Copyright
©The Author(s) 2022.
World J Clin Cases. Jul 26, 2022; 10(21): 7422-7428
Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7422
Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7422
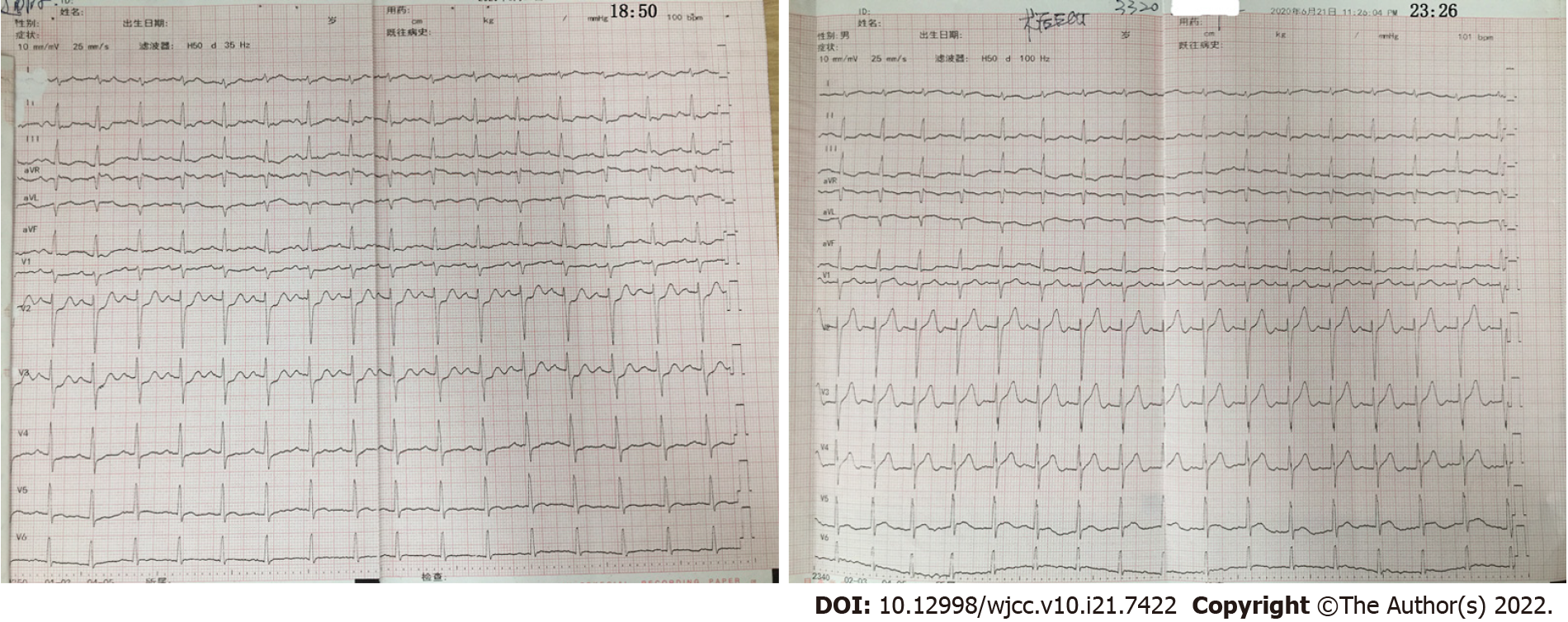
Figure 1 Preoperative and postoperative electrocardiograms.
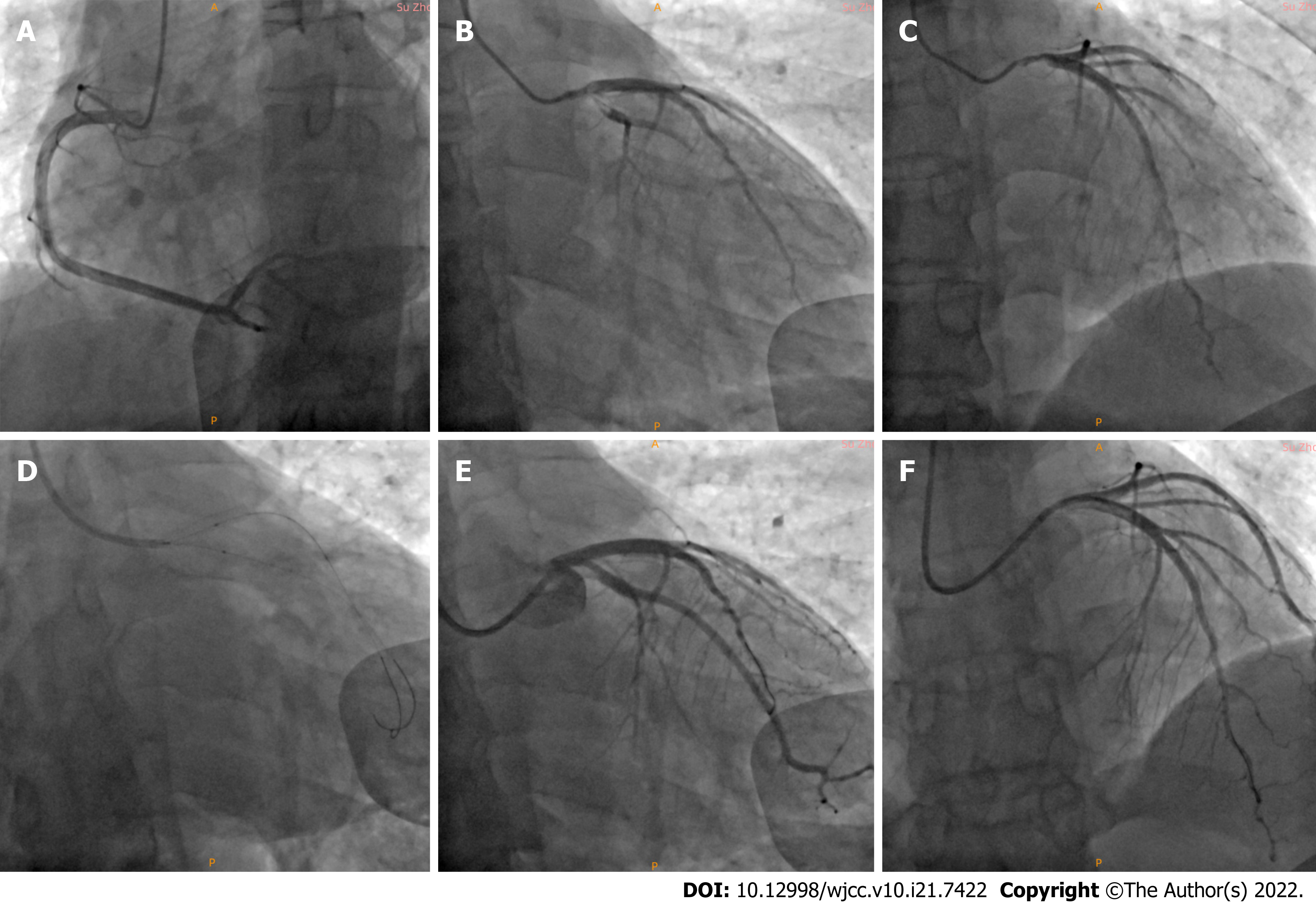
Figure 2 Coronary angiography and percutaneous coronary intervention.
A: There was no obvious stenosis in the right coronary artery; B and C: Left main (LM) bifurcation lesion with a Medina classification of 1%, 0%, 1%, 60% diffuse stenosis in the LM that extended to the ostial left anterior descending (LAD), 30% stenosis in the ostial LAD, thrombosis of the ostial LAD and proximal left circumflex (LCX), 90% stenosis in the proximal LCX, and coronary slow flow in the obtuse marginal (OM); D: Final kissing balloon technique was performed; E and F: Finally, LM showed great expansion after stent treatment, and the thrombus load was significantly decreased in the ostial and proximal LCX. There was 60% residual stenosis in the ostial LCX, with a thrombolysis in myocardial infarction flow grade of 3 in the OM. The ostial LAD showed great expansion after stent treatment.
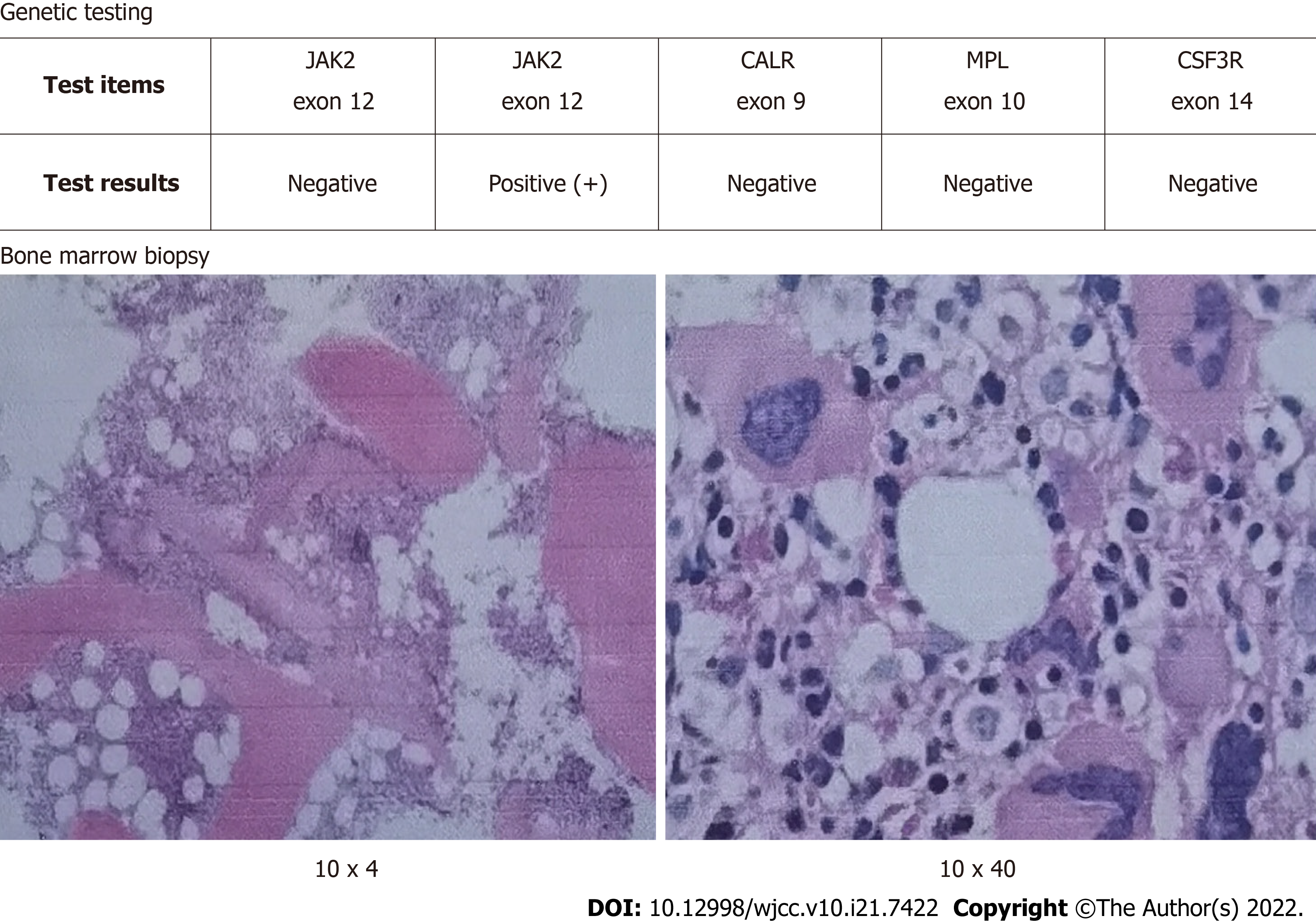
Figure 3 Genetic testing showed that the presence of a JAK2 (exon 14) V617F mutation.
The bone marrow biopsy showed that bone marrow hyperplasia was significantly active, the granulocyte/nucleated red blood cell ratio was normal, and megakaryocytes were common.
- Citation: Wang ZM, Chen WH, Wu YM, Wang LQ, Ye FL, Yin RL. Essential thrombocythemia with non-ST-segment elevation myocardial infarction as the first manifestation: A case report. World J Clin Cases 2022; 10(21): 7422-7428
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7422.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7422