Copyright
©The Author(s) 2022.
World J Clin Cases. Dec 6, 2022; 10(34): 12665-12670
Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12665
Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12665
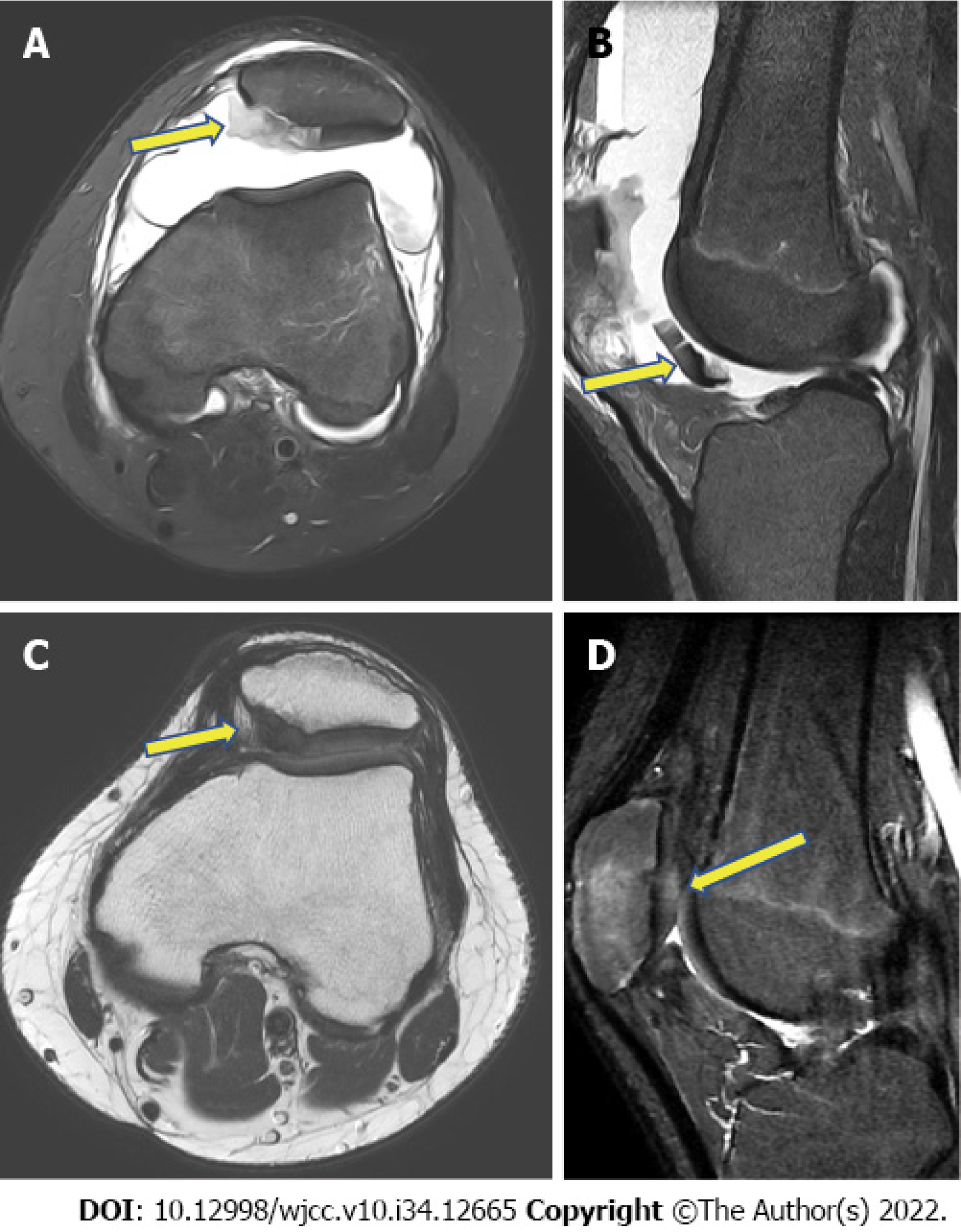
Figure 1 Magnetic resonance images.
A: T2-weighted, a fat-suppressed axial image showing a cartilage defect (arrow) on the medial side of the patella and patellar dislocation with a medial patellofemoral ligament tear; B: T2-weighted, a fat-suppressed sagittal image showing a large amount of hemarthrosis and detached patellar cartilage (arrow) in the infrapatellar area; C: Proton density axial image showing regeneration of the patellar cartilage (arrow) and a normal patellar position, with the healing of the medial patellofemoral ligament, 18 mo after surgery; D: Proton fat-suppressed sagittal image showing patellar cartilage regeneration (arrow) 18 mo after surgery.
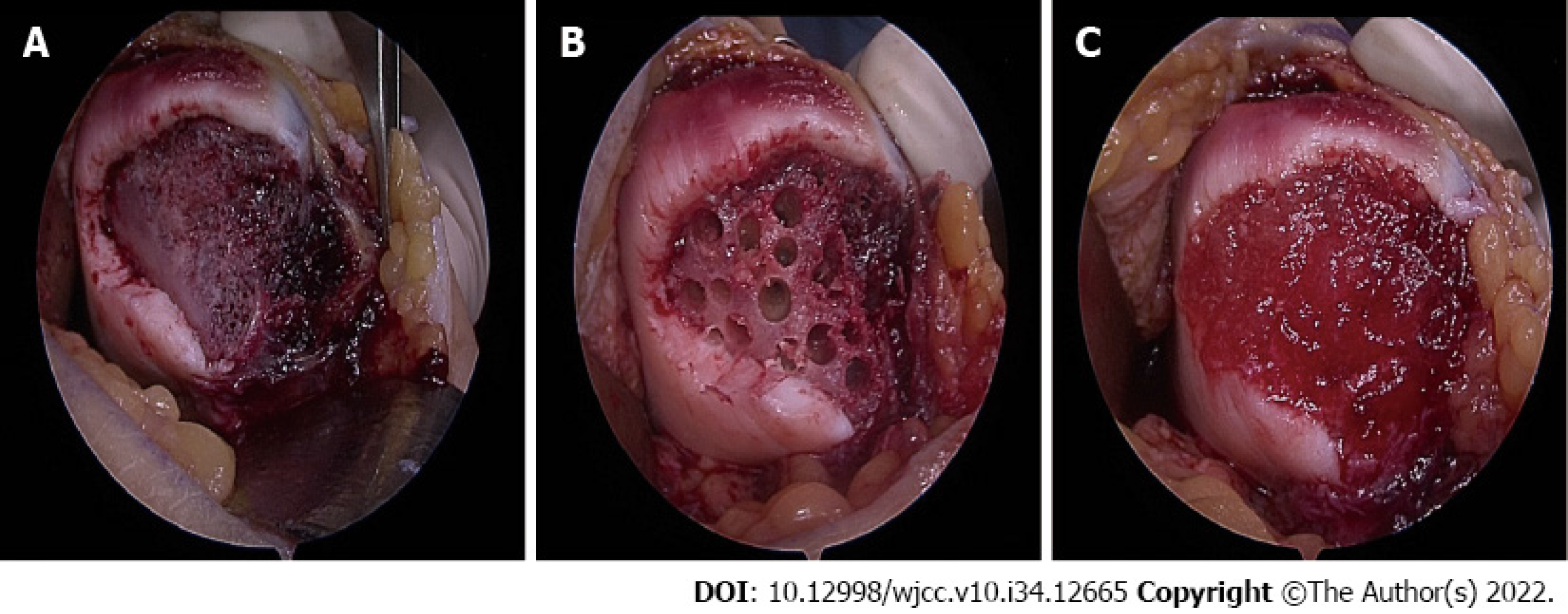
Figure 2 Surgical procedures of the patellar defect.
A: Exposed large subchondral bone on the medial patellar facet; B: After multiple drillings on the subchondral bone; C: After implantation of the human umbilical cord, blood-derived mesenchymal stem cells into the defect.
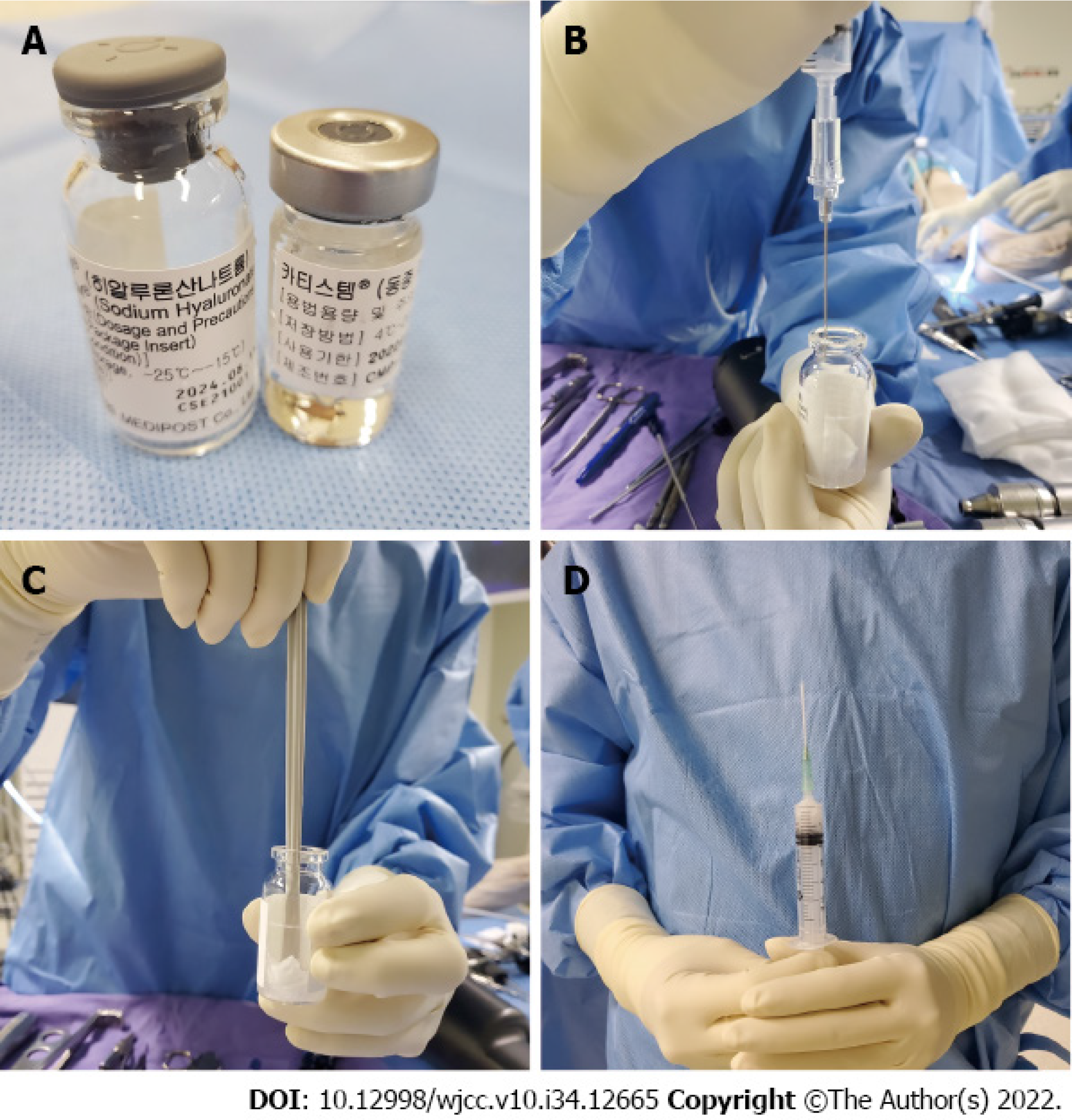
Figure 3 Stem cell product preparation.
A: The left vial contains hyaluronic acid, and the right vial contains hUCB-MSCs; B: Aspirated hUCB-MSCs are injected into the hyaluronic acid vial; C: The hUCB-MSCs with hyaluronic acid are mixed; D: The mixture of hUCB-MSCs and hyaluronic acid is transferred into a syringe.
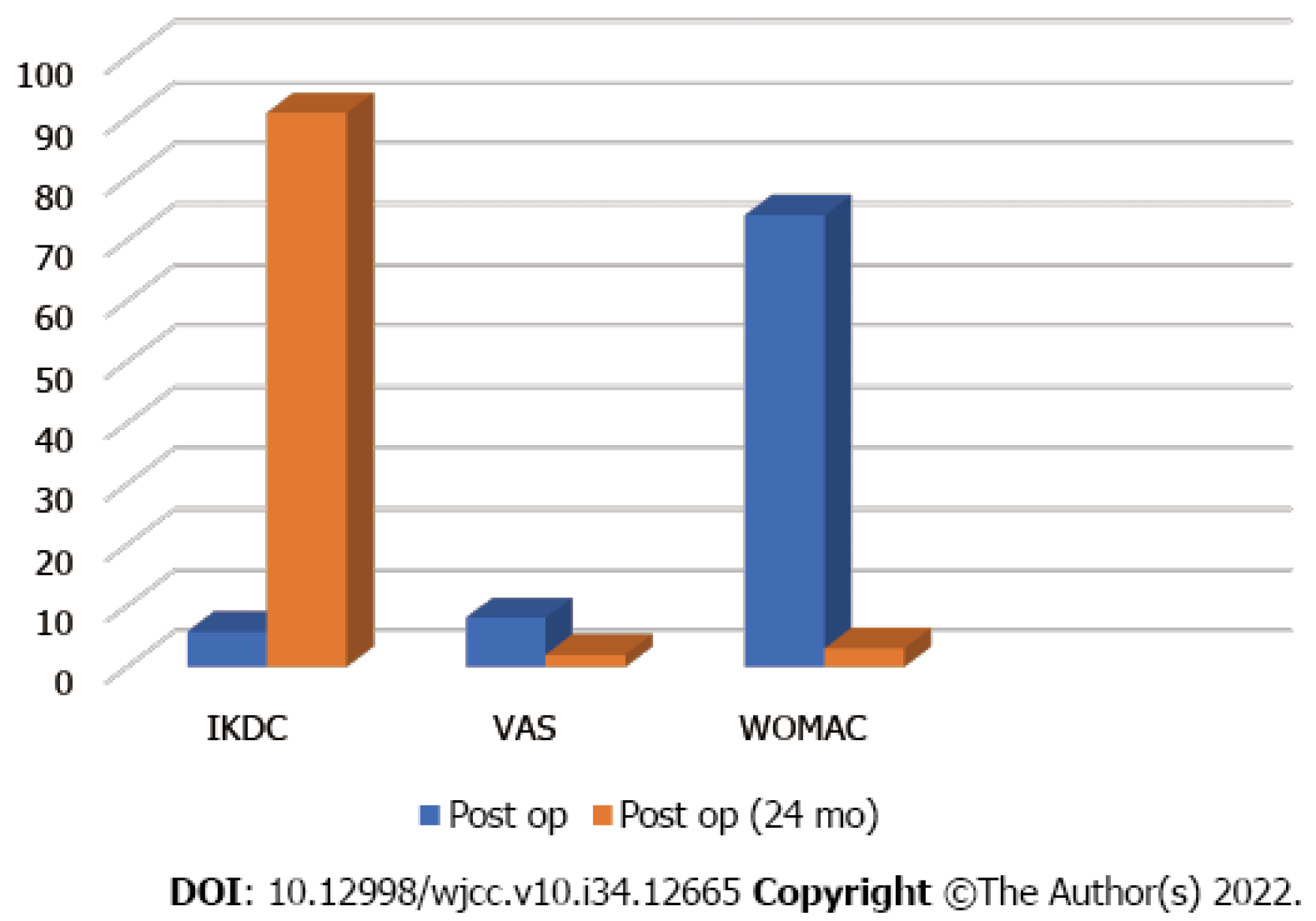
Figure 4 Clinical improvement.
Visual analog scale, International Knee Documentation Committee (IKDC), visual analog scale (VAS), and McMaster Universities Osteoarthritis Index (WOMAC) scores show clinical improvement 2 years after human umbilical cord blood-derived mesenchymal stem cell implantation.
- Citation: Song JS, Hong KT, Song KJ, Kim SJ. Repair of a large patellar cartilage defect using human umbilical cord blood-derived mesenchymal stem cells: A case report. World J Clin Cases 2022; 10(34): 12665-12670
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12665.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12665