Copyright
©The Author(s) 2022.
World J Clin Cases. Jul 16, 2022; 10(20): 6991-6998
Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6991
Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6991
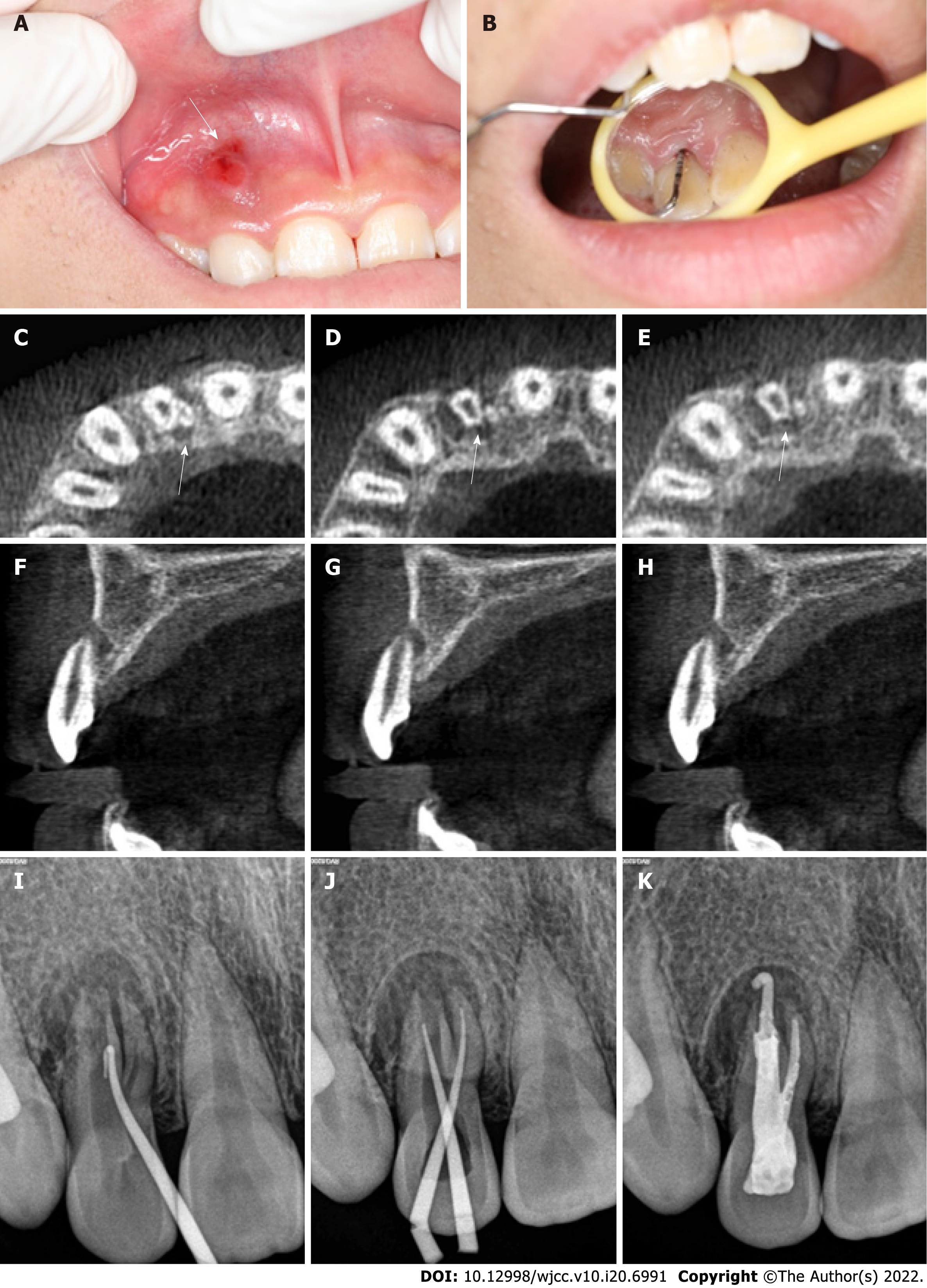
Figure 1 Oral examination and imaging examination before surgery.
A: Visual examination revealed a draining sinus tract on the labial gingival surface associated with the maxillary right lateral incisor; B: Periodontal probing depth of the involved tooth was 13 mm; C-H: Cone-beam computed tomography showed that the maxillary right lateral incisor had two roots with a large area of periradicular radiolucency; I: Preoperative radiography showing that gutta percha was used to trace the sinus tract; J: Intraoral radiography immediately after root canal preparation; K: Intraoral radiography immediately after root canal therapy.
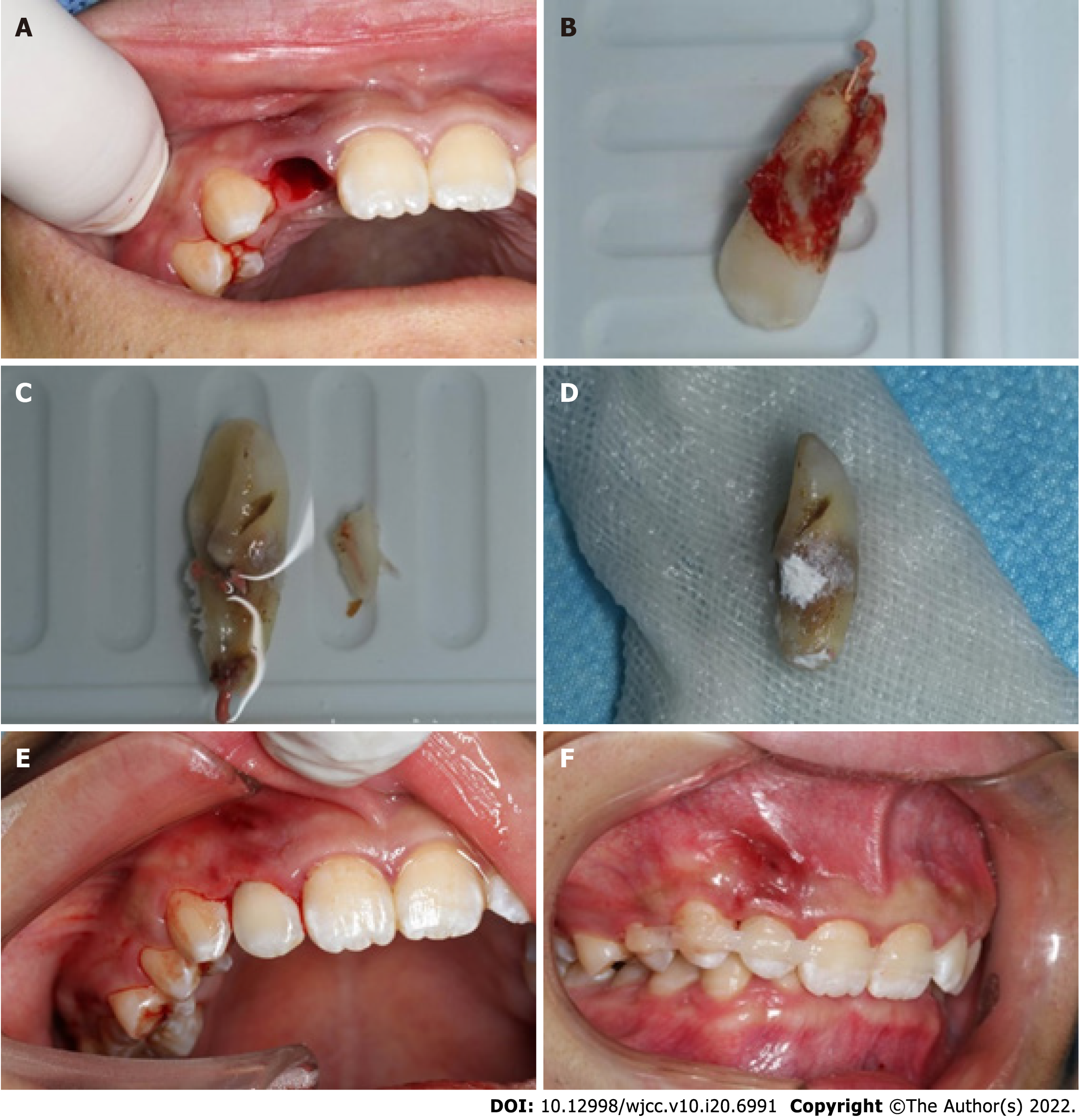
Figure 2 Basic steps of the surgery.
A: The tooth was extracted atraumatically with forceps, and the periodontal ligament remained intact; B: Palatogingival groove extended up to the root apex, and divided into two independent roots; C: The small root was removed with a fissure bur; D: Root tips were backfilled with iRoot BP Plus Root Repair Material; E: The tooth was replanted into its alveolar bone; F: The tooth was splinted with a flexible splint for 1 wk.
Figure 3 Oral examination and imaging examination during the 1-year follow-up.
A-C: The sinus tract was significantly reduced at the 1-wk postoperative visit; D-F: At the 1-mo recall, the sinus tract was closed and radiography showed a reduction in the periapical lesion, and the depth of the periodontal probe was 3 mm; G-I: At the 3-mo recall, radiography showed no periapical lesion, and the tooth was asymptomatic with no periodontal pocket; J-L: Radiography was performed immediately after operation at the 1-wk, 1-mo, 3-mo, 6-mo, and 12-mo recalls, which showed that the periradicular radiolucency gradually narrowed (M, P, Q).
- Citation: Tan D, Li ST, Feng H, Wang ZC, Wen C, Nie MH. Intentional replantation combined root resection therapy for the treatment of type III radicular groove with two roots: A case report. World J Clin Cases 2022; 10(20): 6991-6998
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/6991.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.6991