Copyright
©The Author(s) 2022.
World J Clin Cases. Jan 21, 2022; 10(3): 811-819
Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.811
Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.811
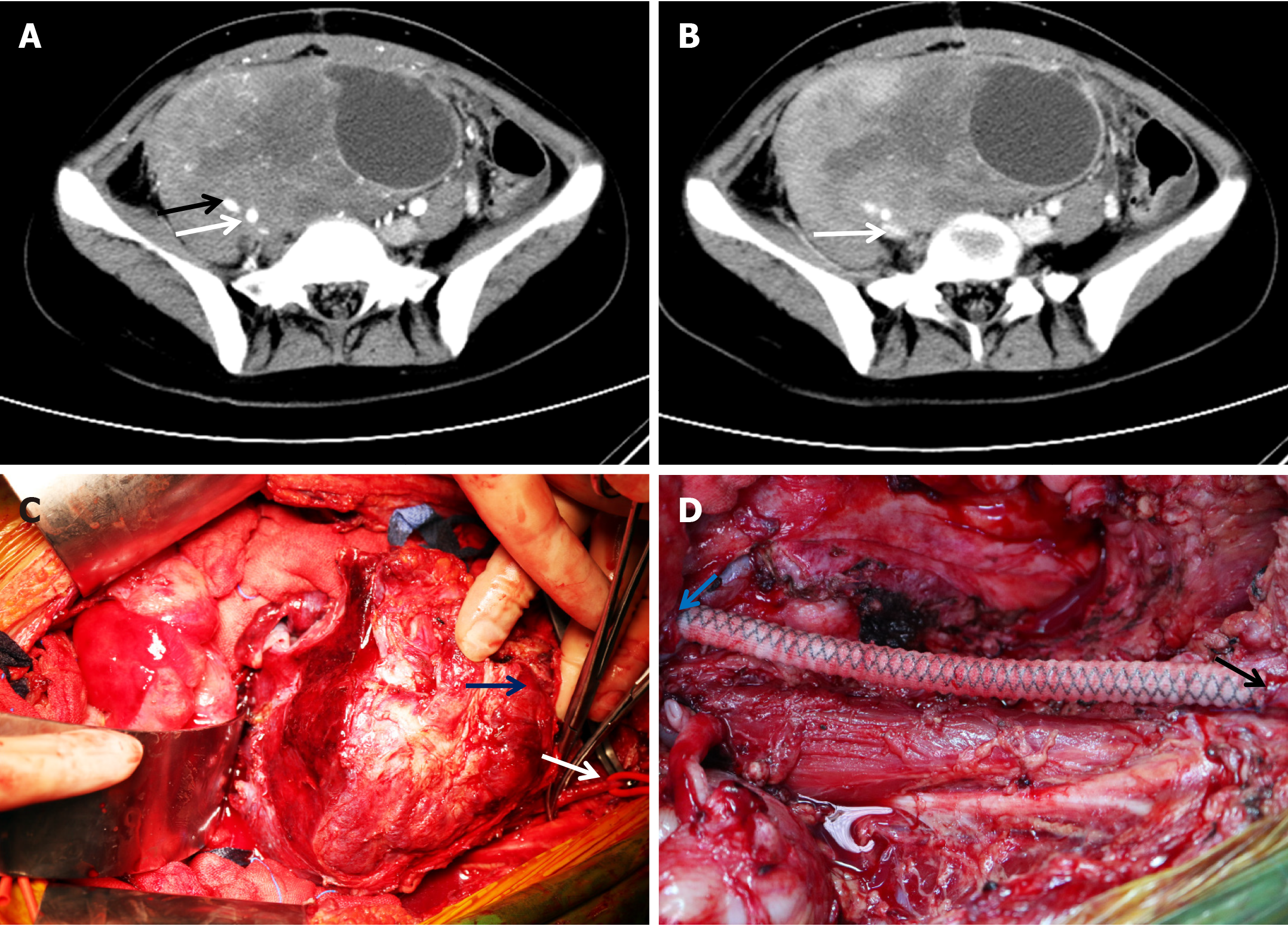
Figure 1 Computed tomography images from a case of retroperitoneal invasive fibroma and key steps in surgery.
A: The arterial phase of the computed tomography (CT) scan indicated a massive pelvic mass with a diameter of approximately 20 cm surrounding the right internal iliac artery (white arrow) and external iliac artery (black arrow); B: The venous phase of the CT scan indicated that the mass surrounded the right common iliac vein and caused compression occlusion (arrow); C: During surgery, the right femoral artery (white arrow) was dissociated; the blue arrow indicates the mass; D: Artificial vessel reconstruction between the right common iliac artery (blue arrow) and femoral artery (black arrow) was performed after tumor removal.
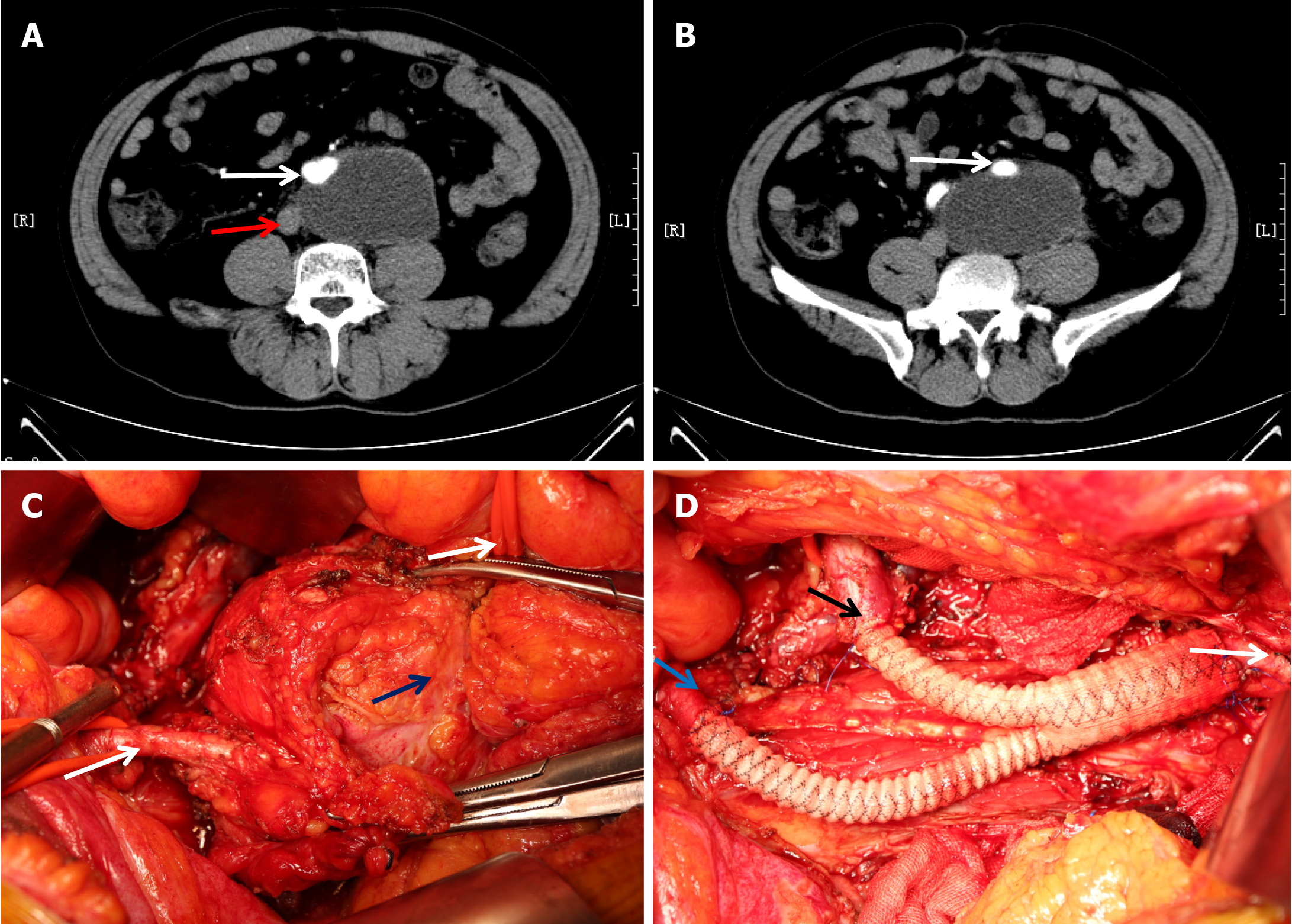
Figure 2 Computed tomography images of a case of myxofibrosarcoma and key steps in the surgery.
A: A layer of the arterial phase of the computed tomography scan indicated a retroperitoneal mass with a diameter of approximately 9 cm surrounding the abdominal aorta (white arrow) and adherent to the inferior vena cava (red arrow); B: Another layer indicated that the mass surrounded the left common iliac artery (white arrow); C: During surgery, the left external iliac artery (lower left arrow) and abdominal aorta (upper right arrow) were dissociated; the blue arrow indicates the mass; D: “Y-type” artificial vascular reconstruction of the abdominal aorta (white arrow), right common iliac artery (black arrow), and left external iliac artery (blue arrow) was performed after tumor removal.
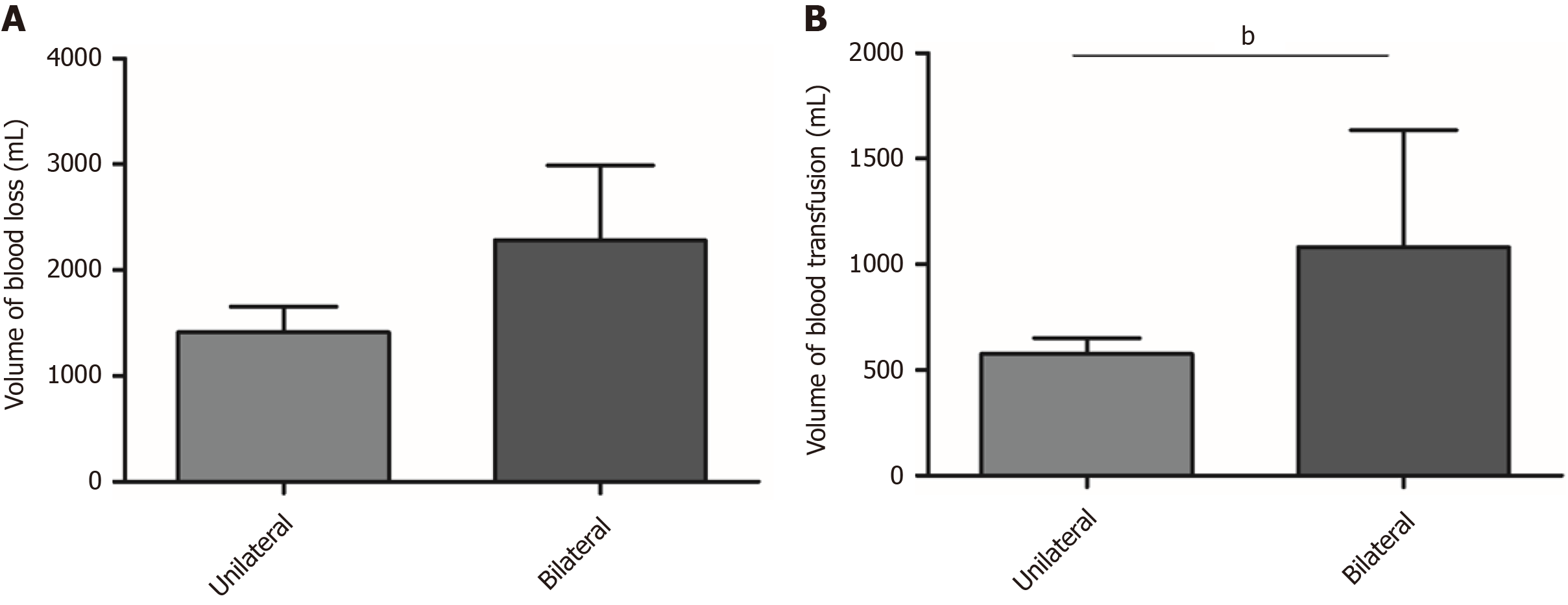
Figure 3 Differences in blood loss and transfusion volume based on the pattern of iliac artery reconstruction.
A: No statistically significant difference was found in the volume of blood loss between the unilateral and bilateral iliac artery reconstruction groups (P = 0.06); B: The volume of transfused blood was significantly higher for patients who received bilateral iliac artery reconstruction than for those who received unilateral iliac artery reconstruction (bP < 0.001).
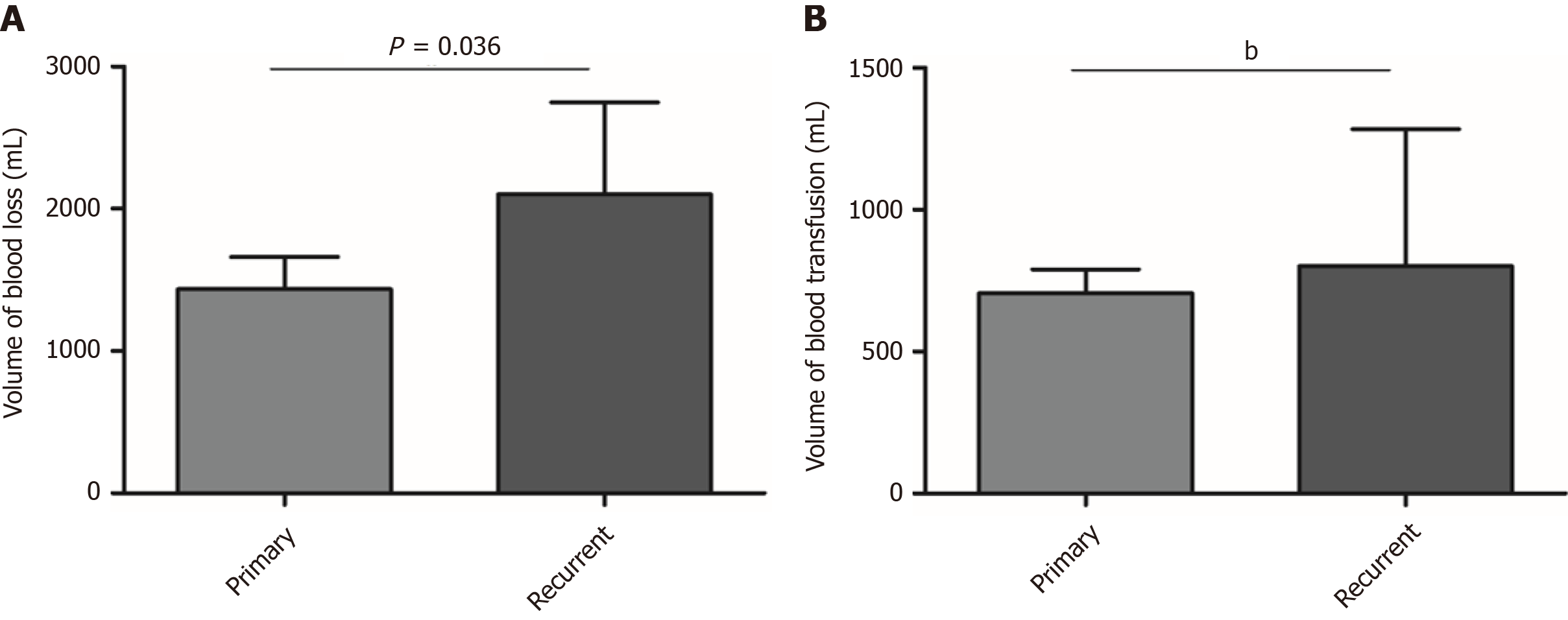
Figure 4 Differences in blood loss and transfusion volume between primary and recurrent cases.
A: The volume of bleeding was significantly increased for patients with recurrent disease (P = 0.036); B: The volume of transfused blood was significantly higher for recurrent cases than for primary cases (bP < 0.001).
- Citation: Li WX, Tong HX, Lv CT, Yang H, Zhao G, Lu WQ, Zhang Y. Management of retroperitoneal sarcoma involving the iliac artery: Single-center surgical experience. World J Clin Cases 2022; 10(3): 811-819
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/811.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.811