Copyright
©The Author(s) 2022.
World J Clin Cases. Jul 16, 2022; 10(20): 7138-7146
Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7138
Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7138
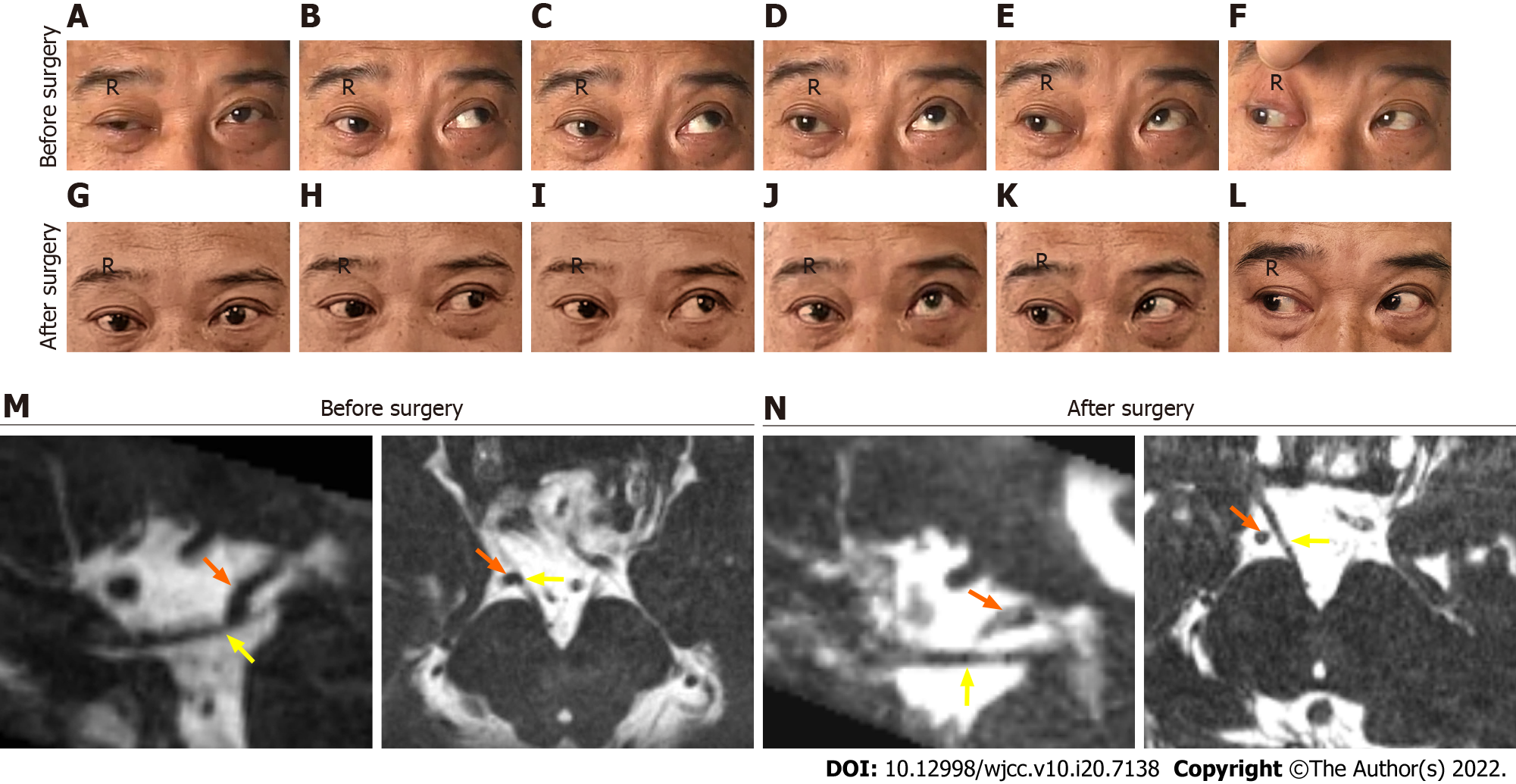
Figure 1 Right ocular motility in different directions of gaze is compared before and after surgery (3 months).
A-F: Showing the deficits in primary position (A), adduction (B), medial-to-upper left (C), elevation (D), and medial-to-upper right (E) except abduction (F); G-L: Demonstrating a good recovery from the right oculomotor nerve palsy with mild deficits in elevation. The representative axial (right) and sagittal (left) T2-weighted image before surgery (M) showing that the right oculomotor nerve (ON) (yellow arrow) was in direct contact with the right posterior cerebral artery (PCA) (orange arrow). The representative axial (right) and sagittal (left) T2-weighted image at 3 mo after surgery (N) showing that there was no contact between PCA and ON.
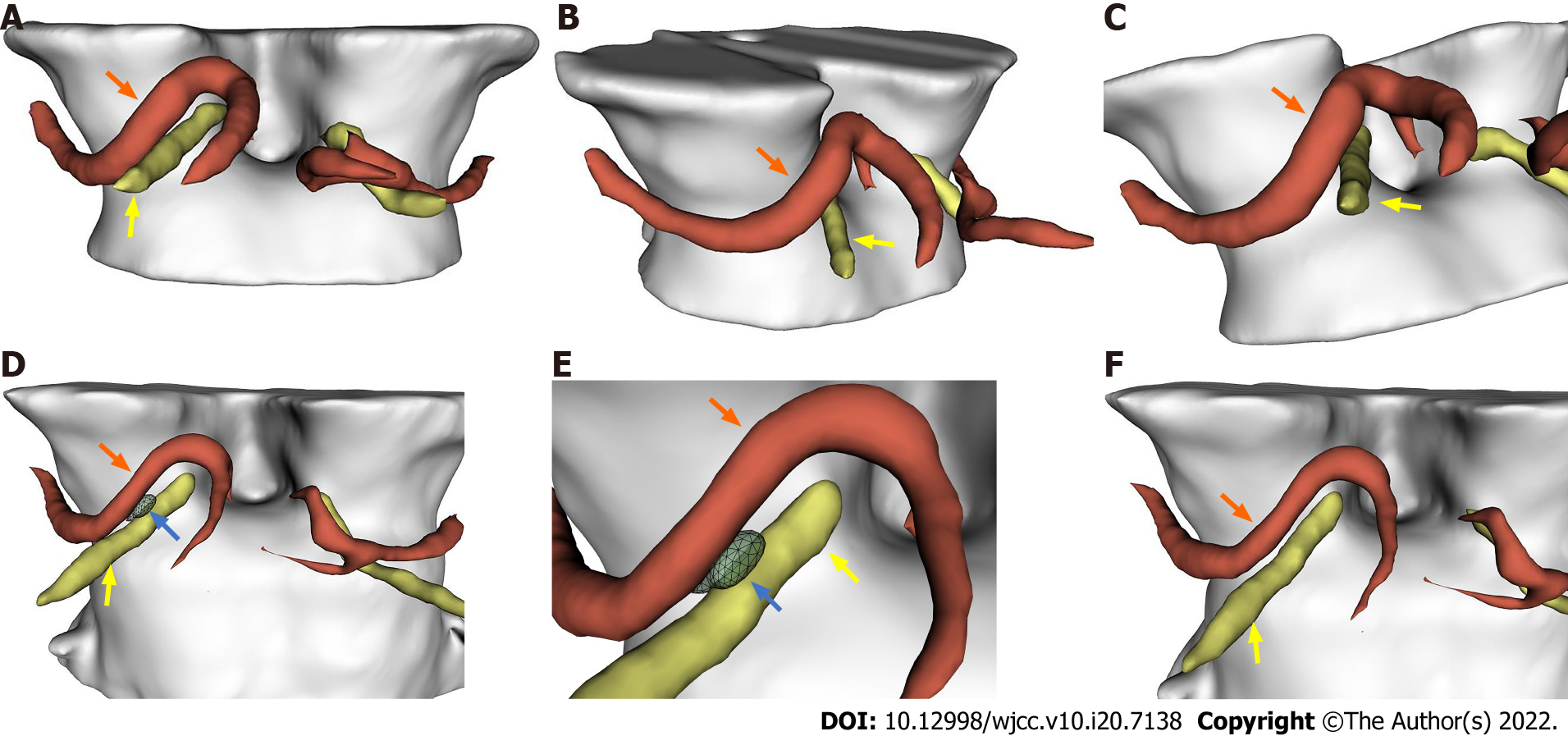
Figure 2 Representative three-dimensional images.
A-C: Demonstrated the right oculomotor nerve (ON) (yellow arrow) was compressed by the right posterior cerebral artery (PCA) (orange arrow) downwardly before surgery; D-F: Demonstrated the decompression of the right oculomotor nerve by the Telfon cottons (blue arrow) between the right PCA and the right oculomotor nerve 3 mo after surgery.
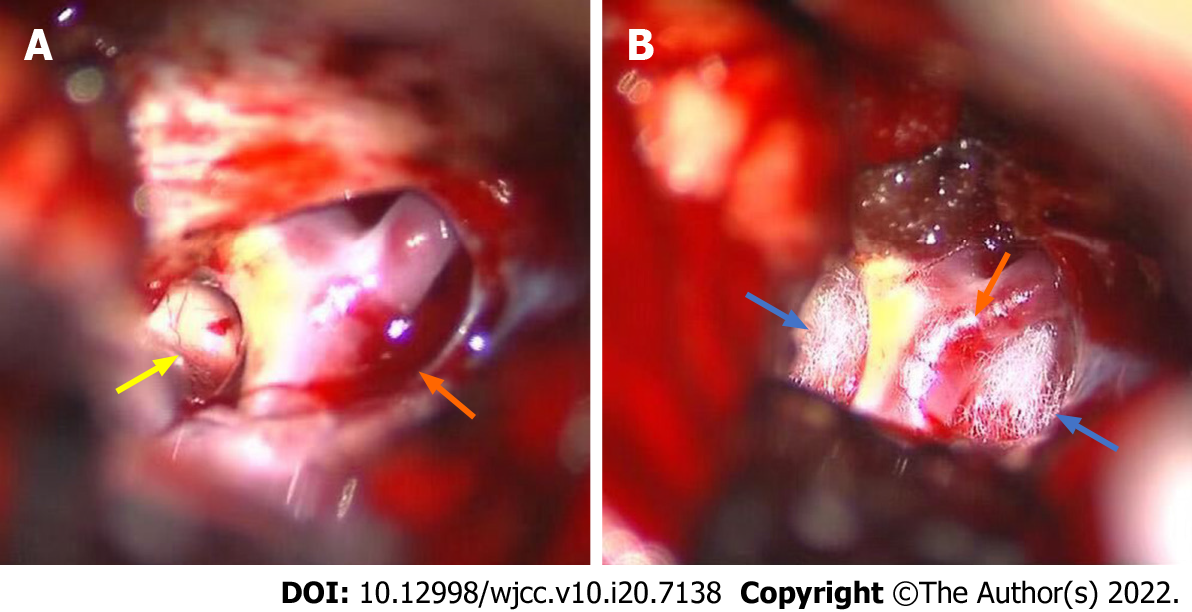
Figure 3 Intraoperative microsurgical view after separating the tense arachnoid membrane and coating of the right posterior cerebral artery.
A: The right posterior cerebral artery (PCA) (orange arrow) compressing the oculomotor nerve (yellow arrow); B: Teflon cotton (yellow arrow) used to cushion the oculomotor nerve against the PCA.
- Citation: Zhang J, Wei ZJ, Wang H, Yu YB, Sun HT. Microvascular decompression for a patient with oculomotor palsy caused by posterior cerebral artery compression: A case report and literature review . World J Clin Cases 2022; 10(20): 7138-7146
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7138.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7138