Copyright
©The Author(s) 2022.
World J Clin Cases. Jun 16, 2022; 10(17): 5723-5731
Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5723
Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5723
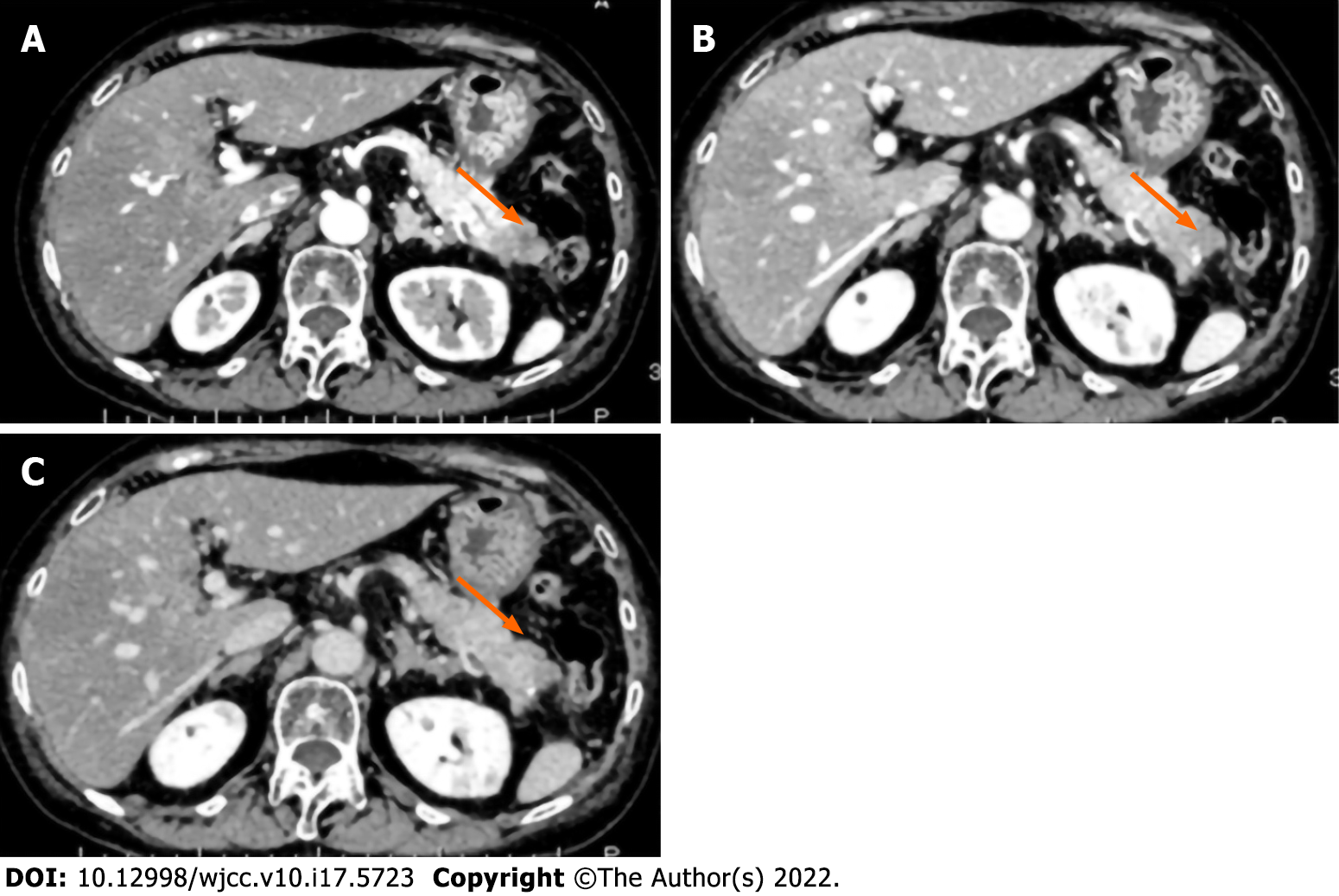
Figure 1 Contrast-enhanced abdominal computed tomography showing a 3-cm hypovascular lesion in the pancreatic tail.
A: Arterial phase; B: Venous phase; C: Equilibrium phase.
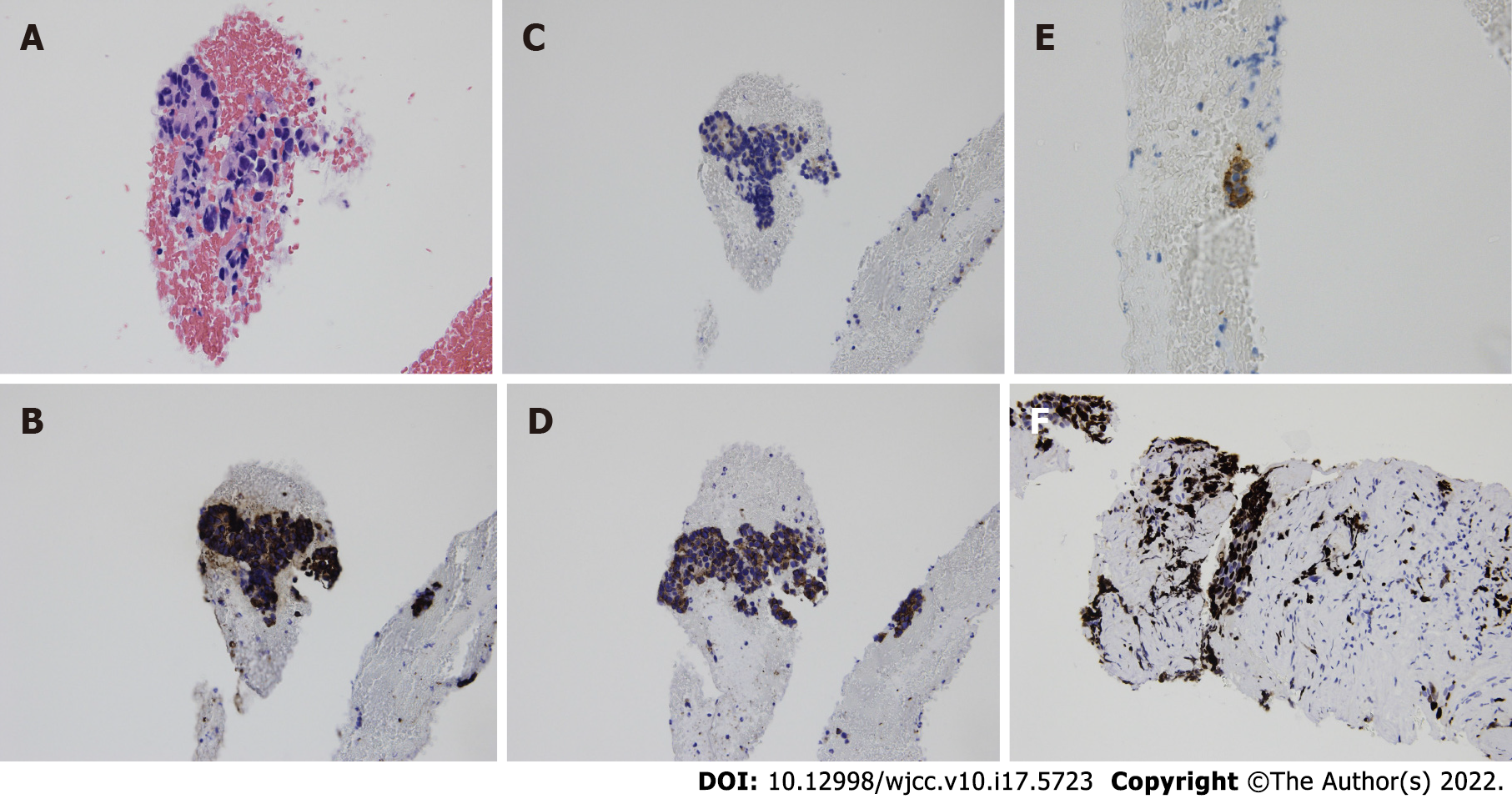
Figure 2 Cytological images of endoscopic ultrasound-guided fine-needle aspiration showing cell clusters with high nuclear/cytoplasmic ratio.
A: Cell clusters show non-specific structure after H-E staining; B: Immunostaining was positive for chromogranin A; C: Synaptophysin; D: CD 56; E: ACTH; and F: The Ki-67 index was approximately 40%.
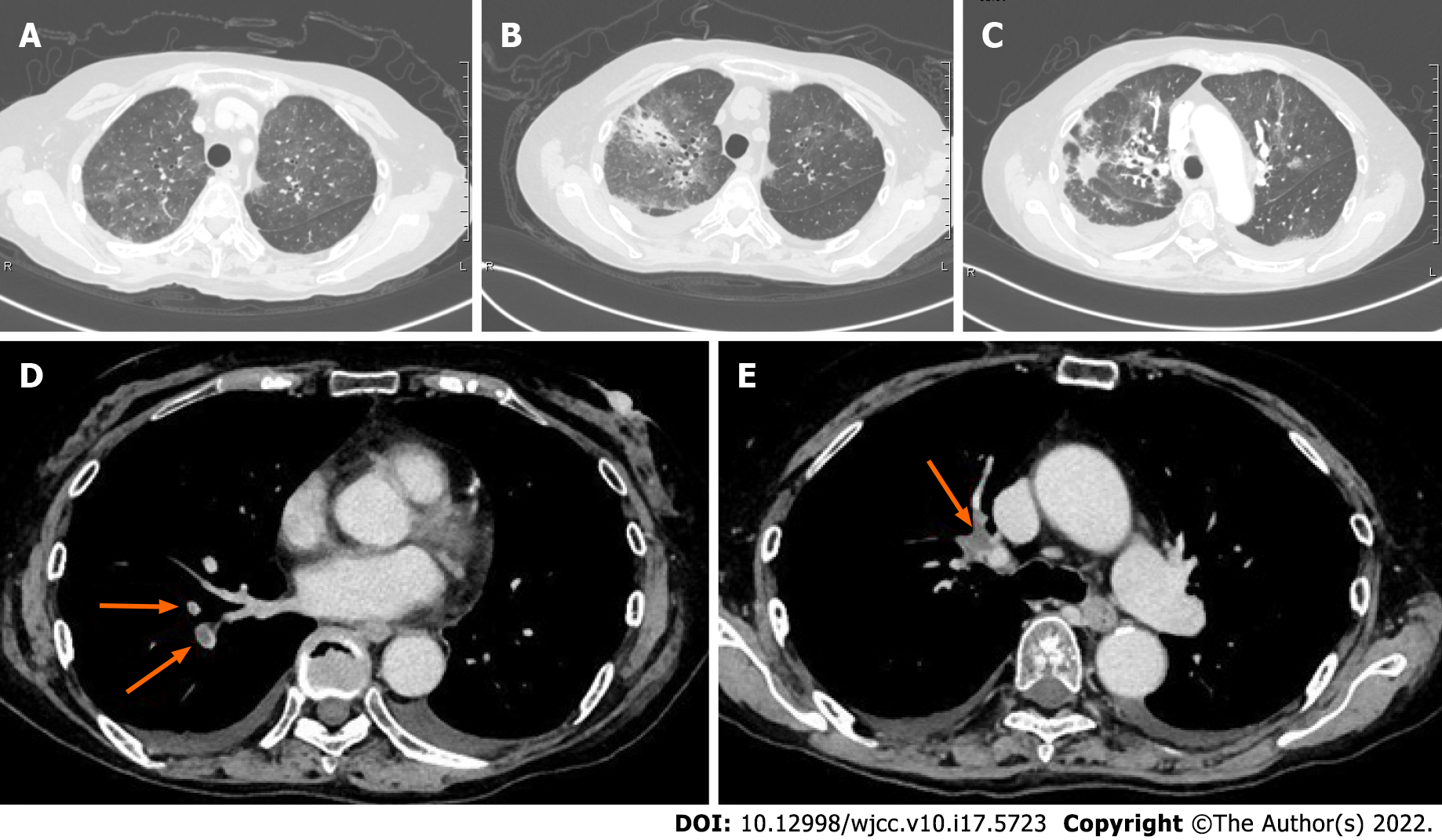
Figure 3 Representative microphotographs showing hypercortisolemia-related infectious and thrombotic complications.
A: Computed tomography revealed bilateral ground-glass opacities (GGO) on day 9; B: The area of GGO was spread, and new patchy consolidations were found in the right lobe on day 19; C: The area of GGO was decreased, and consolidation was observed in the sub-pleural regions suggesting the presence of organizing pneumonia on day 28; D and E: Computed tomography showing pulmonary thromboembolism.
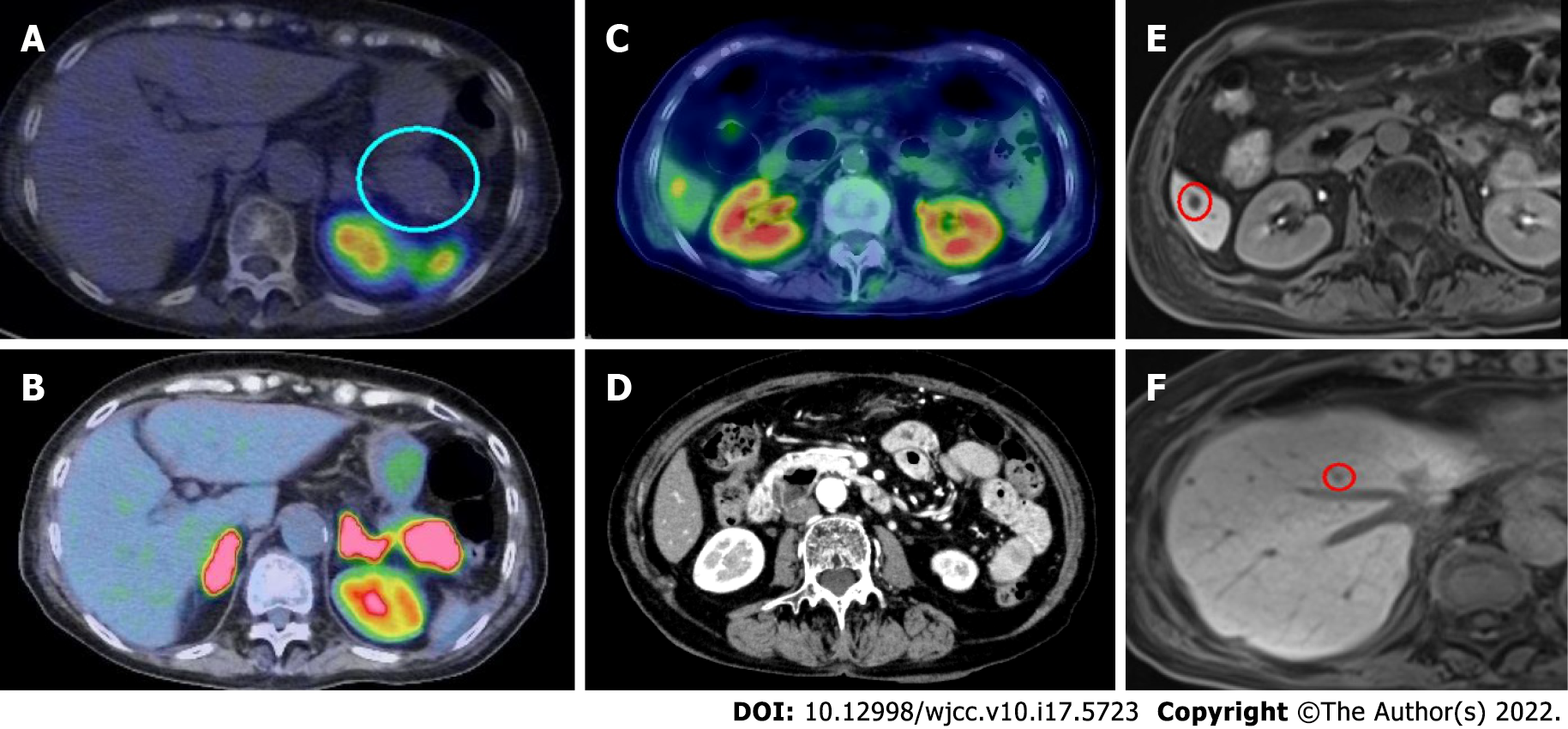
Figure 4 Radioisotope studies, computed tomography, and magnetic resonance imaging.
A: Somatostatin receptor scintigraphy using 111In-pentetoreotide showed no uptake in the pancreatic tumor; B and C: Positron emission tomography using 18F-fluorodeoxyglucose showed uptake in the pancreatic tumor and the liver; D: The computed tomography scan performed before transfer to Mie University showed no lesion; E and F: Gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid (Gd-EOB-DTPA)-magnetic resonance imaging also revealed multiple liver tumors suggesting metastases.
- Citation: Yoshihara A, Nishihama K, Inoue C, Okano Y, Eguchi K, Tanaka S, Maki K, Fridman D'Alessandro V, Takeshita A, Yasuma T, Uemura M, Suzuki T, Gabazza EC, Yano Y. Adrenocorticotropic hormone-secreting pancreatic neuroendocrine carcinoma with multiple organ infections and widespread thrombosis: A case report. World J Clin Cases 2022; 10(17): 5723-5731
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5723.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5723