Published online Mar 20, 2025. doi: 10.5662/wjm.v15.i1.96923
Revised: August 9, 2024
Accepted: August 21, 2024
Published online: March 20, 2025
Processing time: 133 Days and 22.9 Hours
The success rate of apexification is primarily determined by multiple factors, including the material used, the size of the open apex compared to the length of the root, and the technique used in each case. The main objective of this review was to provide an update on the present management of open apex to identify factors and circumstances that may influence the success of apexification using different materials and techniques. Future research on apexification should focus on how to treat open apices with wide periapical lesions without surgery. Pre
Core Tip: Trauma to the pulp before root formation induces pulpal necrosis, which impairs dentin and root growth. The thin, fragile dentin walls that lead to the exposed apex of the canal remain broad. Therefore, root canal treatment in these cases is becoming increasingly complex. In these situations, mineral trioxide aggregate (MTA) apexification has replaced calcium hydroxide apexification because of its superior properties. It is a reliable method for creating a rigid apical tissue barrier. To solve this endodontic enigma, this review discussed the nonsurgical treatment of an open apex with MTA, the micro apical placement system, magnification, and bioceramics.
- Citation: Chauhan S, Chauhan R, Bhasin P, Sharaf BG. Present status and future directions: Apexification. World J Methodol 2025; 15(1): 96923
- URL: https://www.wjgnet.com/2222-0682/full/v15/i1/96923.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i1.96923
A tooth typically completes its root development and apex closure within 3 years after erupting. However, during this time, the tooth is vulnerable to various accidents and injuries. Exposure of immature teeth to such accidents can halt root formation, and the wide canal and open apices may complicate root canal treatment[1]. Injuries to the front teeth, particularly the upper central or lateral incisors, are quite common, affecting almost 16%-17% of the population. In severe cases, this can lead to tooth pulp inflammation and ultimately pulp necrosis[2].
Regenerative endodontics is becoming more popular than apexification due to continuous root development in nonvital teeth. However, success is not guaranteed. Apexification is a common therapeutic approach for pulpless permanent teeth with an open apex, also known as the “blunderbuss” canal. Its goal is to induce apical healing as a rigid tissue barrier across the apex[3].
Due to the complex anatomy, treating immature necrotic teeth remains challenging for clinicians[4]. Treating teeth with incomplete root development has always presented significant challenges in endodontics for the following reasons: (1) The mechanical instrumentation of the root canal presents difficulties because of the unique anatomical characteristics of the developing tooth; (2) Because there is no apical stop, sealing the root canal with conventional filling techniques is challenging; and (3) The thin root canal walls of teeth that remain in development are brittle[5].
The etiology of the open apex are as follows: Pulp necrosis can occur due to caries or trauma; orthodontic teeth have caused extensive apical resorption; periapical pathosis or trauma; over instrumentation (iatrogenic); thermal injuries; chemical injuries; and others, such as dens in dente and dentin dysplasia, exhibit similar symptoms.
A tooth with an open apex presents challenges such as thin dentinal walls prone to fracture, periapical lesions with or without apical resorption, and a compromised crown-root ratio due to short roots affecting the long-term prognosis. Large open apices pose challenges in terms of working length, root canal preparation, and obturation[6].
Clinical tests include electric and thermal tests, such as heat and cold tests, which may elicit varied responses in permanent teeth with immature apexes[7]. Doppler flowmetry can measure the blood flow in traumatized teeth. A pulse oximeter is a reliable tool for monitoring pulp vitality by measuring the oxygenation of pulp flow[8,9]. A thorough dental history should be taken to understand all symptoms and characteristics of associated pain. A detailed pain history, including duration, nature, and factors that worsen or alleviate the pain should be taken. Additionally, a clinical examination should be conducted to determine the presence or absence of swelling, crown discoloration, caries, mobility, and periodontal probing to check the status of the pulp[10].
It can be difficult to interpret radiographic images, especially when differentiating between healthy pulp and pathologic radiolucency caused by necrotic pulp. Comparing it with the apex of the opposing tooth can help[11]. Cone-beam computed tomography or digital volume tomography overcomes the drawbacks of two-dimensional radiography for the precise measurement of the dentinal walls and size of periapical lesions. With early diagnosis and intervention, pulp preservation strategies create an optimal environment for ongoing dentine apposition and root formation[12].
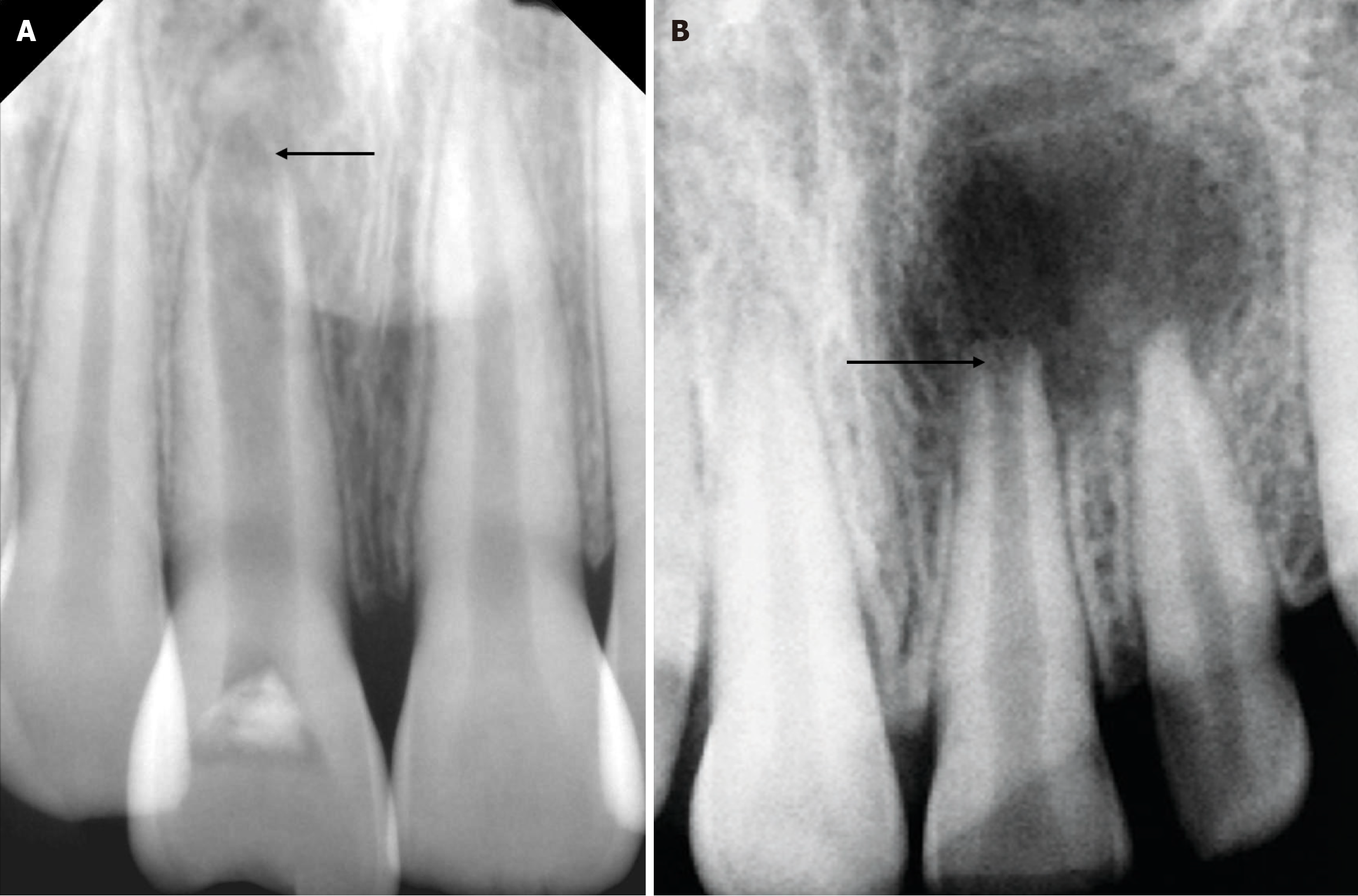
There are two types of open apex: Blunderbuss apices (Figure 1A) and non-blunderbuss apices (Figure 1B). The blunderbuss apex features divergent walls and a funnel-shaped apex. In contrast, the non-blunderbuss apex may have parallel or slightly convergent walls, resulting in a broad-shaped or convergent apex.
When treating an immature permanent tooth with a blunderbuss canal, challenges include mechanical preparation, canal disinfection, a lack of a tapered root canal seal, and thin, brittle radicular walls[13]. One of the key factors in the treatment selection criteria is the width of the apex diameter. According to the literature[2], apexification is the preferred treatment if the apex diameter is more than 1.1 mm.
The most popular procedure for an immature tooth with an open apex[14] is apexification, which stimulates the formation of a hard tissue barrier that allows ideal root canal obturation. The more prolonged treatment process associated with calcium hydroxide apexification has always been the main cause of concern[15]. Other contributing factors include the diameter of the open apex, questionable apical closure, continuing instrumentation, temporary restorations that can cause reinfection, and the possibility of tooth fracture[14]. To overcome the shortcomings of conventional calcium hydroxide apexification[16], which include the requirement for multiple appointments, the possibility of non-compliance, missed appointments, and coronal seal failure from temporary restorations, the artificial formation of the apical plug technique is a more effective and recommended approach to treatment[17]. This procedure makes it possible to fill the root canal system immediately.
Presently, a wide range of bioactive materials have been considered for this purpose, including mineral trioxide aggregate (MTA) putty, EndoCem, Biodentine, EndoSequence, OrthoMTA, MTA Plus, and mineral tricalcium phosphate (MTA)[18]. They bind with the dentine to form an appetite-like three-dimensional barrier when used as an apexification material. This fills the space created during contraction and strengthens the ability of the root canal to fracture[17]. Phosphorus and calcium ions stimulate osteoblastic or cementoblastic activity, which is promoted by bioactive materials[19]. These bioactive cements function by releasing calcium ions, which stimulate cell adhesion and proliferation. The high pH of the cement also creates an antimicrobial environment[20].
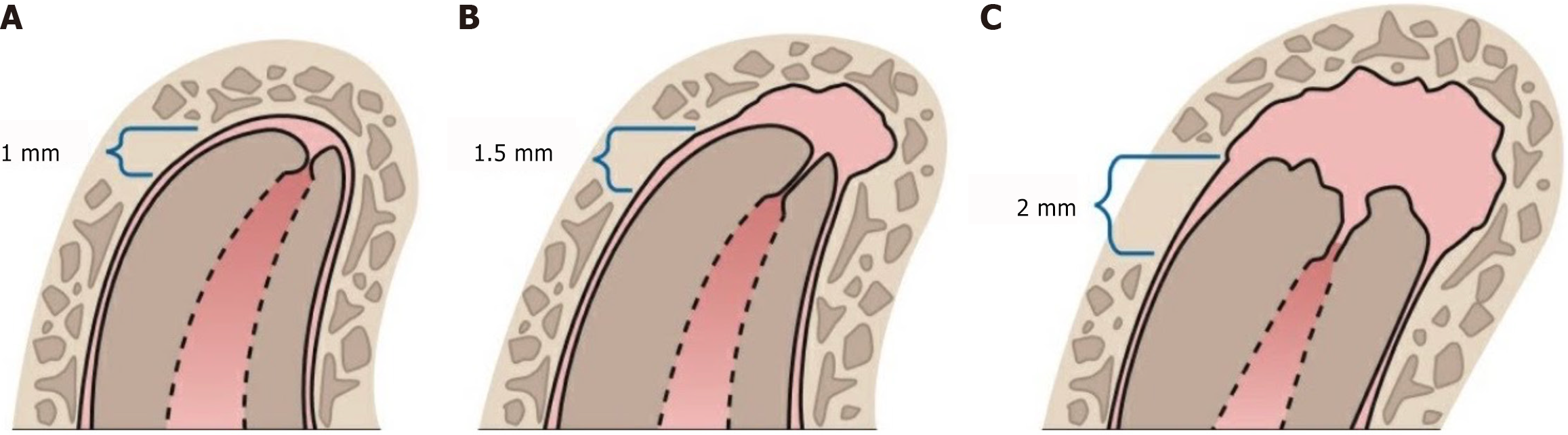
Wein’s recommendations for determining working length based on radiographic evidence of root or bone resorption are as follows (Figure 2): If no root or bone resorption is evident, the preparation should terminate 1.0 mm from the apical foramen; if bone resorption is apparent but there is no root resorption, shorten the length by 1.5 mm; and if both root and bone resorption are apparent, shorten the length by 2.0 mm[21].
The apexification technique depends on the root canal system being thoroughly disinfected because this greatly impacts the treatment outcome. Numerous negative effects of infection inhibit stem cell function and healing. Since these irrigants and medications should not negatively impact the patient’s stem cell survival and proliferate, chemical disinfection of the root canal system is not exclusively dependent on their bactericidal and bacteriostatic properties[22].
Guidelines prescribe irrigation with 5.25% sodium hypochlorite for 1 min. In contrast, a study by Mohmmed et al[23] revealed that the Enterococcus faecalis biofilm could not be effectively removed by irrigation with 5.25% sodium hypochlorite for 1 min. The investigation conducted by Martin et al[24] revealed that the dentinal walls were less affected by 1.5% sodium hypochlorite irrigation than by 6% sodium hypochlorite irrigation.
Three-dimensional canal cleaning has been demonstrated to be possible through the application of a 17% EDTA solution and internal heating of 5.25% sodium hypochlorite with ultrasonic activation. It is observed that the concentration at which sodium hypochlorite is used affects its ability to dissolve tissue. The suggested protocol for cases with mature apex formation is to employ a final irrigation solution of 5.25% sodium hypochlorite and 17% EDTA. On the other hand, teeth with an immature apex have a far higher possibility of these chemical agents extruding. The clinician needs to handle these kinds of instances with extreme caution while implementing treatments for these kinds of cases[22].
According to different studies, the application of an endoVac system, a negative pressure device intended to facilitate the evacuation of the irrigant from the canal, is one technique for reducing apical extrusion. Using an endoVac system or needles with microcannulas instead of traditional needles proved advantageous for removing apically extruded irrigants, as demonstrated by Gade et al[25].
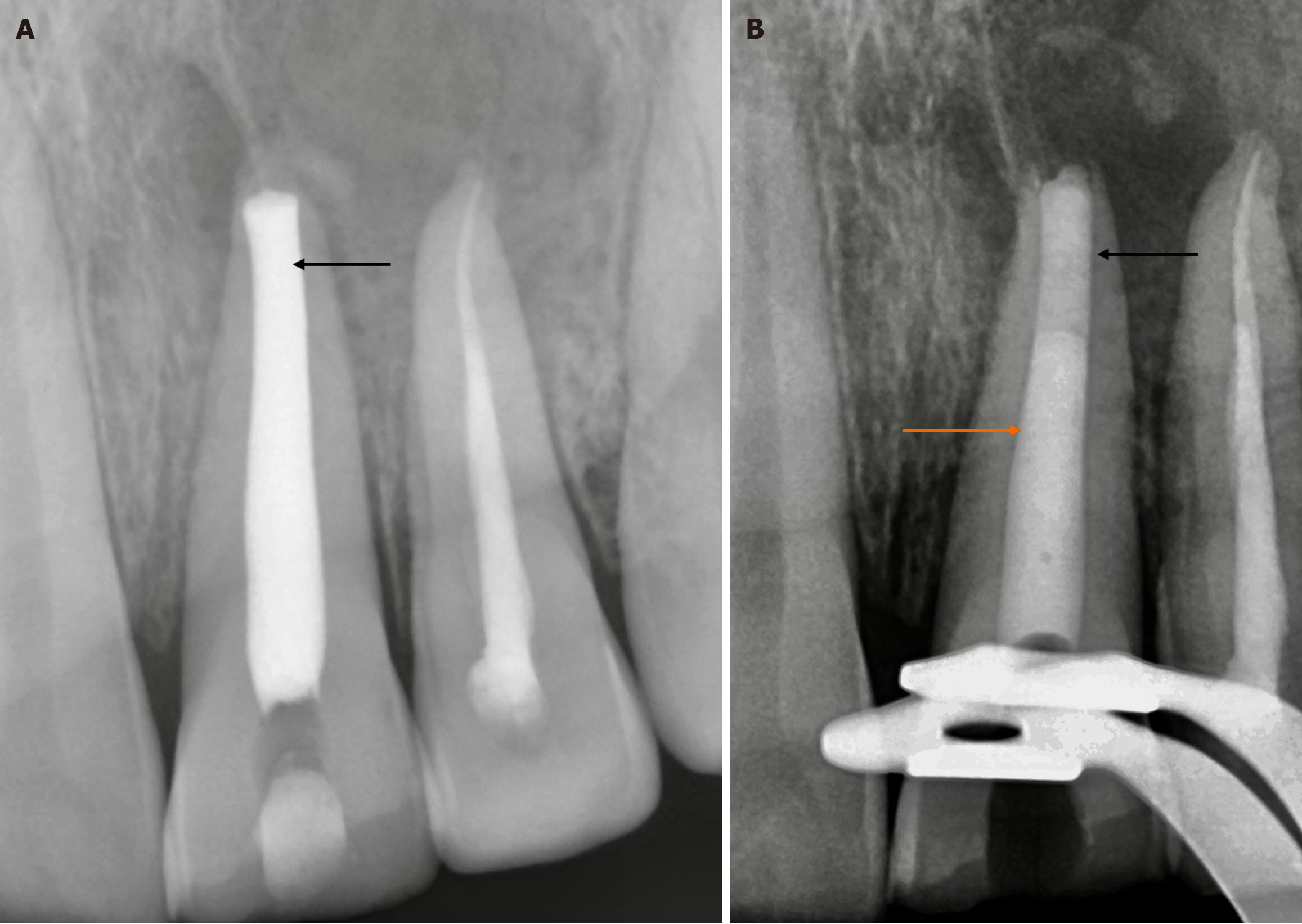
Another factor to be considered when assessing the disinfection of the root canal system is the use of intracanal medications. Any intracanal medication should ideally be able to release its antibacterial effect for a considerable amount of time after being inserted into the canal. Calcium hydroxide was the most frequently recommended intracanal medicine by Herman in 1920. It is essential to use a carrier when applying calcium hydroxide in the intracanal space (Figure 3A). In addition to making the material more radiopaque in radiography, a viscous vehicle will remain in the canal longer compared to a water-based vehicle[26].
Triple antibiotic paste (TAP), developed by Banchs and Trope and comprising metronidazole, ciprofloxacin, and minocycline, is another widely used intracanal medication. Its foundation was the idea of lesion sterilization and tissue repair therapy, which uses a mix of several antibacterial medications to disinfect oral infectious lesions, such as dentinal, pulpal, and periradicular lesions[27]. Since most of the bacteria in the infected root canal dentin are obligate anaerobes, metronidazole was initially prescribed as an antibacterial medication of choice. TAP has demonstrated significant success in reducing the number of bacteria in the infected root canal system and is effective in eliminating Enterococcus faecalis colonies even at low concentrations (e.g., 1 mg/mL, 0.1 mg/mL, and 0.01 mg/mL) with minimal impact on stem cell viability[28].
It has also been demonstrated to have far superior antibacterial properties than calcium hydroxide. The discoloration of teeth is one of the main side effects of using TAP over a long period due to the presence of minocycline, as evidenced by multiple case studies[26-29]. The goal is to minimize the effects of applying a paste that contains ciprofloxacin and metronidazole[27]. Emdogain is one of the newly approved intracanal medications used in endodontics; studies have demonstrated that it has a much stronger antibacterial impact and less detrimental effects on stem cell activity[29].
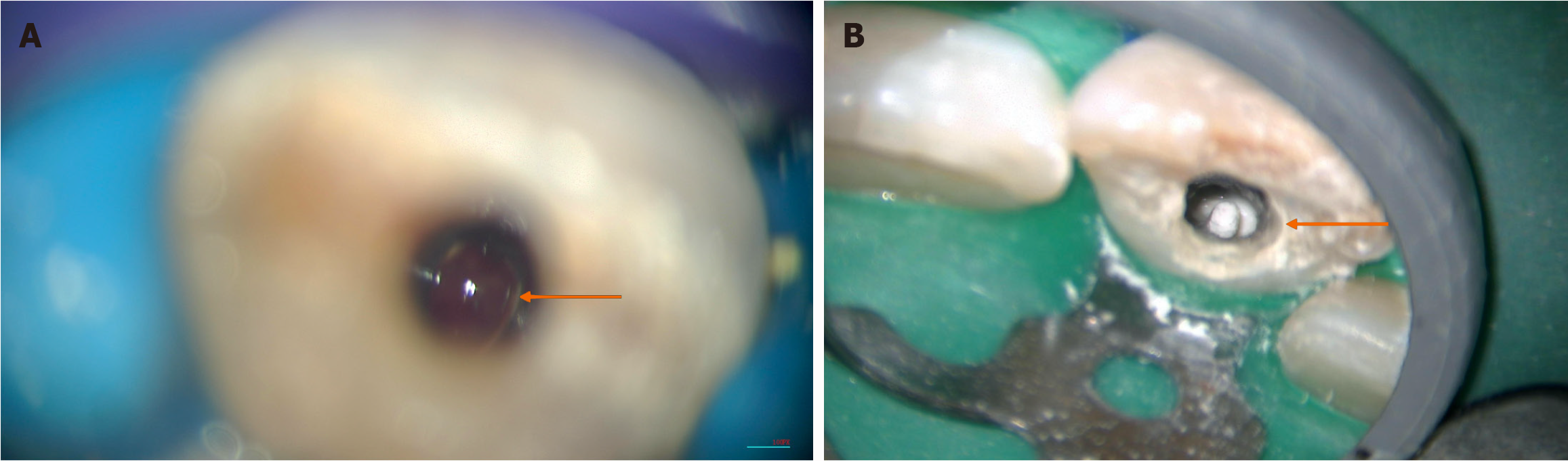
A dental operating microscope has a significant impact on the precise placement of the material and its marginal adaptation. Furthermore, it minimizes the obscurity of the operative field by providing high magnification and bri
Armamentarium for apexification are as follows: Rubber dam for isolation; paper points and condensers; collagen sponge; dental operating microscope; bioactive materials such as MTA, OrthoMTA, MTA Plus, Biodentine, Endo
When the canal walls are parallel or slightly convergent, with an apex size of less than 0.8 mm and the tuck back is present with the master cone then the obturation of the canal with a bioceramic sealer and gutta-percha is recommended. If canal walls are parallel or slightly convergent (non-blunderbuss apex), with an apex size of more than 0.8 mm then obturation of the canal should be done with a minimum of 5 mm of bioceramic cement. This applies regardless of whether the tuckback is present or absent from the master cone. When the walls diverge, the funnel-shaped flaring, also known as the blunderbuss apex, obturation of the canal with a minimum of 5 mm of bioceramic cement is recommended. After creating a 5 mm bioceramic plug, any sealer can be used for obturation, but using bioceramic sealer alone or in combination with gutta-percha can significantly improve the outcome of the tooth (Figure 3B).
The case undergoes pre-evaluation based on the clinical history and radiographic findings. The process involves access opening and determining the working length under rubber dam isolation. The root canal system undergoes cleaning and shaping, followed by irrigation with 1.5% sodium hypochlorite (20 mL) and saline irrigation (40 mL) using 27/30 G double-sided vented needles 3 mm above the working length. Final irrigation is performed using 2% chlorhexidine-gluconate (5 mL) or 1% alexidine-digluconate (5 mL). The irrigants undergo internal heating and activation through the use of sonic or ultrasonic devices and are administered 3-4 mm above the working length. The administration of an intracanal medication, such as calcium hydroxide, double antibiotic paste, or modified TAP/Emdogain, is necessary.
The evaluation process includes a radiographic examination of the tooth, followed by an assessment of the patient’s pain level. The canal is irrigated with saline to eliminate the medication. The process involves copious irrigation and activation using 1.5% sodium hypochlorite, followed by final irrigation of 17% EDTA (20 mL, 5 min), after which the canals are dried using paper points. During the irrigation procedure, the patient should be asymptomatic completely, with no debris coming from the canal. A 5 mm bioactive cement plug is made, followed by obturation and composite. If there are any craze lines or fractures in the tooth, the recommended protocol is apexification, followed by a crown. Follow-up should occur after 1 month, 3 months, 6 months, 1 year, 2 years, and 5 years. The tooth of interest is evaluated with cone-beam computed tomography after 1 year to determine the thickness of the dentin.
For nonsurgical treatment of chronic lesions with an open apex, adequate infection control with three-dimensional cleaning and irrigant usage combined with intracanal medications facilitates regression of the microorganisms and induces healing. By reducing the challenges associated with conventional approaches and creating a better apical seal, an apical plug using bioactive cement results in enhanced condensed apical plugs under magnification. For the management of open apexes, implementing a dental operating microscope in conjunction with bioceramics is now extremely effective. For the treatment of a nonvital immature tooth with a wide-open apex, apexification is the precise approach since it is more predictable, takes less time, and produces effects promptly. The management of this endodontic mystery has been improved by recent bioactive cement, bioceramic sealers, and magnification for the treatment of teeth with an immature apex[6].
| 1. | Gill I, Mittal S, Kumar T, Keshav V. Open Apex and its Management: Review Article. J Pharm Bioallied Sci. 2024;16:S31-S34. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (2)] |
| 2. | Nj N, S P, Ms R, Kumar TS. Endodontic management of an open apex with apexification using Mineral trioxide aggregate: A case report. Med Sci. 2022;26. [RCA] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 3. | Singh N, Mittal N, Baranwal H, Tripathi R, Wang C. Single-visit apexification in immature necrotic teeth using mineral trioxide aggregate as an apical plug: Case series. SRM J Res Dent Sci. 2019;10:239. [DOI] [Full Text] |
| 4. | Rafter M. Apexification: a review. Dent Traumatol. 2005;21:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 287] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 5. | Graziele Magro M, Carlos Kuga M, Adad Ricci W, Cristina Keine K, Rodrigues Tonetto M, Linares Lima S, Henrique Borges A, Garcia Belizário L, Coêlho Bandeca M. Endodontic Management of Open Apex Teeth Using Lyophilized Collagen Sponge and MTA Cement: Report of Two Cases. Iran Endod J. 2017;12:248-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 6. | Bhasin P, Saraf BG, Chauhan S, Kumar H, Wahi P, Vats V. The Successful Interdisciplinary Outcome of Blunderbuss Canal with an Open Apex Using MTA under Magnification: A Case Report. Int J Clin Pediatr Dent. 2024;17:97-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (2)] |
| 7. | Brandt K, Kortegaard U, Poulsen S. Longitudinal study of electrometric sensitivity of young permanent incisors. Scand J Dent Res. 1988;96:334-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Jafarzadeh H. Laser Doppler flowmetry in endodontics: a review. Int Endod J. 2009;42:476-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Setzer FC, Kataoka SH, Natrielli F, Gondim-Junior E, Caldeira CL. Clinical diagnosis of pulp inflammation based on pulp oxygenation rates measured by pulse oximetry. J Endod. 2012;38:880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Pileggi R, Dumsha TC, Myslinksi NR. The reliability of electric pulp test after concussion injury. Endod Dent Traumatol. 1996;12:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Santos MS, Dos Santos AB, Carvalho MS. New Insights in Hydrogels for Periodontal Regeneration. J Funct Biomater. 2023;14. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Camp JH. Diagnosis dilemmas in vital pulp therapy: treatment for the toothache is changing, especially in young, immature teeth. Pediatr Dent. 2008;30:197-205. [PubMed] |
| 13. | Sharma V, Sharma S, Dudeja P, Grover S. Endodontic management of nonvital permanent teeth having immature roots with one step apexification, using mineral trioxide aggregate apical plug and autogenous platelet-rich fibrin membrane as an internal matrix: Case series. Contemp Clin Dent. 2016;7:67-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Nagmode PS, Satpute AB, Patel AV, Ladhe PL. The Effect of Mineral Trioxide Aggregate on the Periapical Tissues after Unintentional Extrusion beyond the Apical Foramen. Case Rep Dent. 2016;2016:3590680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Metzger Z, Solomonov M, Mass E. Calcium hydroxide retention in wide root canals with flaring apices. Dent Traumatol. 2001;17:86-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Pawar AM, Pawar SM, Pawar MG, Kokate SR. Retreatment of endodontically failed tooth with wide-open apex using platelet rich fibrin membrane as matrix and an apical plug of Biodentine™. Eur J Gen Dent. 2015;4:150-154. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 713] [Cited by in RCA: 659] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 18. | Vinaya Susan V, Veerendra U Nirmal K. One-step Apexification Of Blunderbass Canal Using Biodentin. Chrismed J Health Res. 2017;4:280-282. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Güneş B, Aydinbelge HA. Mineral trioxide aggregate apical plug method for the treatment of nonvital immature permanent maxillary incisors: Three case reports. J Conserv Dent. 2012;15:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Prati C, Gandolfi MG. Calcium silicate bioactive cements: Biological perspectives and clinical applications. Dent Mater. 2015;31:351-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 304] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 21. | Floratos SG, Tsatsoulis IN, Kontakiotis EG. Apical barrier formation after incomplete orthograde MTA apical plug placement in teeth with open apex--report of two cases. Braz Dent J. 2013;24:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Plascencia H, Díaz M, Gascón G, Garduño S, Guerrero-Bobadilla C, Márquez-De Alba S, González-Barba G. Management of permanent teeth with necrotic pulps and open apices according to the stage of root development. J Clin Exp Dent. 2017;9:e1329-e1339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Mohmmed SA, Vianna ME, Penny MR, Hilton ST, Knowles JC. The effect of sodium hypochlorite concentration and irrigation needle extension on biofilm removal from a simulated root canal model. Aust Endod J. 2017;43:102-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Martin DE, De Almeida JF, Henry MA, Khaing ZZ, Schmidt CE, Teixeira FB, Diogenes A. Concentration-dependent effect of sodium hypochlorite on stem cells of apical papilla survival and differentiation. J Endod. 2014;40:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 206] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 25. | Gade VJ, Sedani SK, Lokade JS, Belsare LD, Gade JR. Comparative evaluation of debris removal from root canal wall by using EndoVac and conventional needle irrigation: An in vitro study. Contemp Clin Dent. 2013;4:432-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011;44:697-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 381] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 27. | Vijayaraghavan R, Mathian VM, Sundaram AM, Karunakaran R, Vinodh S. Triple antibiotic paste in root canal therapy. J Pharm Bioallied Sci. 2012;4:S230-S233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Siqueira JF Jr, Lopes HP. Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J. 1999;32:361-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 473] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 29. | Wang HH, Sarmast ND, Shadmehr E, Angelov N, Shabahang S, Torabinejad M. Application of Enamel Matrix Derivative (Emdogain) in Endodontic Therapy: A Comprehensive Literature Review. J Endod. 2018;44:1066-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Kakani AK, Veeramachaneni C. Sealing ability of three different root repair materials for furcation perforation repair: An in vitro study. J Conserv Dent. 2020;23:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |