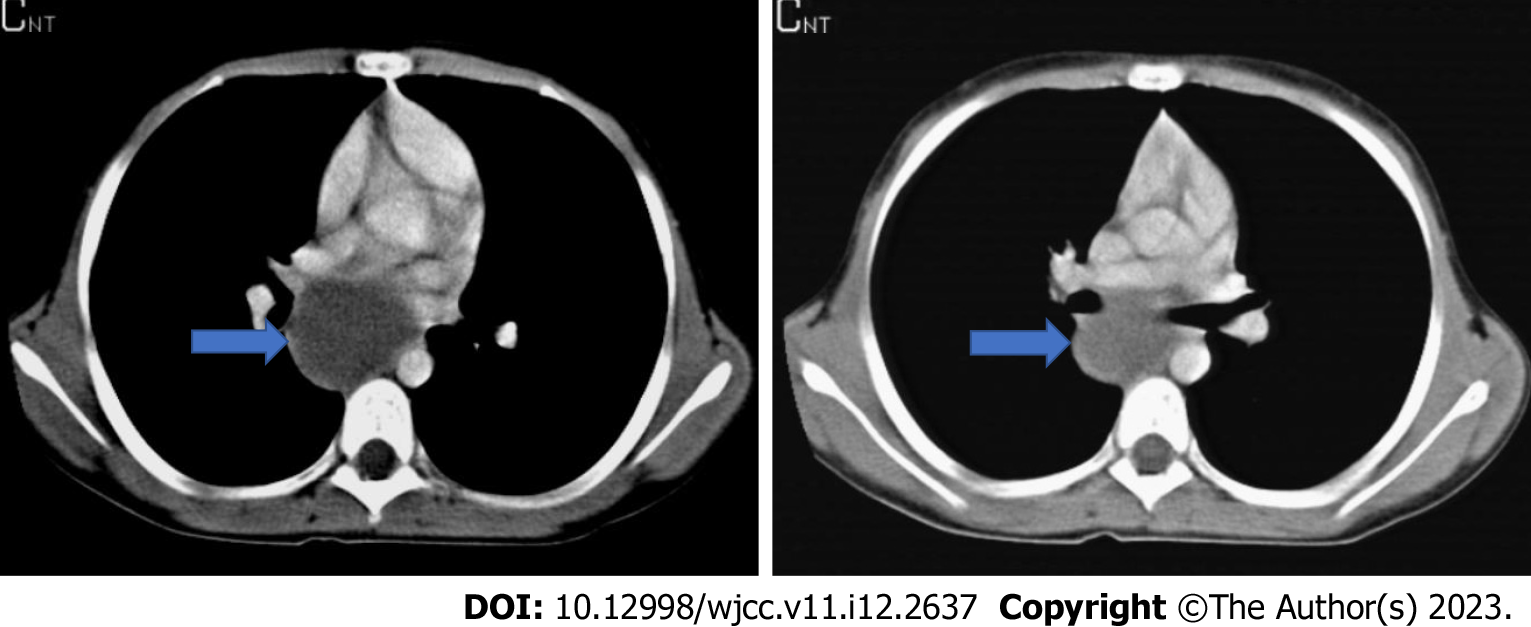
Figure 7 Normal thymus and axial computed tomography of a 4-mo-old patient.
A: Normal thymus on posteroanterior chest radiograph; B: Axial computed tomography (CT) examination of a 4-mo-old patient. In CT, the thymus (blue arrow) arcus is observed in the prevascular distance at the level of the aorta, its edges are convex, with homogeneous density and it does not cause a compression effect.
Figure 8 A 4-year-old patient's posteroanterior chest radiograph.
A: It shows a decrease in the dimensions of the thymus; B: Flattened edges in the axial computed tomography examination.
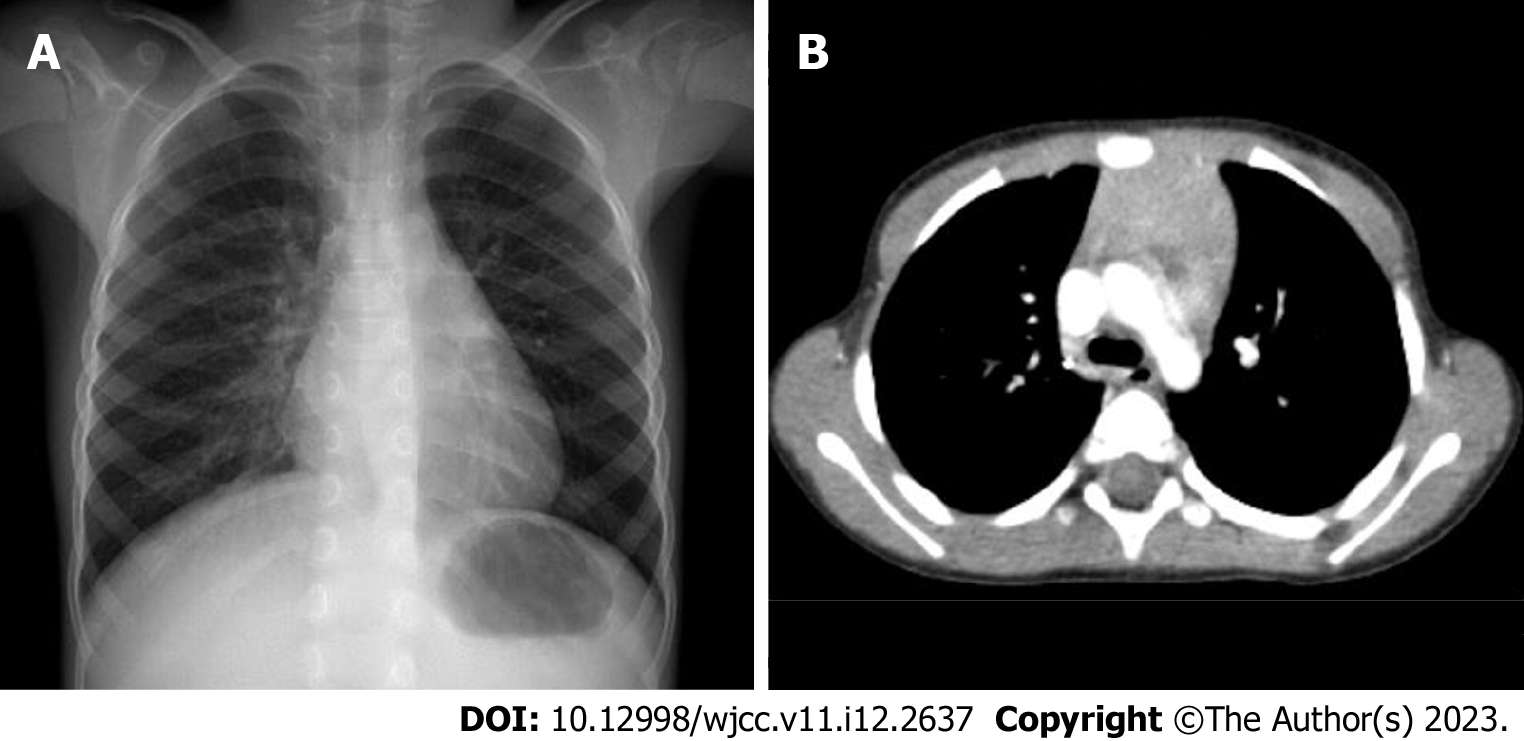
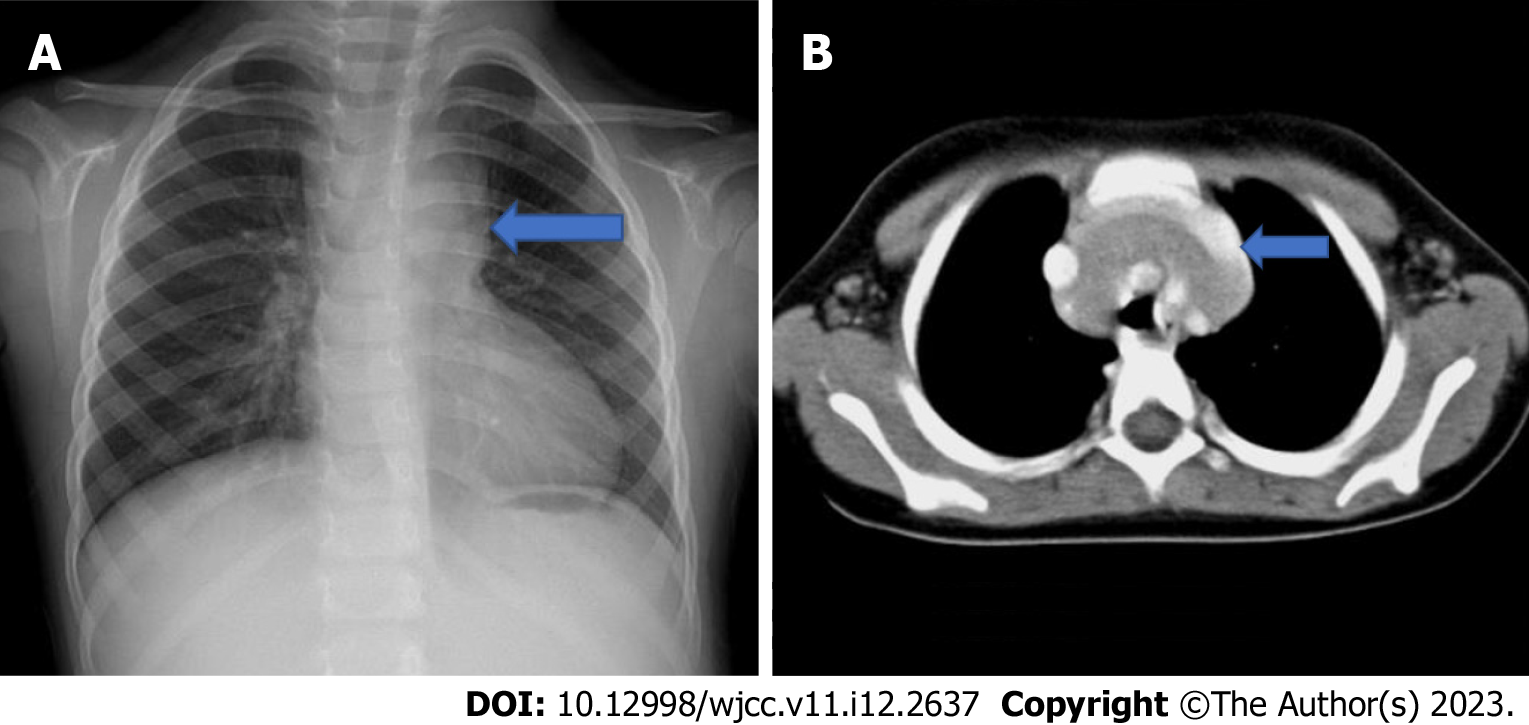
Figure 9 A 17-year-old patient’s examination.
A: Thymus is not observed in the posteroanterior chest radiograph of the 17-year-old patient; B: In the axial section, on computed tomography, it is observed as small, triangular in the anterior mediastinum, with concave edges and lower density due to the fat tissue it contains.
Figure 10 A 3-year-old patient who presented with the complaint of cough.
A: There is mediastinal enlargement on the left in the posteroanterior chest radiograph; B: In the axial computed tomography examination, it is observed that the thymus forms the mediastinal enlargement and the thymus (blue arrow) extends to the posterior of the main vascular structures.
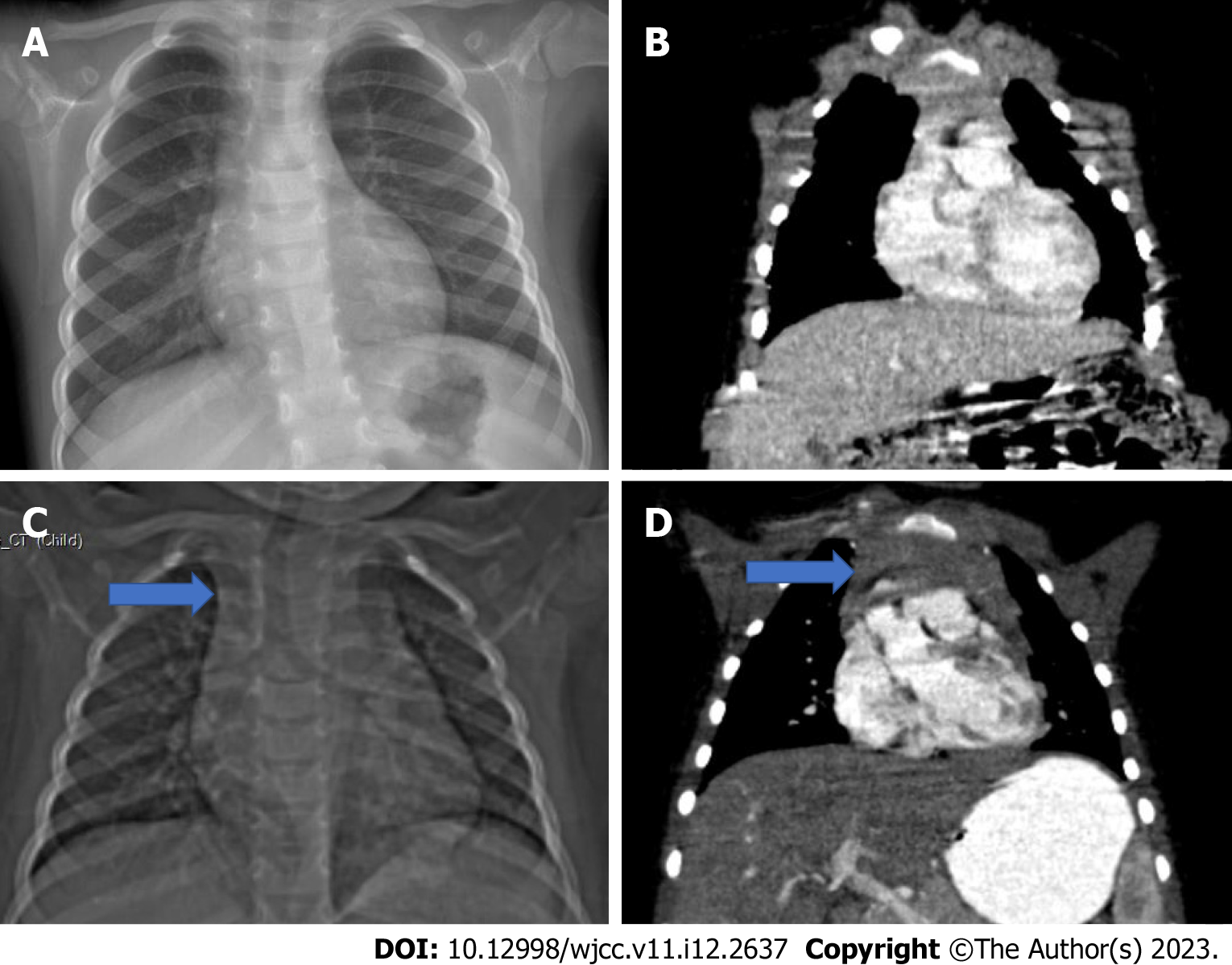
Figure 11 A 3-year-old patient who was followed up with an operated Wilms tumor during chemotherapy.
A: The thymus tissue is observed to be smaller than normal in the posteroanterior chest radiograph; B: Coronal computed tomography examination; C and D: In the second month follow-up of the same patient after the end of chemotherapy. Hyperplasia in the thymus (blue arrow) is observed in the scout (C) and coronal plane computed tomography images (D).
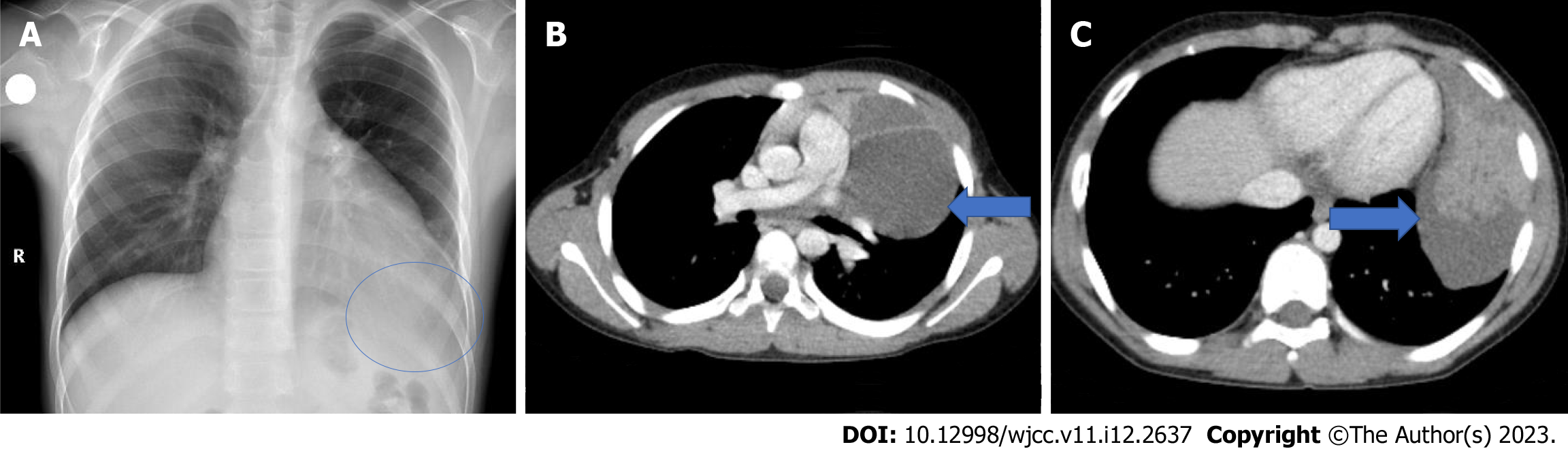
Figure 12 A 10-year-old patient who is being followed up for asthma.
A: Density that erases the heart and diaphragm contours (blue round) on the left is observed on posteroanterior chest radiography; B: Thymic cyst containing septa (blue arrow); C: A solid component of the thymoma (blue arrow) in the inferior of the cyst are observed.
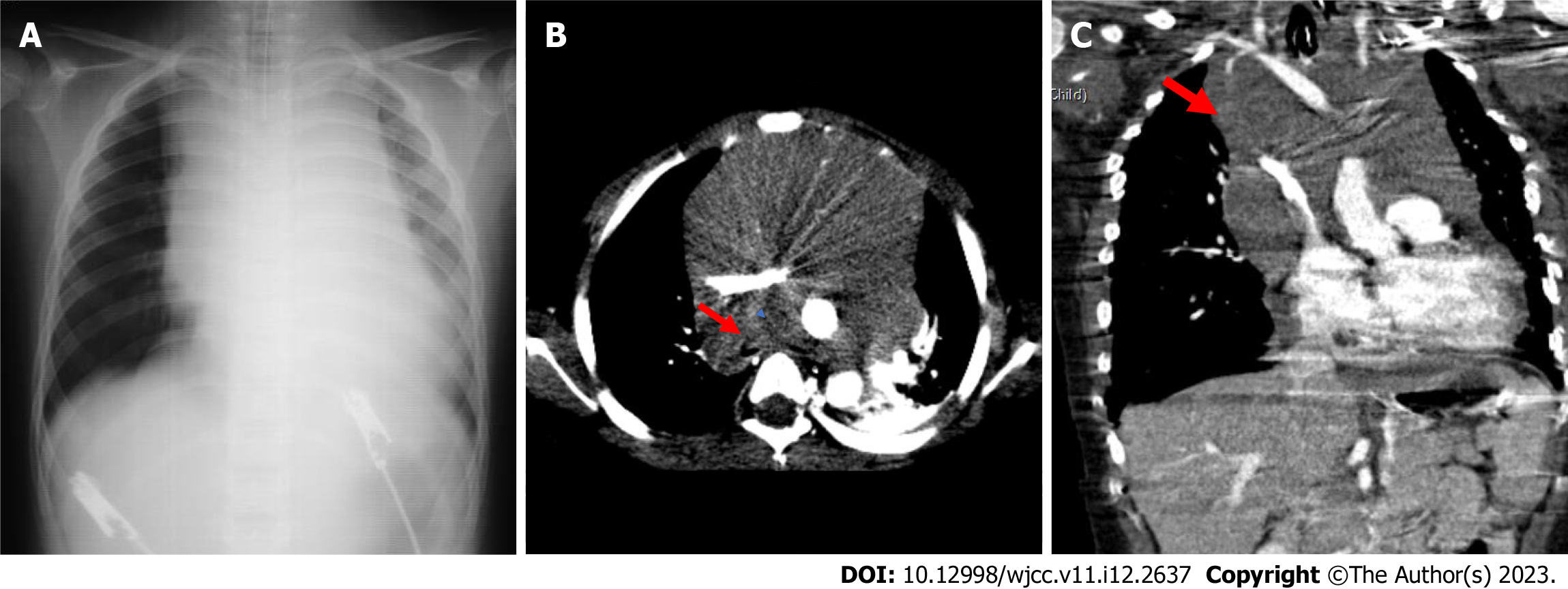
Figure 13 A 5-year-old patient with T-cell ALL has neck and back pain, shortness of breath, and cough.
A: On posteroanterior chest radiograph, significant enlargement of the mediastinum secondary to the mass and increased aeration in the right lung are observed; B: Compression of the right main bronchus secondary to the mass (red arrow) also draws attention; B and C: A mass lesion (red arrow) located in the anterior mediastinum but extending into the middle mediastinum and circulating the main vascular structures is observed.
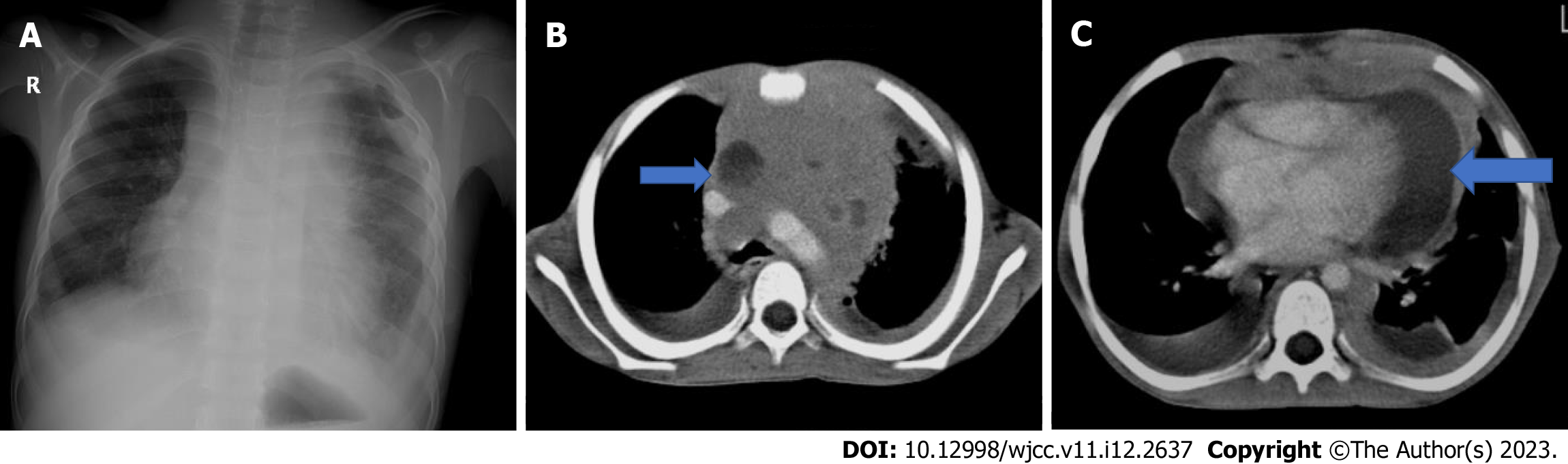
Figure 14 A 7 years old patient with T-cell lymphoblastic lymphoma.
A: There is cough and shortness of breath. Significant enlargement of the mediastinum, pleural effusion in the left hemithorax, and increased aeration in the right lung are observed in the posteroanterior chest radiograph; B and C: In the axial computed tomography examination, a mass lesion with fatty areas is located in the anterior mediastinum. Bilateral pleural and pericardial effusion, and pleural and pericardial fatty solid lesions (blue arrow) are also observed.
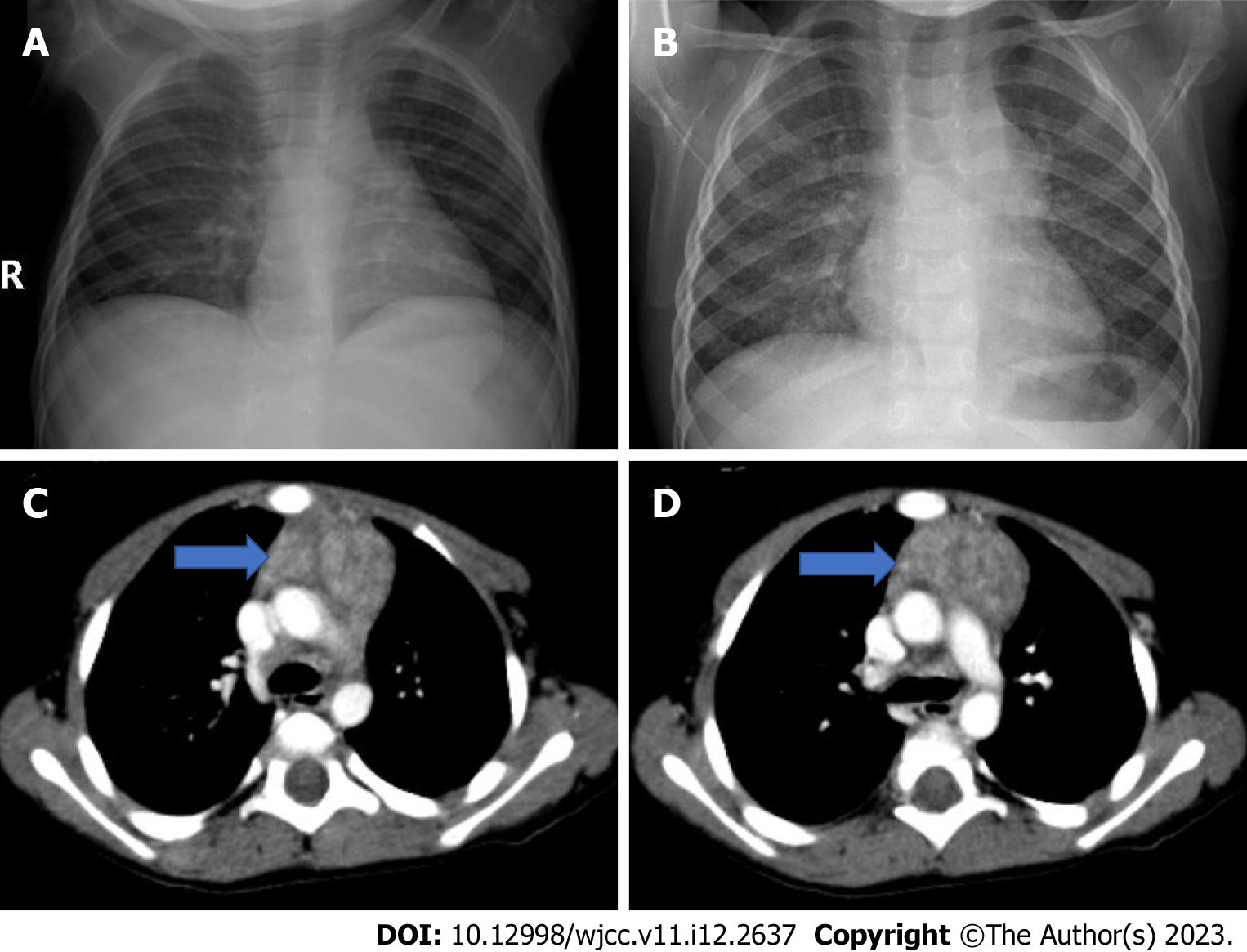
Figure 15 In the 1 year and 9 mo old patient with langerhans cell histiocytosis.
A: The first one; B: The second radiograph taken six months after A, Mediastinal enlargement and lobulation in the left mediastinal contour are observed; C and D: Thymic enlargement (blue arrow), lobulation in the contour and heterogeneous appearance are observed in the axial computed tomography images of the same patient.
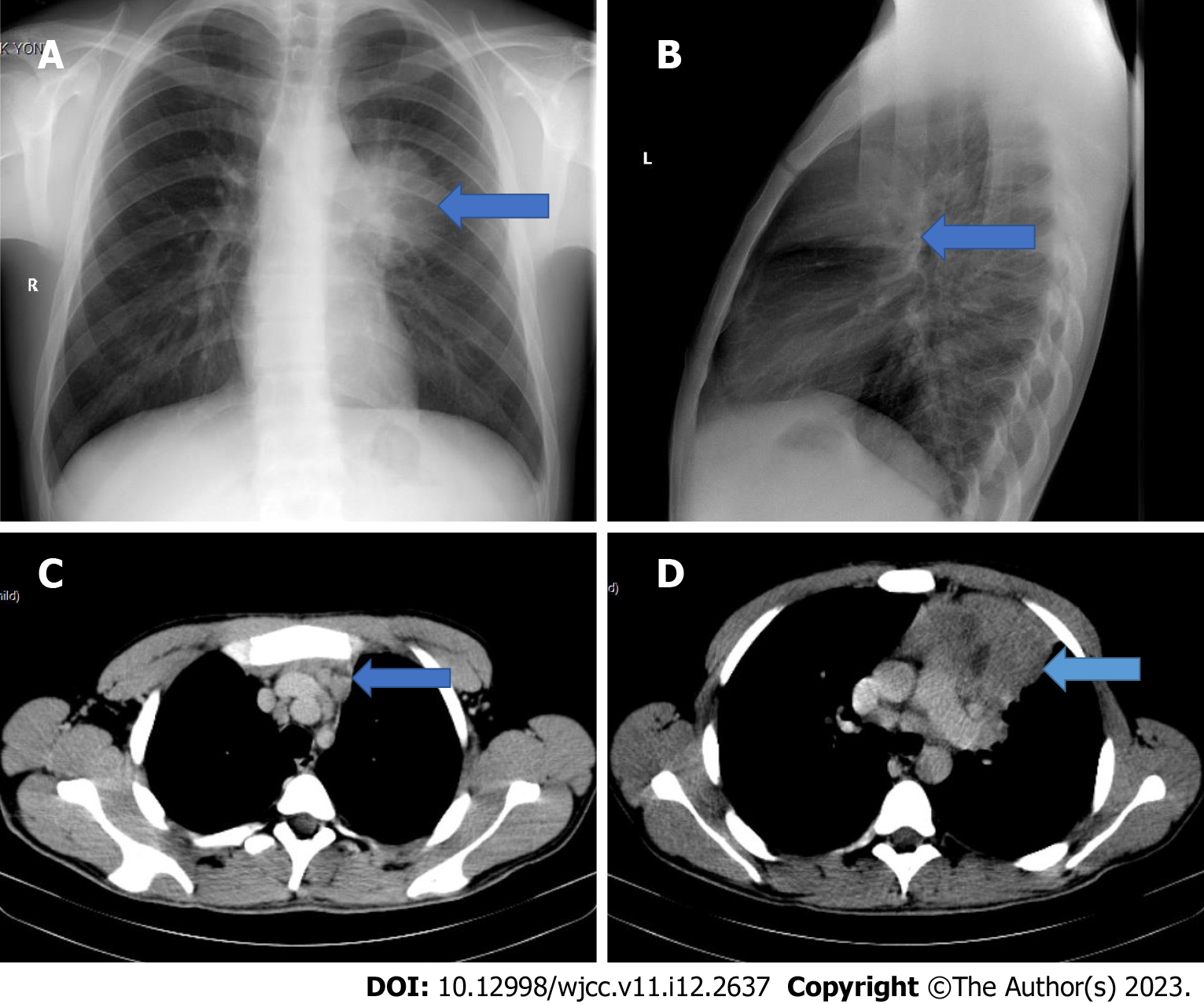
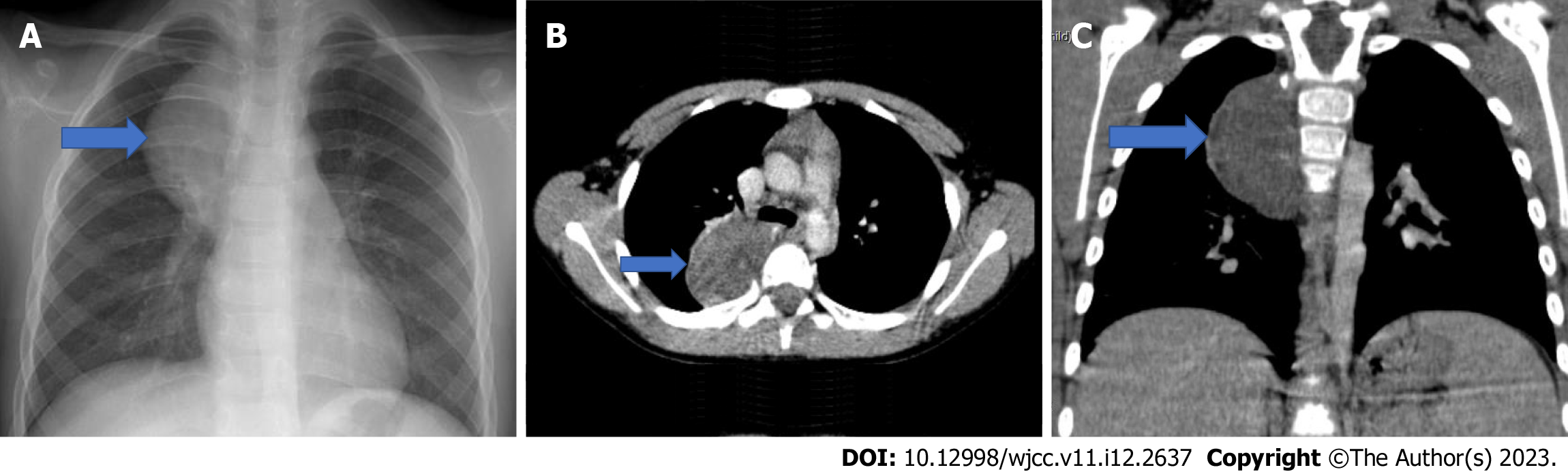
Figure 16 Hodgkin lymphoma (nodular sclerosing type).
A 17-year-old male patient presents with cough and weight loss. A and B: On the 2-way chest radiograph there is a mass density (blue arrow) located in the anterior mediastinum; C: Lymphadenopathies (blue arrow) in the upper mediastinum; D: A mass lesion containing cystic-necrotic areas (blue arrow) in the anterior mediastinum are detected.
Figure 17 4-year-old male patient with Hodgkin lymphoma (mixed cellular type).
A: Mediastinal enlargement and bilateral hilar lymphadenopathy are observed in the 2-way chest radiograph of the patient with the complaints of fever and anemia; B: Lymphadenopathies forming conglomeration in prevascular, paratracheal, subcarinal, hilar and azygoesophageal recess are observed in the axial computed tomography images of the same patient.
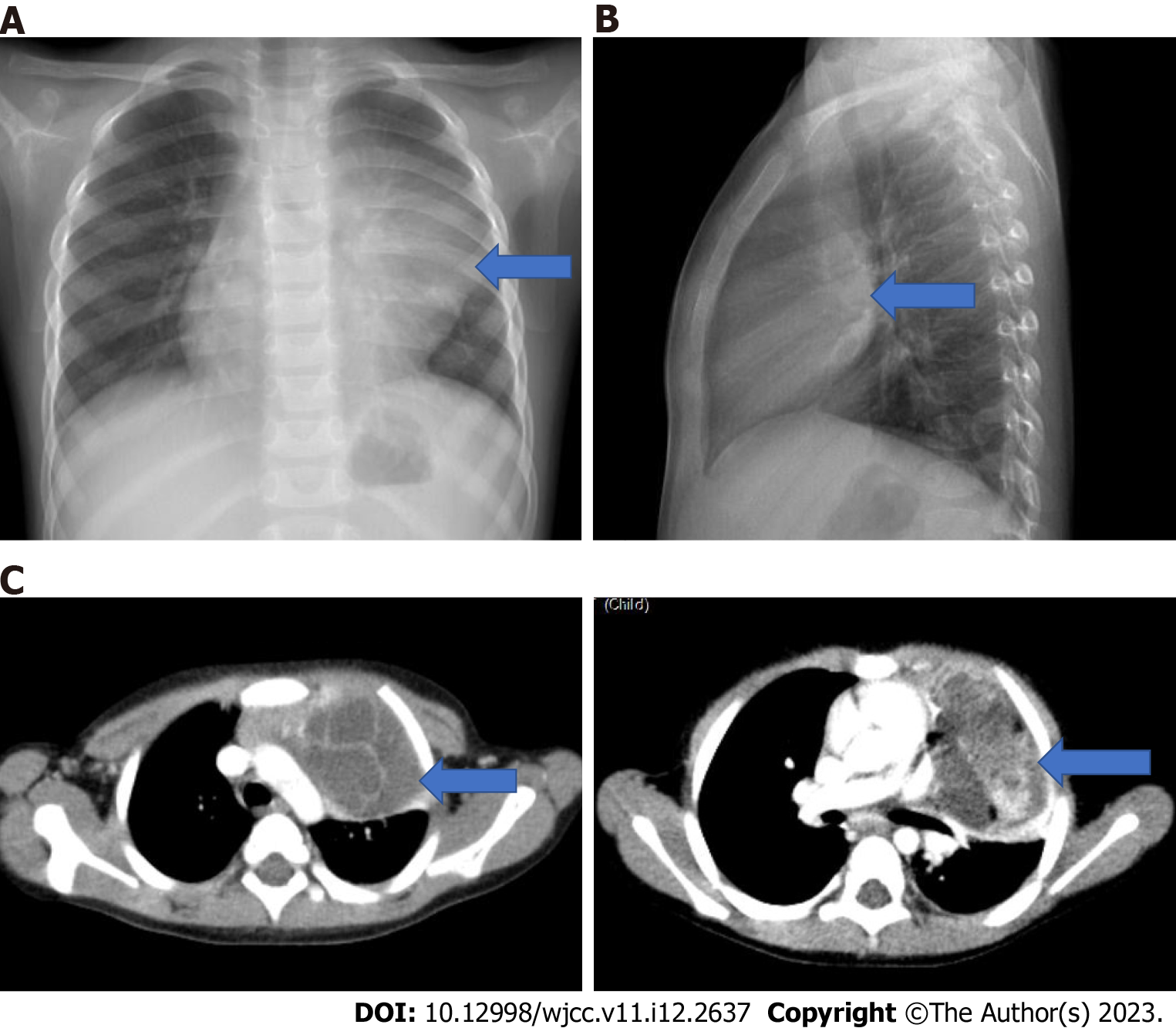
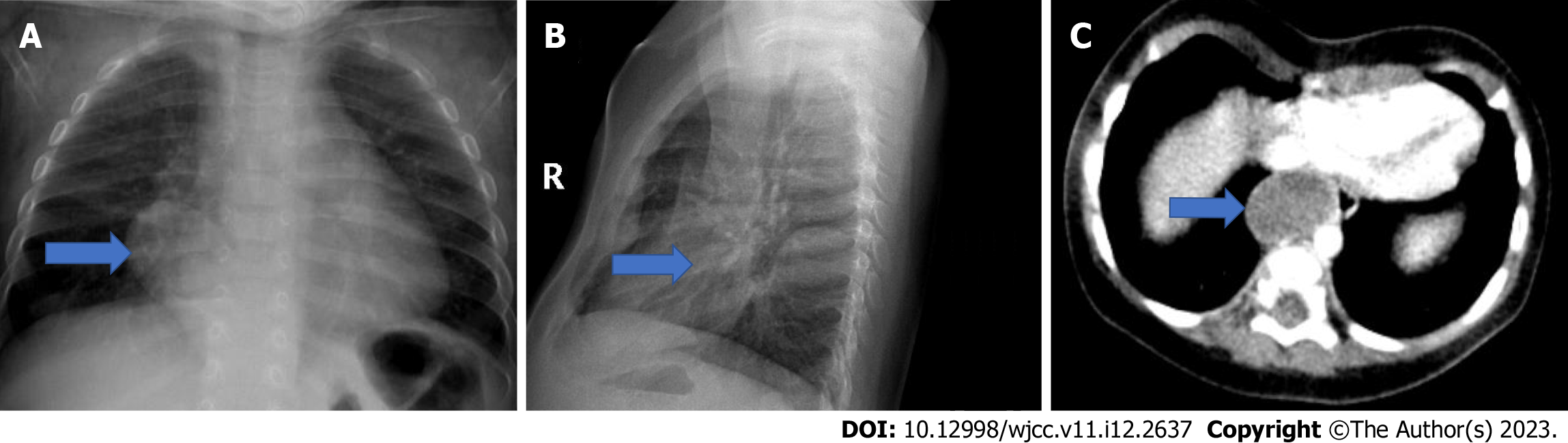
Figure 18 A 3-year-old girl with mature teratoma.
She presents with dyspnea. A: On the posteroanterior chest radiograph the mass (blue arrow) erases the contour of the hilus and heart on the left, slightly compresses the left main bronchus; B: It is located in the anterior mediastinum on the lateral X-ray (blue arrow); C: In the axial computed tomography images of the same patient, a septated mass lesion containing fluid, calcification and fat density (blue arrow) is located in the anterior mediastinum, it compresses the thymus and slightly compresses the left main bronchus. The mass also extends to the left side of the mediastinum.
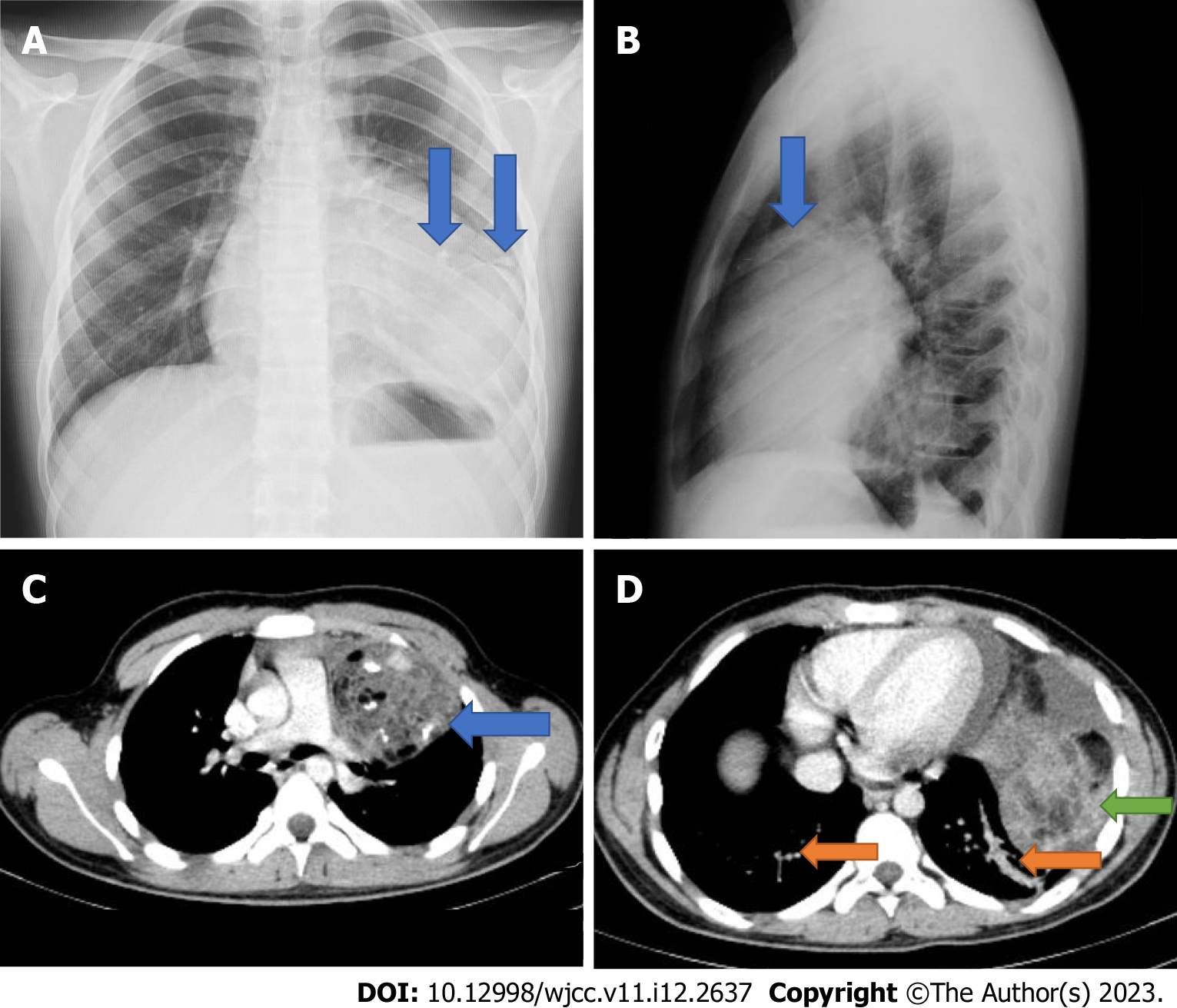
Figure 19 A 14-year-old male patient with Kleinefelter syndrome.
He has been complaining of pain in the left arm and shoulder for 3 d. A: Posteroanterior chest radiograph shows calcifications (double blue arrow) that erases the contour of the heart; B: Diaphragm on the left and the density of a mass located in the anterior mediastinum on the lateral radiograph (blue arrow); C: In the axial computed tomography images of the same patient, a lobulated mass lesion with calcification, fluid and fat densities, located in the left anterior mediastinum, adjacent to the thymus is observed (blue arrow); D: Pericardial and pleural effusion are present in the inferior slices of the same patient (green arrow). In addition, basal linear atelectasia is (double orange arrow).
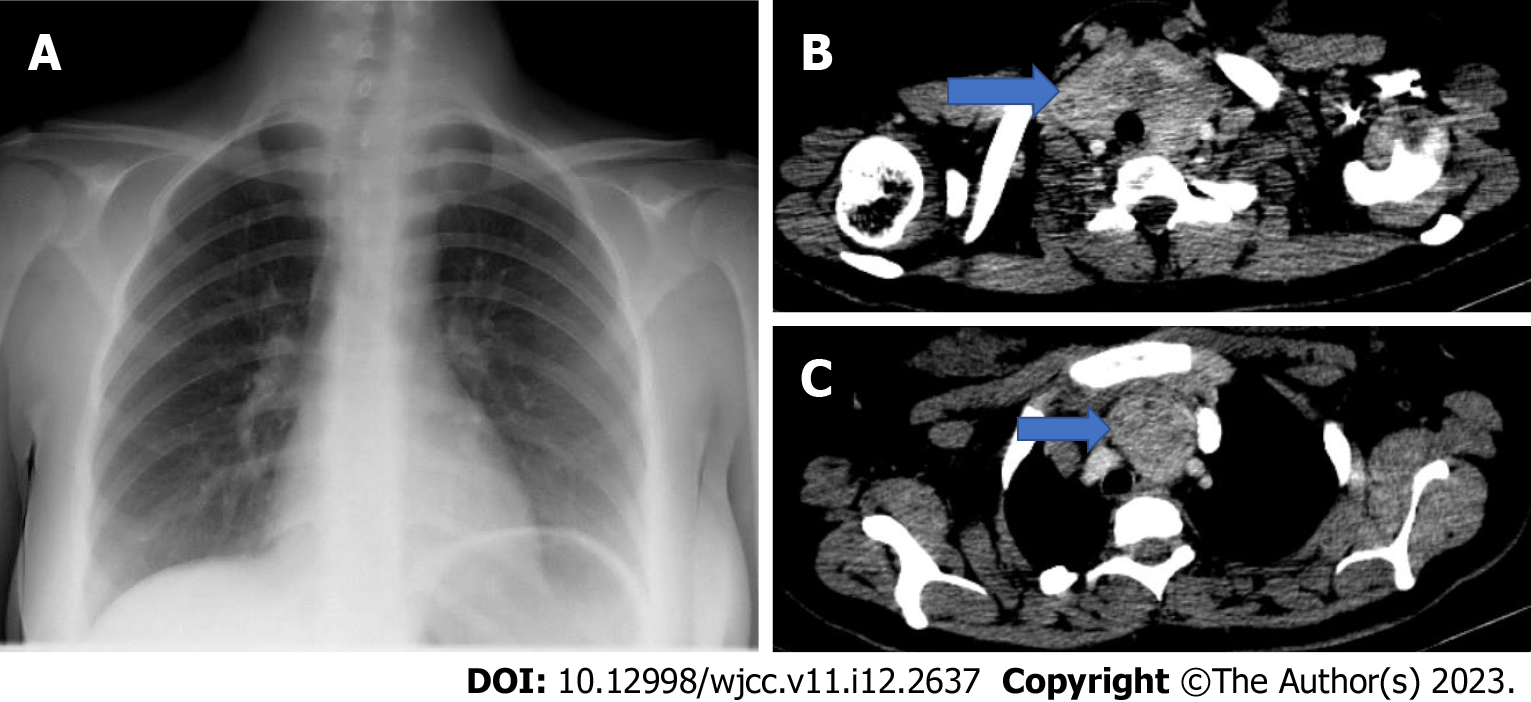
Figure 20 A 17-year-old girl with intrathoracic goiter.
A: In the posteroanterior chest radiograph of the patient followed up for multinodular goiter, enlargement in the upper mediastinum and a density that deviates the trachea to the right are observed. B and C: In axial computed tomography images (blue arrow), the thyroid gland is hyperplastic and contains nodules. In addition its extension is observed in the anterior mediastinum up to the superior aortic arch. Trachea is deviated to the right and no compression is detected.
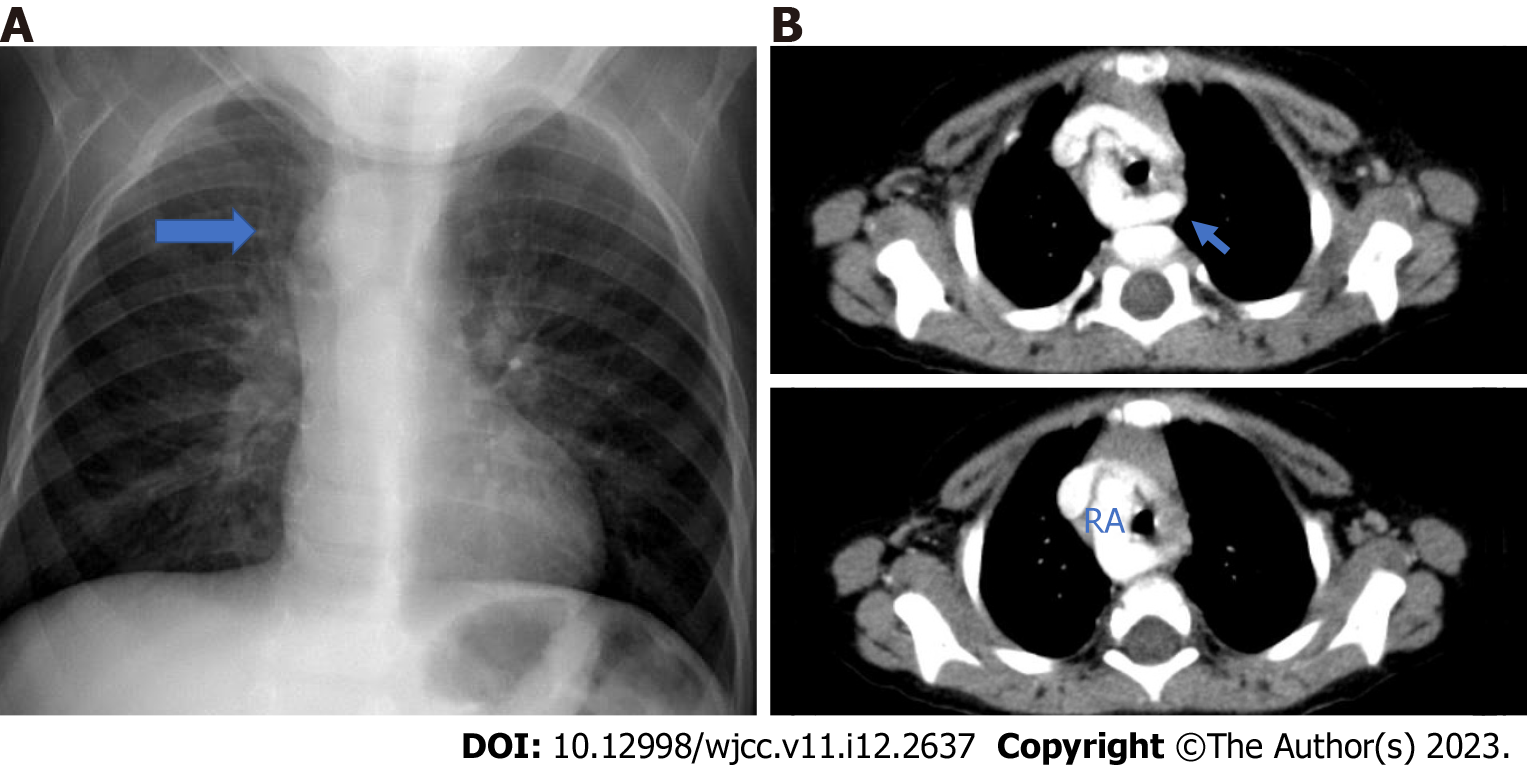
Figure 21 A 2-year-old male patient with right aortic arch.
A: There are complaints of shortness of breath and cough. On posteroanterior chest radiograph, enlargement of the upper mediastinum on the right and compression of the trachea are observed (blue arrow); B: Right aortic arch and left aberrant subclavian artery (blue arrow) are observed in the axial computed tomography angiography images of the same patient. RA: Right aortic arch.
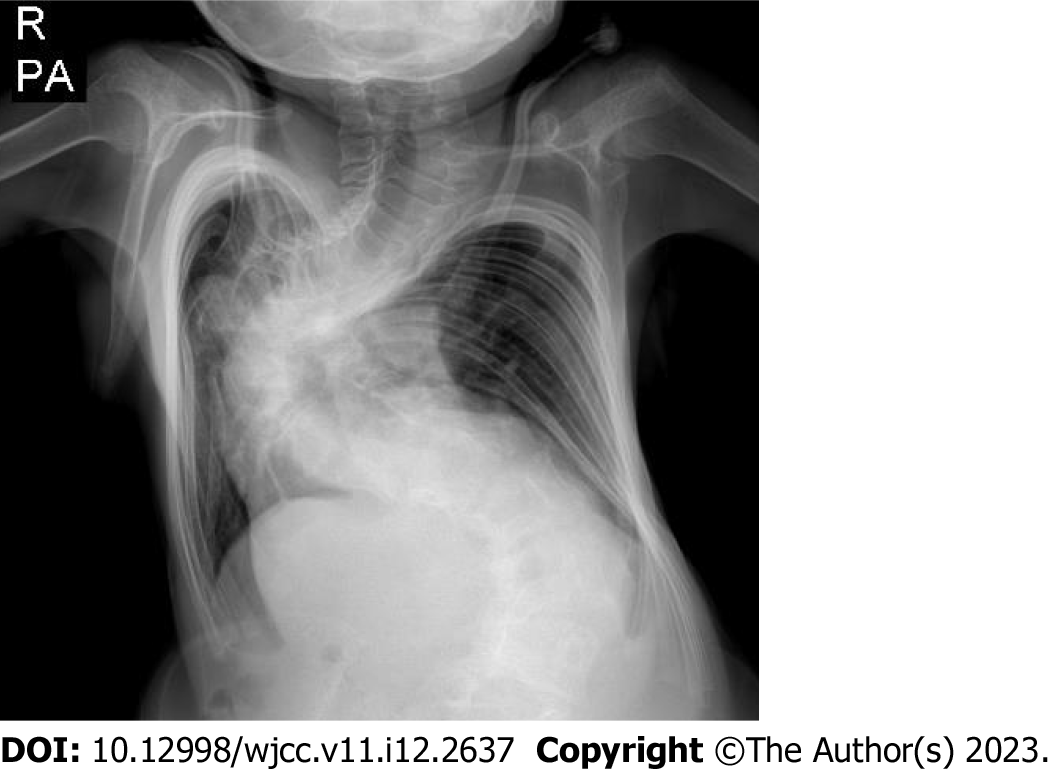
Figure 22 A 10-year-old male patient with Marfan syndrome.
There is mediastinal enlargement and rotoscoliosis in the thoracolumbar region on posteroanterior chest radiograph.
Figure 23 Aneurysmatic dilatation.
A: Aneurysmatic dilatation is observed in the aortic root in the axial; B: Coronal images in the computed tomography Angiography.
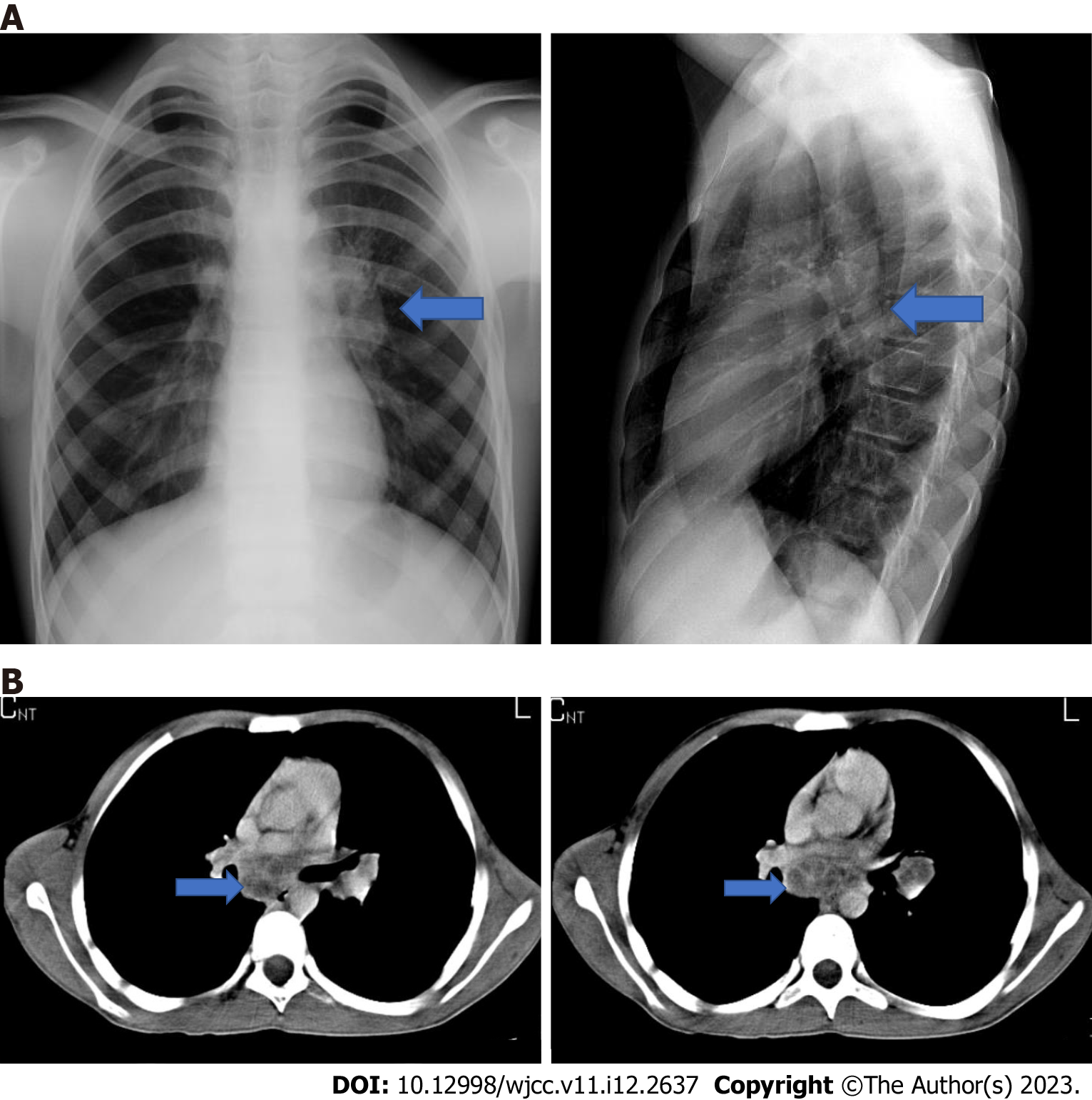
Figure 24 A 16-year-old male patient with tuberculosis.
A: There is fever and weight loss. Left hilar LAP is seen on bidirectional chest radiograph (blue arrow). B: Subcarinal and left hilar necrotic lymphadenopathies (blue arrow) are observed in the axial plane computed tomography examination of the same patient.
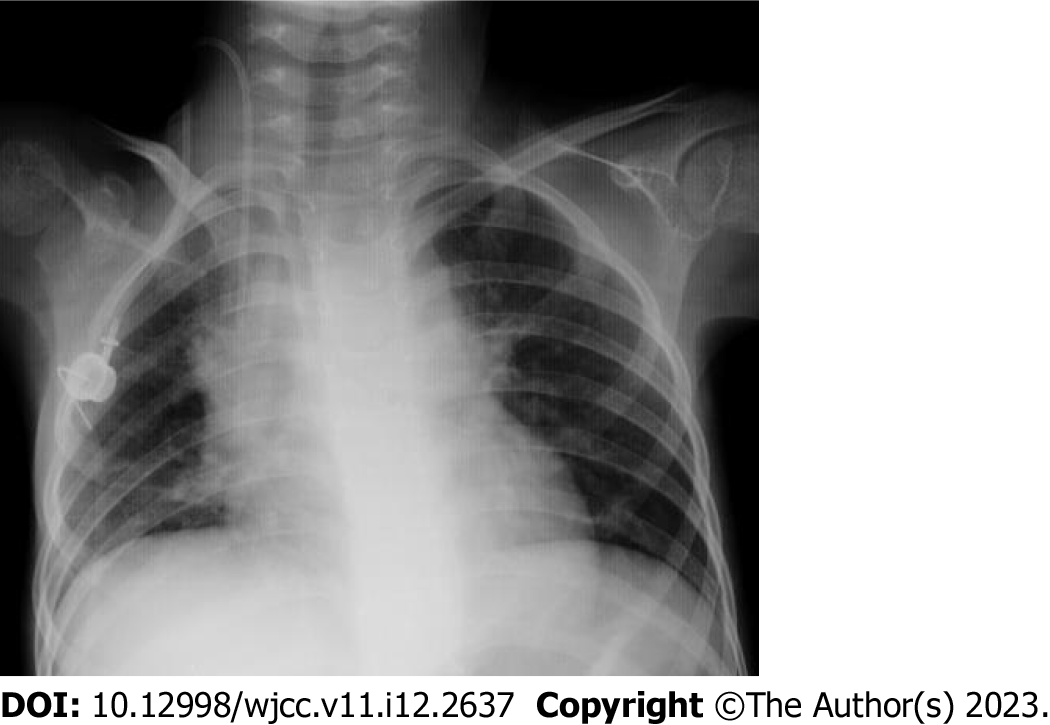
Figure 25 An 8-year-old female patient followed up with neuroblastoma.
Mediastinal enlargement and tracheal deviation are observed in posteroanterior chest radiograph.
Figure 26 The axial computed tomography images.
A and B: In the axial computed tomography images, necrotic lymphadenopathies (blue arrow) are present in paratracheal, precarinal and subcarinal areas; B: They deviate the trachea anteriorly and invade the left bronchus.
Figure 27 A 15-year-old female patient with bronchogenic cyst (blue arrow).
A 15-year-old female has a complaint of intermittent cough. Axial computed tomography images of the patient at different levels show a cyst located posterior to the right hilum (blue arrow).
Figure 28 A 6 mo old male patient.
A: On posteroanterior chest radiograph right paravertebral; B: Lateral radiograph posteriorly located smooth-contoured density (blue arrow) is observed; C: Esophageal duplication cyst (blue arrow). In the axial computed tomography images of the same patient, a lobulated contoured cyst is observed in the middle mediastinum, adjacent to the esophagus, and it extends into the posterior mediastinum.
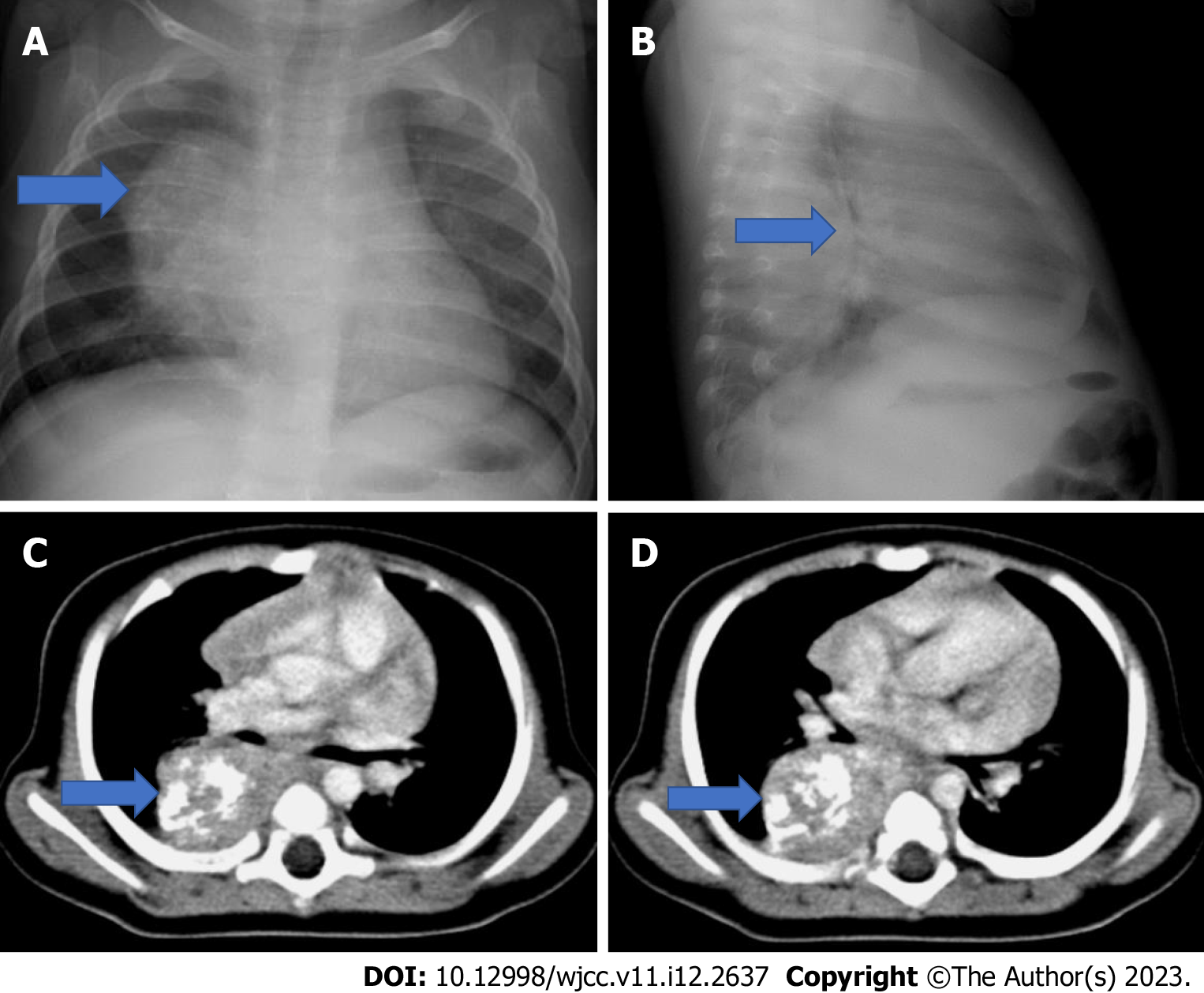
Figure 29 A 7 mo old girl with Neuroblastoma.
He is admitted to the hospital because of cough and wheezing. A: On posteroanterior chest radiograph (blue arrow) the mass is seen on the right paravertebral area; B: On the lateral radiograph a posteriorly located mass with a smooth outer contour and calcifications (blue arrow) is seen; C and D: In the axial computed tomography images of the same patient, a homogeneous mass with smooth contours and punctate-coarse calcifications (blue arrow) is observed in the paravertebral distance. The mass extends to the midline and mild compression is detected on the right main bronchus.
Figure 30 A 6-year-old female patient with Ganglioneuroma.
There is a cough complaint that has been going on for 3 mo. Posteroanterior chest radiograph shows a density (blue arrow) of paravertebral, well-contoured mass causing enlargement of the mediastinum on the right; B and C: In the axial and coronal computed tomography images of the same patient, a well-contoured, homogeneous mass (blue arrow) is observed in the paravetebral distance on the right.
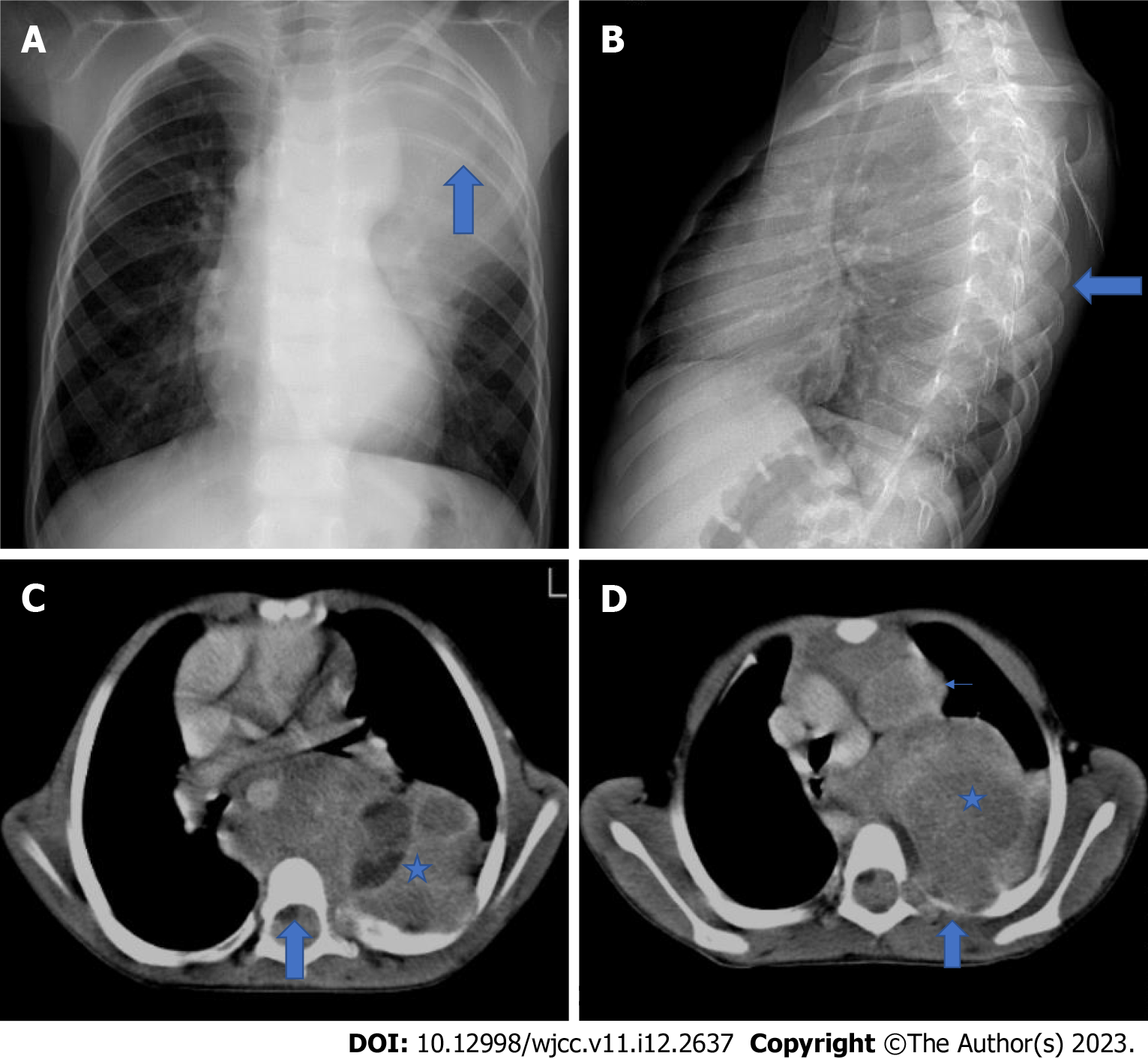
Figure 31 A 5-year-old girl with Ganglioneuroblastoma.
There are complaints of cough and left flank pain. A: A lobulated contoured mass lesion is observed in the Posteroanterior chest radiograph (blue arrow) that causes mediastinal enlargement on the left, deviates the trachea to the right; B: It is seen posteriorly on the lateral radiograph and causes erosion in the ribs (blue arrow); C and D: In the axial computed tomography images of the same patient, a heterogeneous mass lesion is seen (blue star).
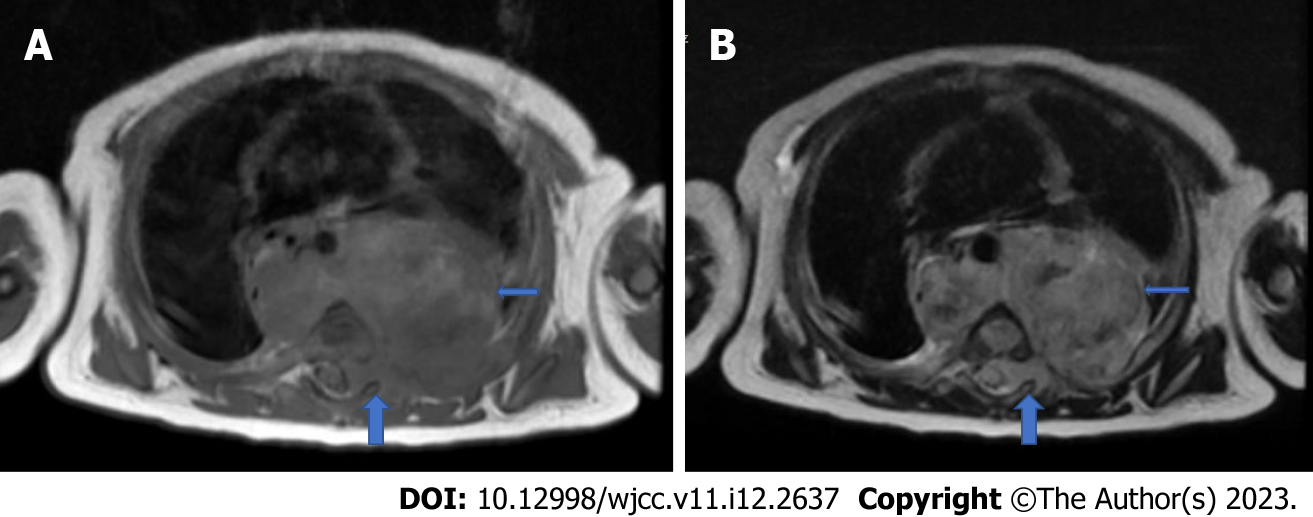
Figure 32 A 4-mo-old male patient diagnosed with neuroblastoma.
A: A heterogeneous mass is observed on both sides in the paravertebral area in T1W-weighted; B: T2W-weighted sections in the axial plane. The descending aorta is surrounded by the mass (thin blue arrow) and pushed anteriorly. It is also noteworthy that the mass invades the left neural foramen, extending into the spinal canal and compressing the spinal cord (A and B, thick blue arrow).
- Citation: Çinar HG, Gulmez AO, Üner Ç, Aydin S. Mediastinal lesions in children. World J Clin Cases 2023; 11(12): 2637-2656
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2637.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2637