Copyright
©The Author(s) 2022.
World J Clin Cases. Jan 14, 2022; 10(2): 677-684
Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.677
Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.677
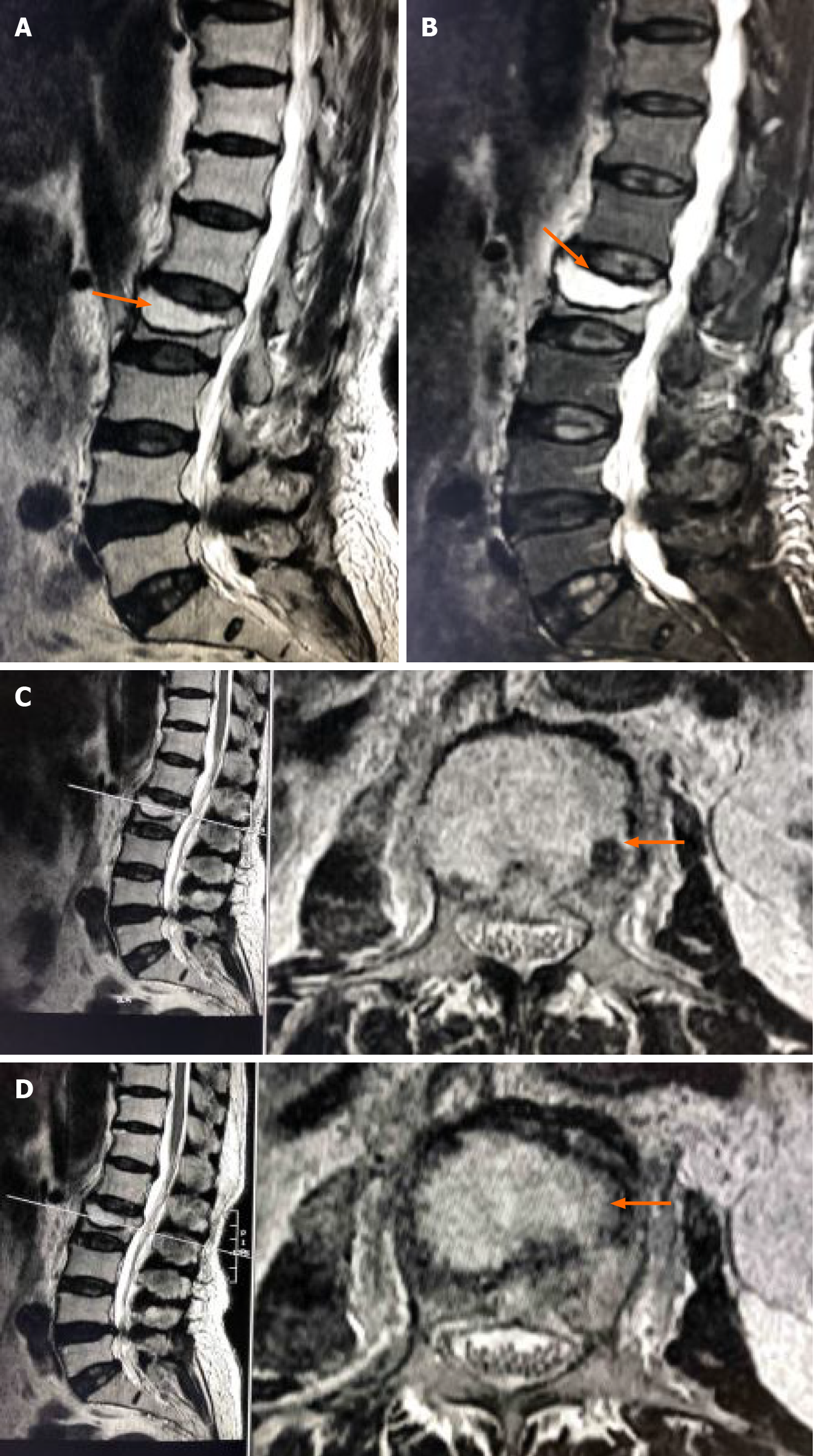
Figure 1 Magnetic resonance imaging.
A: Preoperative MRI indicated collapse of the L2 vertebral body and the formation of an intravertebral cavity-like structure indicated by the arrows; B: T2WI with fat suppression (T2WI FS) showed a fluid-filled intravertebral vacuum, with little of the upper endplate structure remaining indicated by the arrows; C and D: T2WI showed a low signal at the cavity edge, indicating vertebral bone necrosis and fibrous perichondrium formation, indicated by the arrows.
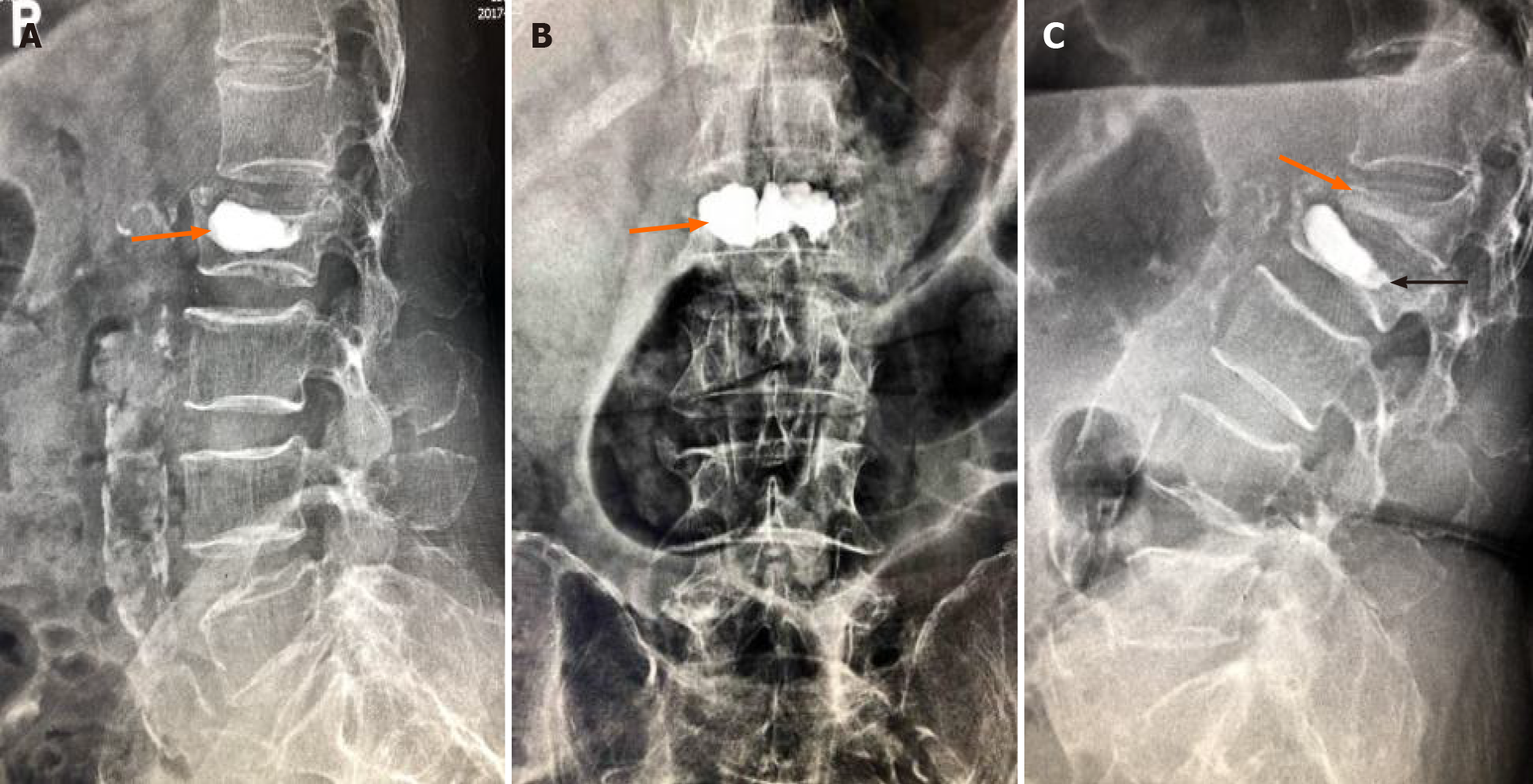
Figure 2 X-ray images.
A and B: Postoperative X-ray images showed that bone cement filled the cystic cavity of the L2 vertebral body with smooth edges, and there was insufficient bone cement dispersion outside the cystic cavity; C: Fifty days postoperatively, X-ray images showed L2 vertebral body collapse, slight forward bone cement displacement (indicated by the black arrow), L1 vertebral compression fracture, and severe collapse (indicated by the orange arrow).
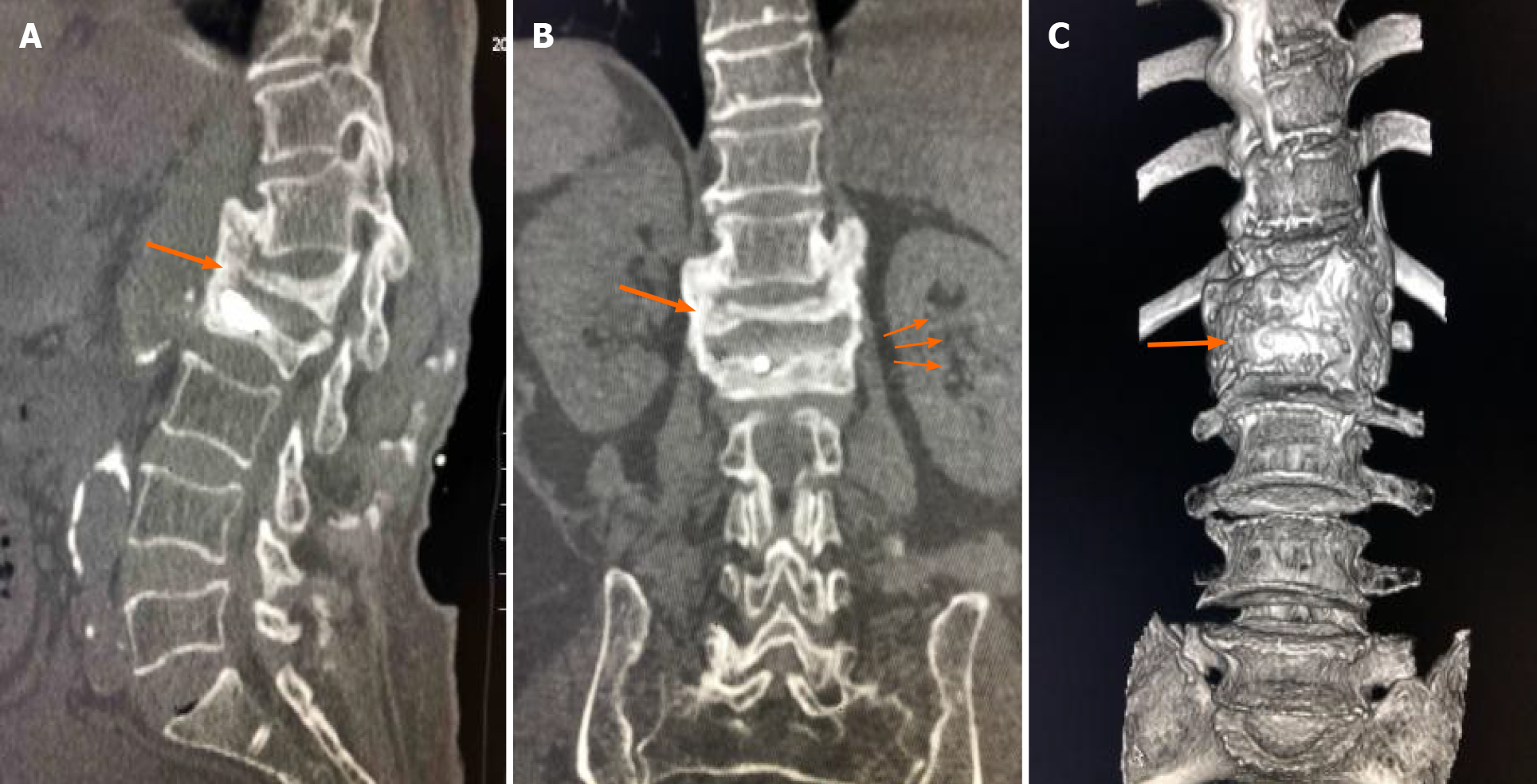
Figure 3 Computed tomography imaging.
Seven-month follow-up computed tomography (CT) indicated extensive callus formation around the T12-L2 vertebrae and intervertebral bridging ossification, providing new stability, as indicated by the arrow.
- Citation: Li J, Liu Y, Peng L, Liu J, Cao ZD, He M. Intervertebral bridging ossification after kyphoplasty in a Parkinson’s patient with Kummell’s disease: A case report. World J Clin Cases 2022; 10(2): 677-684
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/677.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.677