Copyright
©The Author(s) 2022.
World J Clin Cases. Jul 16, 2022; 10(20): 6769-6783
Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6769
Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6769
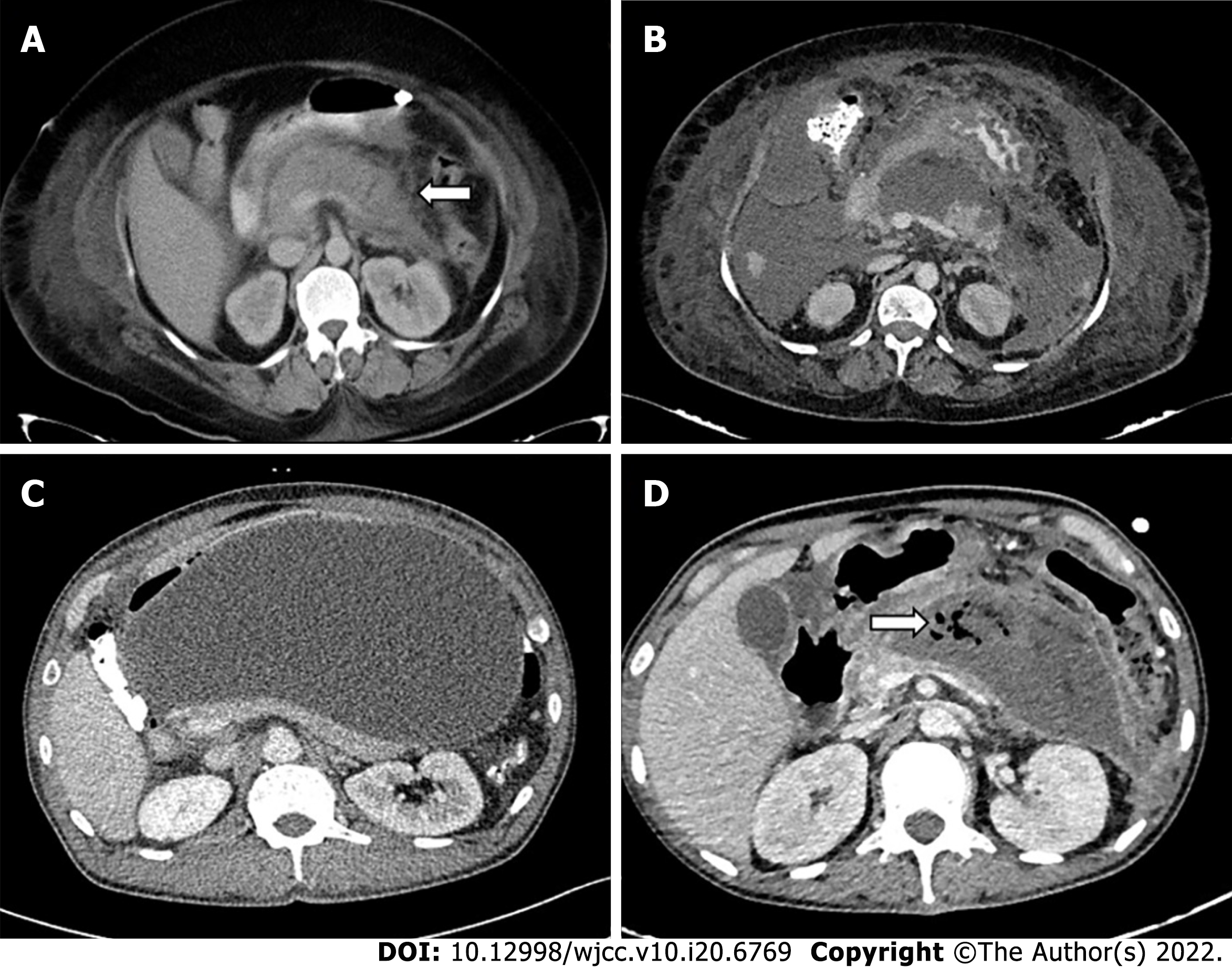
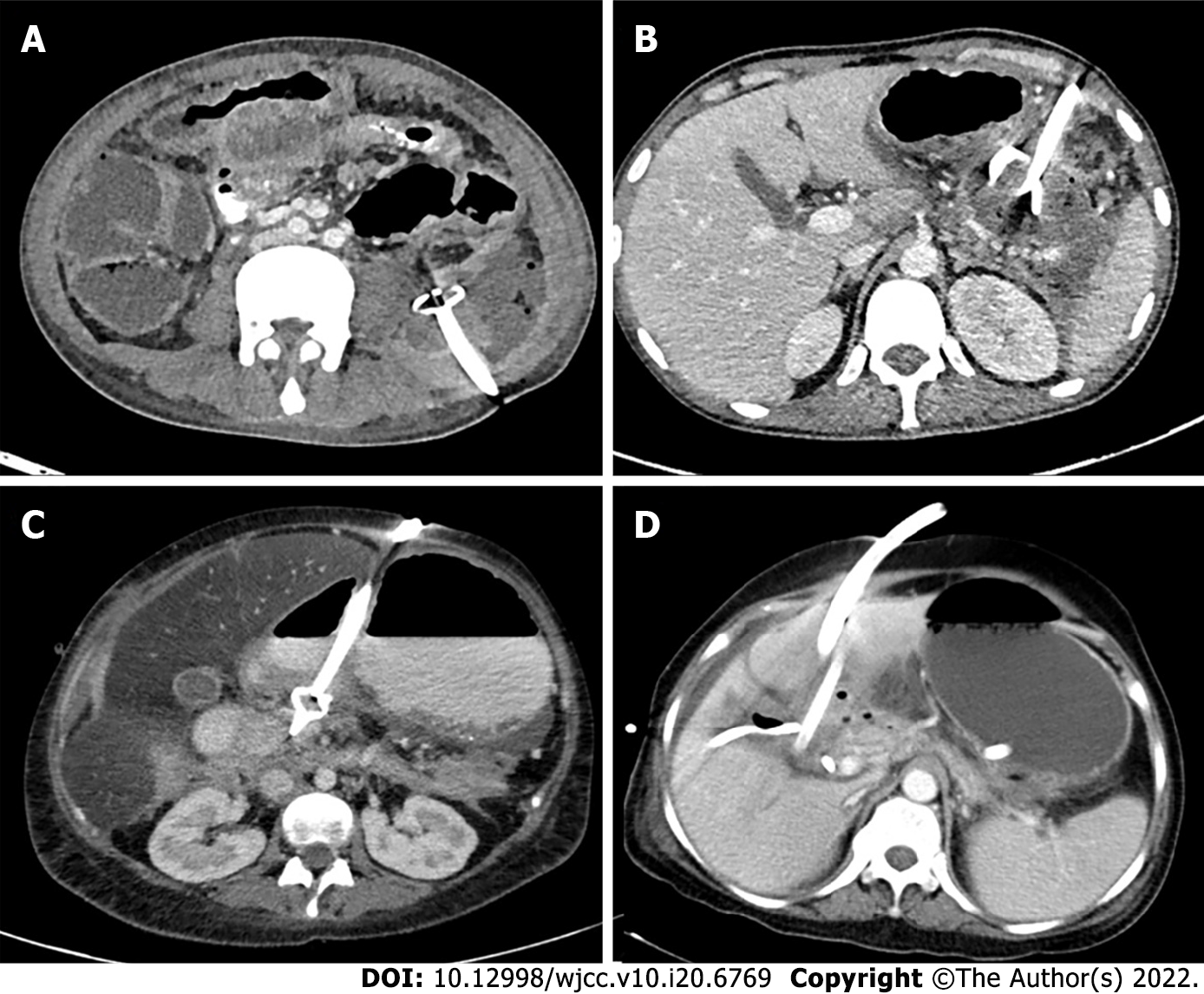
Figure 1 Various types of pancreatic fluid collections according to revised Atlanta classification.
A: Acute peripancreatic fluid collection (arrow); B: Acute necrotic collection; C: Pseudocyst; D: Walled off necrosis with air foci (arrow) in the collection.
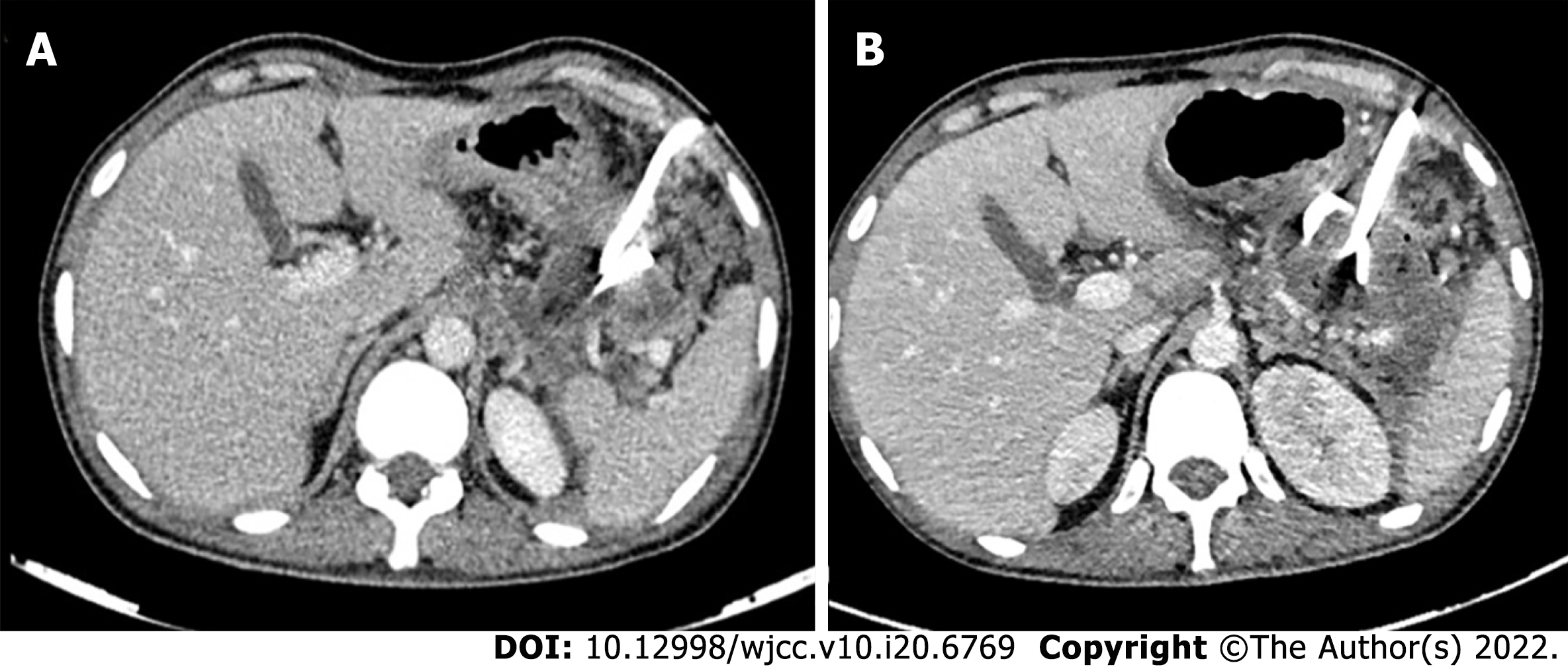
Figure 2 Step-up approach to management of pancreatic fluid collections.
A: Lesser sac collection with 14 F pigtail in-situ which was upgraded to 18 F; B: The patients later underwent endoscopic cystogastrostomy and necrosectomy (not shown).
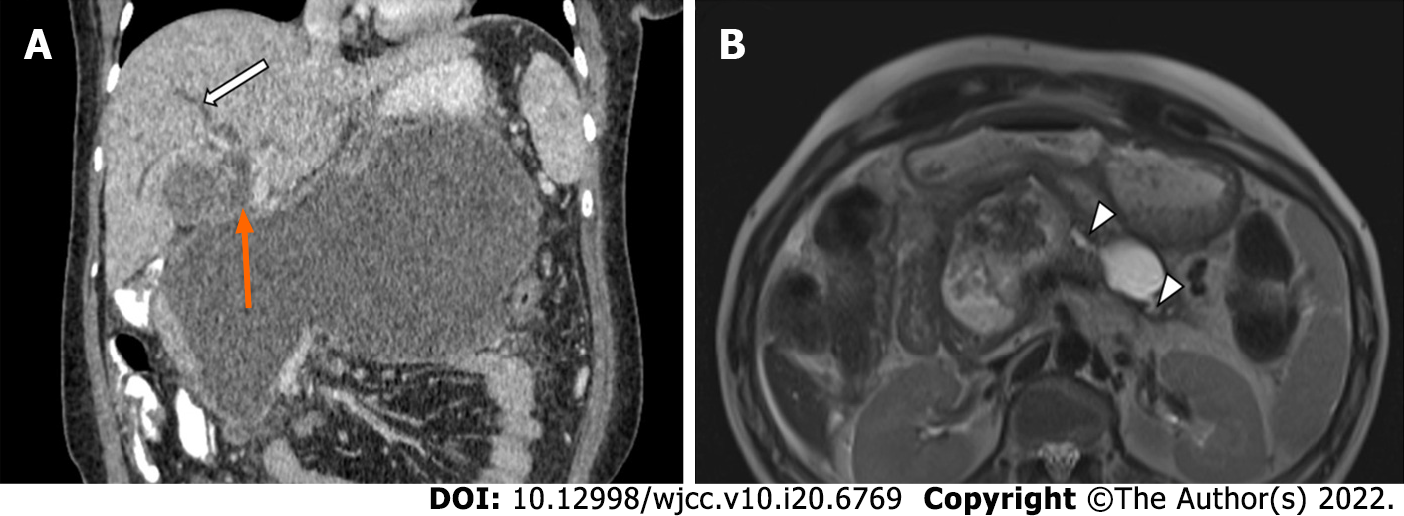
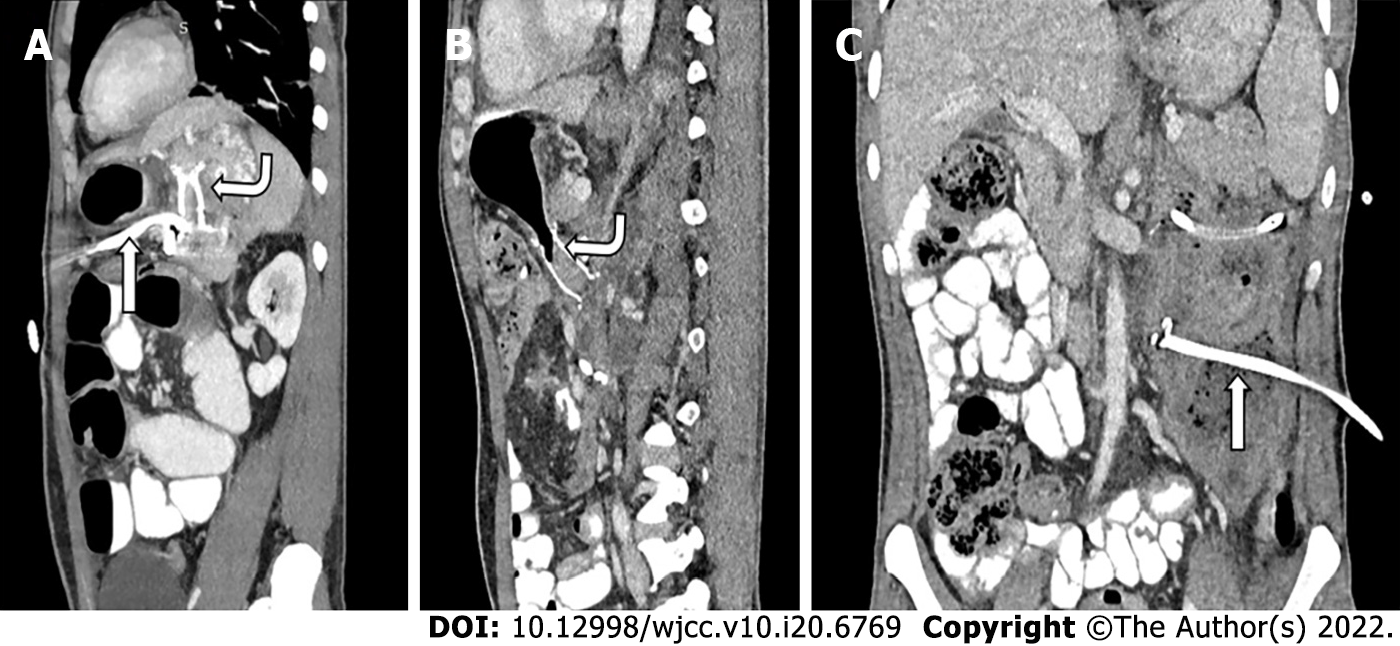
Figure 3 Evolving indications of drainage.
A: Large peripancreatic collection compressing the ampulla (orange arrow) causing biliary dilatation (white arrow); B: Disconnected pancreatic duct syndrome with dilated pancreatic duct communicating with the collections (arrowheads).
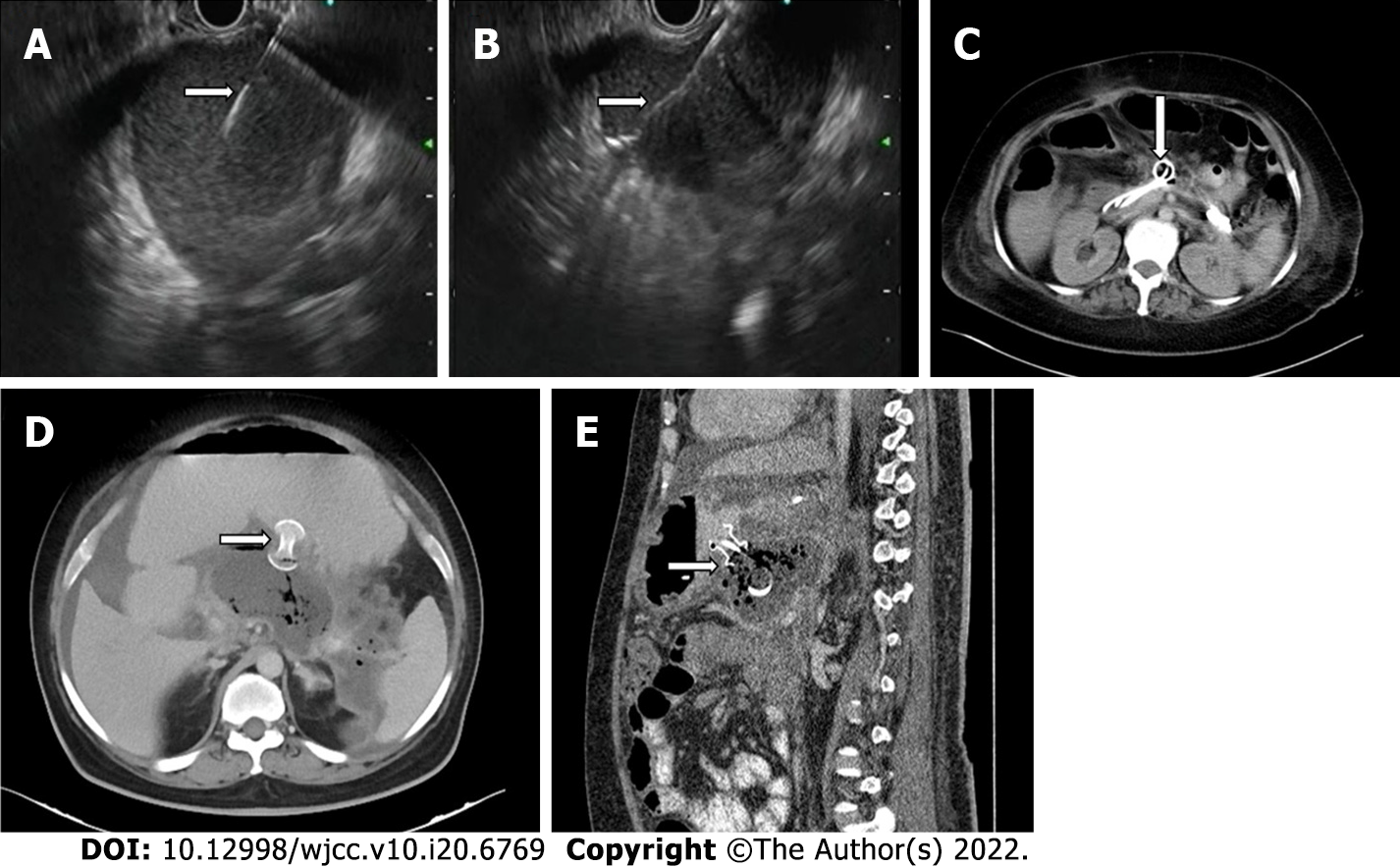
Figure 4 Endoscopic transmural drainage.
A: Endoscopic ultrasound guided transmural puncture of the lesser sac collection with needle tip in situ (arrow); B: Guidewire (arrow) passed through the needle into the collection; C: Double pigtail cystogastrostomy catheters (arrow) in the partially drained lesser sac collection; D: Axial; E: Sagittal computed tomography images showing lumen apposing metal stents (arrows).
Figure 5 Routes of percutaneous catheter drainage.
A: Retroperitoneal; B: Transperitoneal; C: Transgastric; D: Transhepatic.
Figure 6 Dual modality drainage in different patients.
A: Sagittal sections showing presence of both a lumen apposing metal stent (LAMS-curved arrow) and a transperitoneal percutaneous catheter (PCD-straight arrow) in the same collection; B: Sagittal section; C: Coronal sections of a patient showing LAMS (curved arrow) in the lesser sac component and PCD (straight arrow) in the paracolic component of the same collection utilizing advantages of both types of drainages.
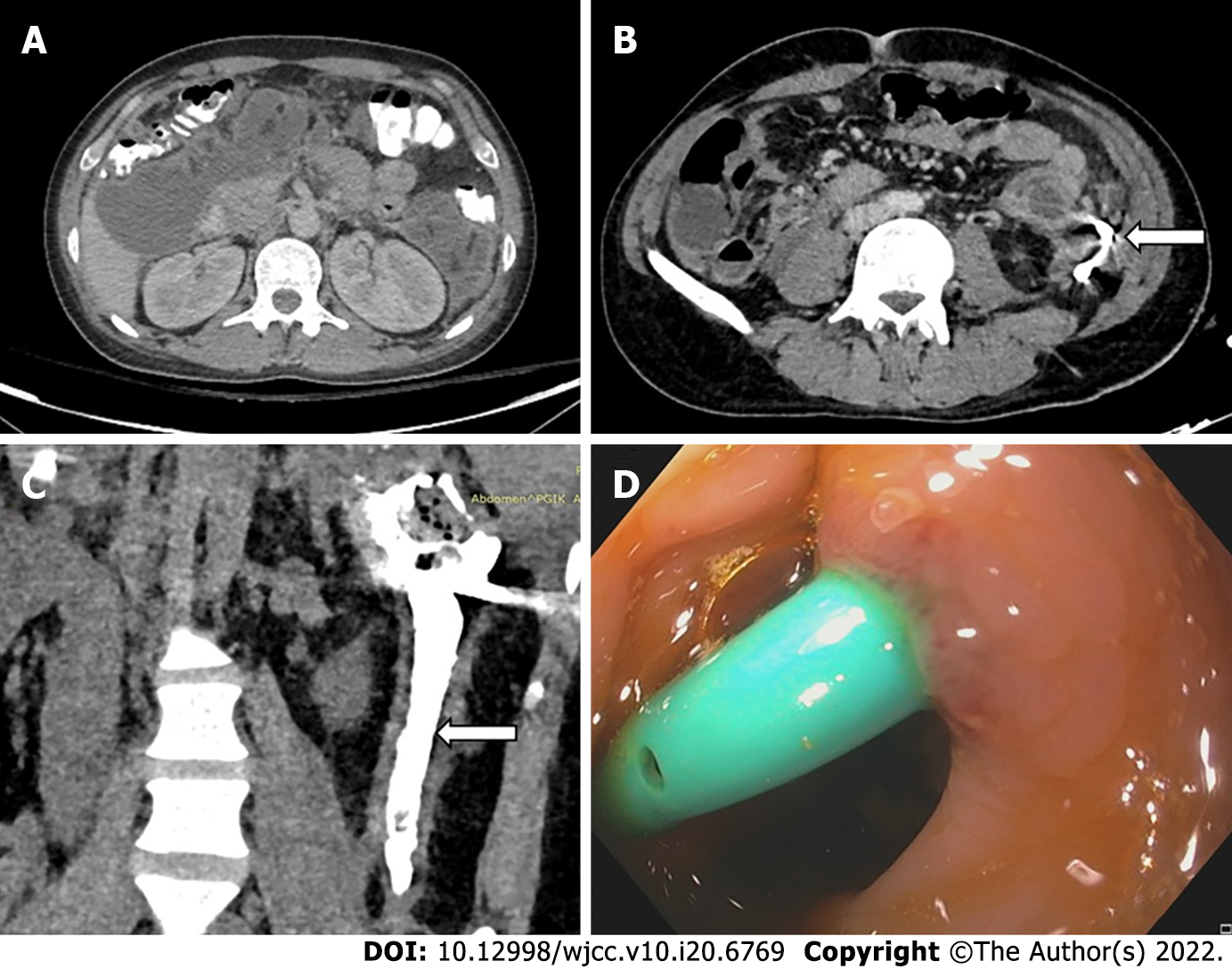
Figure 7 Gastrointestinal fistula formation after percutaneous catheter placement.
A: Pre percutaneous catheter (PCD) computed tomography (CT) showing walled off necrosis in left paracolic gutter (PCG) and subhepatic space; B: Axial CT showing pigtail in situ in the PCG collection (arrow); C: CT-PCD gram (coronal section) showing communication of the collection with descending colon with contrast in the lumen (arrow); D: Colonoscopic image showing pigtail tip in the colon lumen.
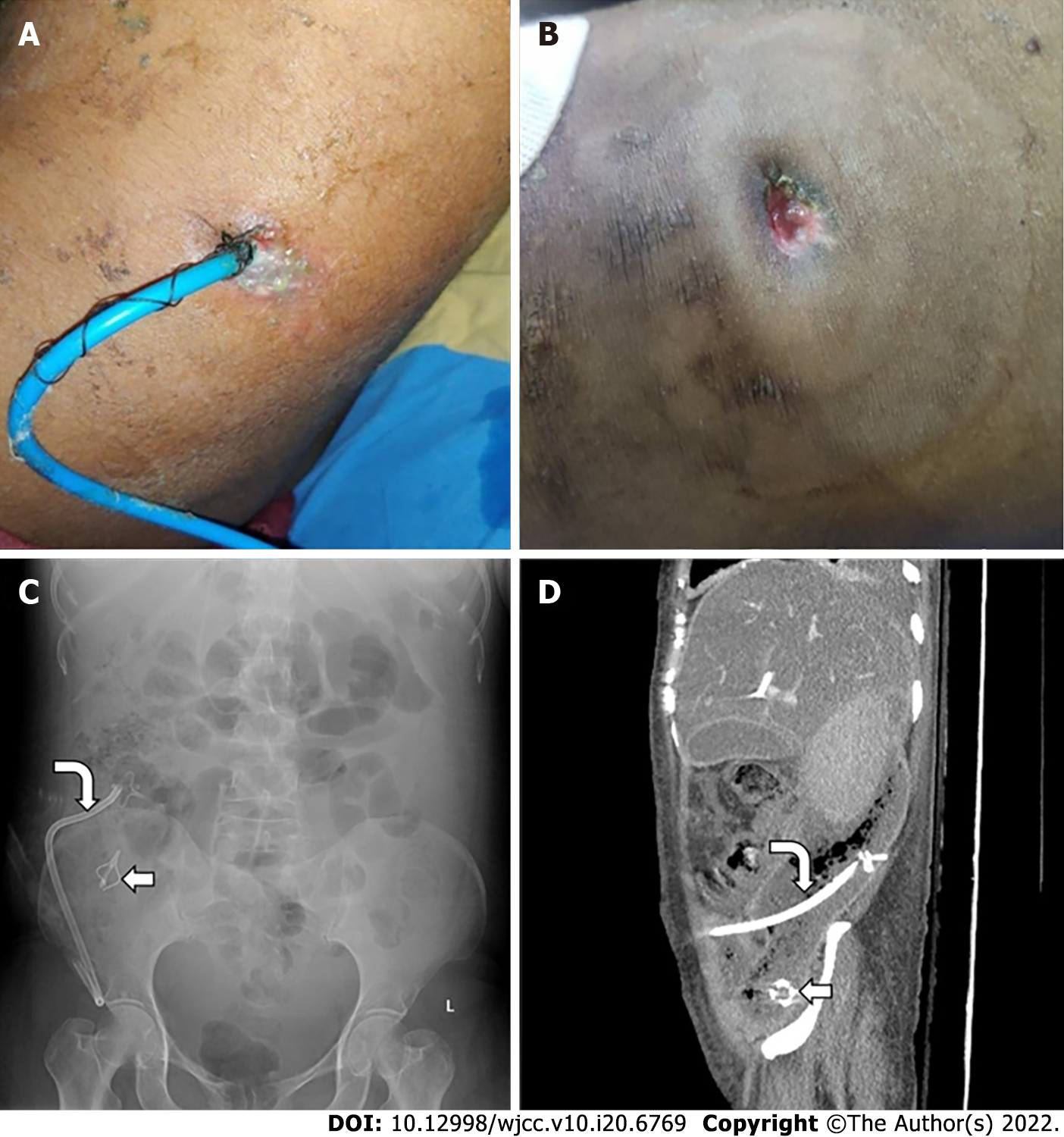
Figure 8 Rare and overlooked complications of percutaneous catheter placement.
A: Clinical photograph of a patient with percutaneous catheter drainage showing skin changes; B: Skin changes and erosions due to percutaneous catheter percutaneous catheter placement and pericatheter leak in another patient; C: Abdominal Radiograph shows broken catheter (straight arrow) in right iliac fossa. Also note the other part of the same catheter (curved arrow); D: Catheter tip fracture with shaft of catheter (curved arrow) and tip (straight arrow) seen separately on X-Ray and computed tomography.
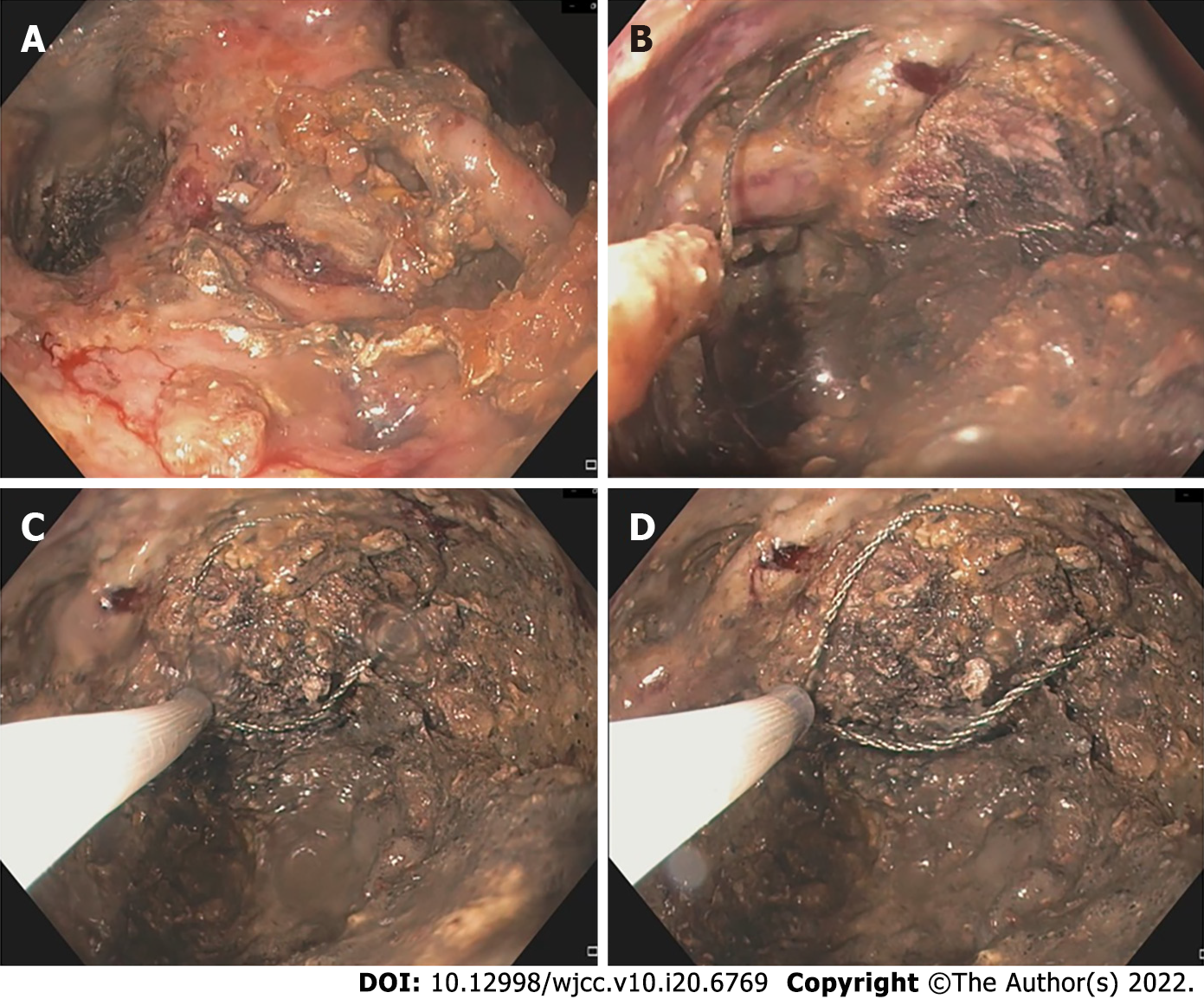
Figure 9 Direct endoscopic necrosectomy.
A: Endoscopic images showing large amount of necrotic debris within the collection; B: Snare placed into the necrotic collection using the endoscopic route; C: Partial removal of necrotic debris using snare; D: Dark necrotic residual collection seen with snare in situ.
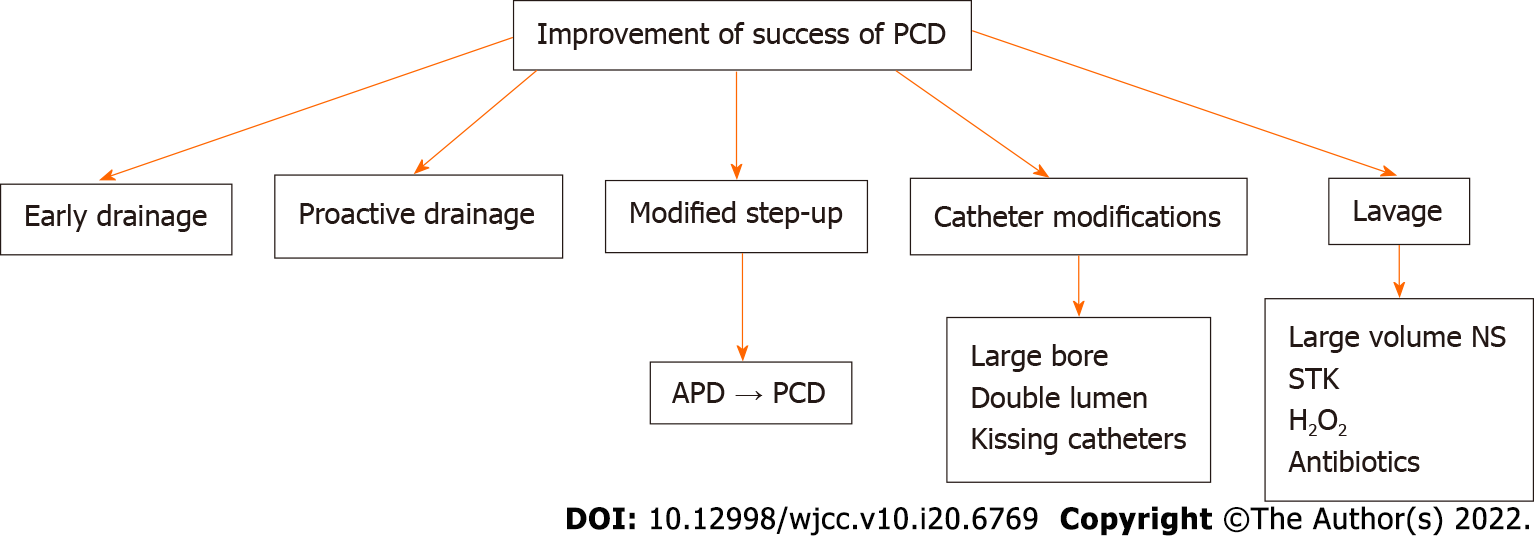
Figure 10 Factors influencing success of percutaneous catheter.
PCD: Percutaneous catheter drainage; APD: Abdominal paracentesis drainage; NS: Normal saline; STK: Streptokinase.
- Citation: Bansal A, Gupta P, Singh AK, Shah J, Samanta J, Mandavdhare HS, Sharma V, Sinha SK, Dutta U, Sandhu MS, Kochhar R. Drainage of pancreatic fluid collections in acute pancreatitis: A comprehensive overview. World J Clin Cases 2022; 10(20): 6769-6783
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/6769.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.6769