Published online Dec 17, 2018. doi: 10.5527/wjn.v7.i8.155
Peer-review started: August 3, 2018
First decision: August 21, 2018
Revised: October 29, 2018
Accepted: November 8, 2018
Article in press: November 8, 2018
Published online: December 17, 2018
Processing time: 137 Days and 18.9 Hours
Clear cell papillary renal cell carcinoma (ccpRCC) was recently established as a distinct type of epithelial neoplasm by the International Society of Urological Pathology Vancouver Classification of Renal Neoplasia. Here, we report a case of partial nephrectomy for a ccpRCC detected during the routine follow-up of a previously treated liposarcoma in a 70-year-old male patient. The patient was referred to the urology department for a right-sided renal mass (size: 2 cm) detected during routine annual imaging follow-up for a malignant right inguinal fibrous histocytoma and liposarcoma that had been diagnosed 6 and 4 years earlier, respectively, and treated with surgery and adjuvant radiation therapy. Following partial nephrectomy, the renal mass was pathologically diagnosed as ccpRCC, and immunohistochemistry revealed carbonic anhydrase 9 (CA9) expression. No recurrences or metastases were detected on follow-up imaging for 6 months. This is the first report of partial nephrectomy for incidentally discovered CA9-positive ccpRCC.
Core tip: Clear cell papillary renal cell carcinoma (ccpRCC) was recently established as a distinct type of epithelial neoplasm. Here, we report a case of partial nephrectomy for a ccpRCC detected during the routine follow-up a previously treated liposarcoma in a 70-year-old male patient. The patient received partial nephrectomy, the renal mass was pathologically diagnosed as ccpRCC, and immunohistochemistry revealed carbonic anhydrase 9 (CA9) expression. No recurrences or metastases were detected on follow-up imaging for 6 mo. This is the first report of partial nephrectomy for incidentally discovered CA9-positive ccpRCC.
- Citation: Kim SH, Kwon WA, Joung JY, Seo HK, Lee KH, Chung J. Clear cell papillary renal cell carcinoma: A case report and review of the literature. World J Nephrol 2018; 7(8): 155-160
- URL: https://www.wjgnet.com/2220-6124/full/v7/i8/155.htm
- DOI: https://dx.doi.org/10.5527/wjn.v7.i8.155
Clear cell papillary renal cell carcinoma (ccpRCC), which is also known as clear cell tubulopapillary renal cell carcinoma, is a rare type of malignant renal tumor that differs markedly from other malignant tumor subtypes in terms of visual, microscopic, and immunohistochemical characteristics[1-4]. Cytopathologically, ccpRCC comprises epithelial cells with clear cytoplasm in both tubular and papillary arrangements, and thus exhibits characteristics of both clear cell renal cell carcinoma (ccRCC) and papillary renal cell carcinoma (pRCC). These clear tumor cells harbor a linear array of low-grade nuclei distal from the basement membrane and develop a range of tubular, papillary, and cystic structures. By contrast, atypical and mitotic cells, vascular invasion, necrosis, hyaline globules, foamy macrophages, and pleomorphism are rarely observed.
Although Tickoo et al[5] first identified ccpRCC in the context of end-stage kidney disease in 2006, this entity mainly occurs in normal kidneys and is rare in patients with end-stage or cystic kidney disease[1,2,6]. Recently, the International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia[7,8] recognized ccpRCC as a distinct epithelial tumor that could be distinguished from ccRCC and pRCC by genetic differences in the von Hippel-Lindau (VHL)tumor suppressor gene mutation and 3p loss status and the extreme rarity of gains in chromosomes 7 and 17 or the loss of chromosome Y, despite significant morphological, immunohistochemical, and genetic similarities among the three tumors[9]. Here, we report a case in which partial nephrectomy was used to treat a ccpRCC that was incidentally diagnosed during a recent imaging follow-up in a patient with a history of previously treated liposarcoma and malignant fibrous histiocytoma.
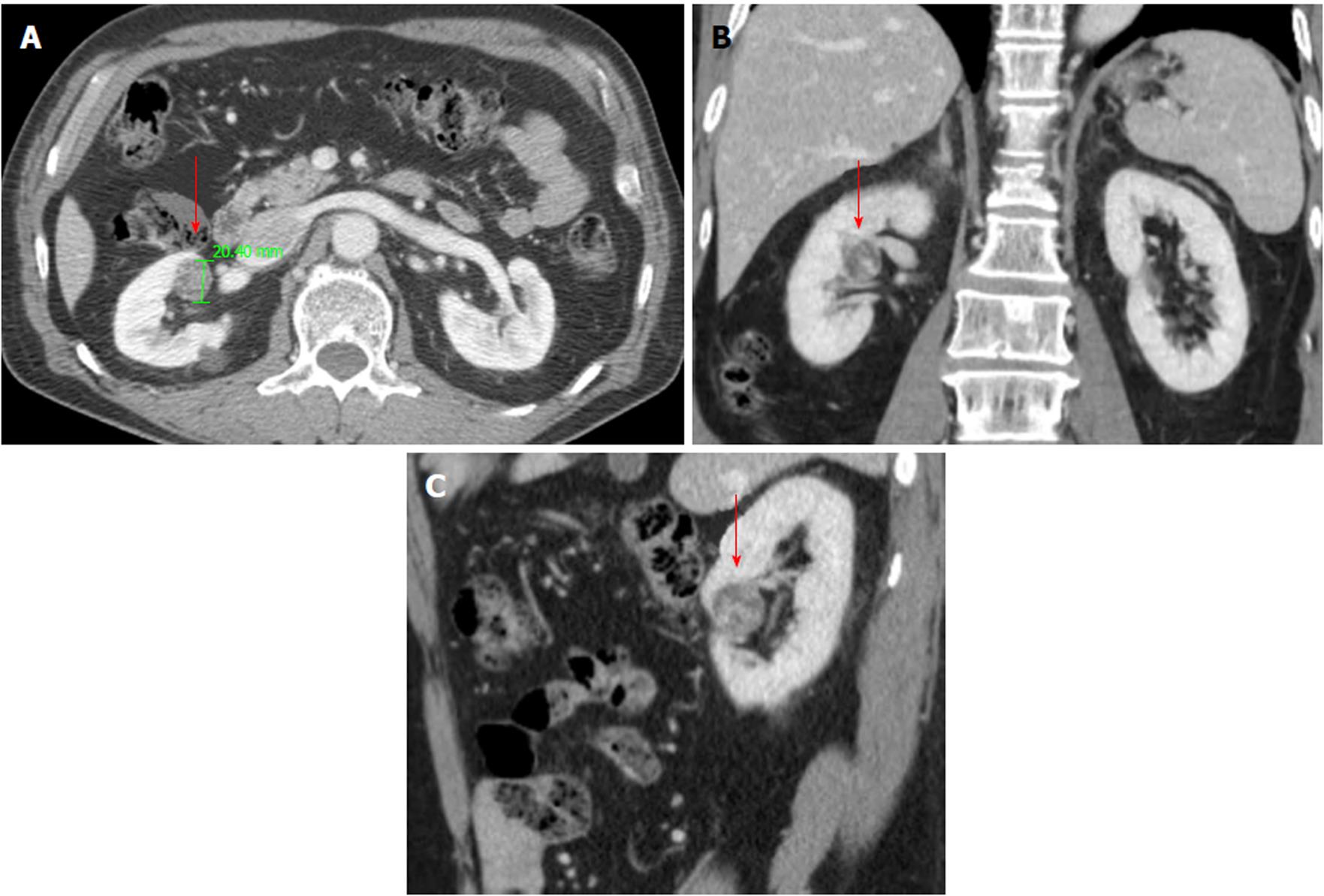
A 17-year-old man was referred to department of urology after a routine computed tomography (CT) scan detected a right-sided enhancing mid-pole renal mass measuring 2.3 cm (Figure 1). He was previously treated for a right-sided inguinal lymph nodal malignant fibrous histiocytoma and right-sided pelvic high-grade pleomorphic and spindle cell sarcoma 6 and 3 years earlier, respectively, via surgical excision in the orthopedic department and radiation therapy (adjuvant dose of 60 Gy/30 fractions to the pelvis) in the radiology department. He had no other underlying diseases such as hypertension or diabetes. The follow-up of the patient included biannual pelvic magnetic resonance imaging (MRI) and chest CT and annual positron emission tomography (PET)-CT. No signs of recurrence or metastasis were identified until the currently described renal mass (Figure 1).
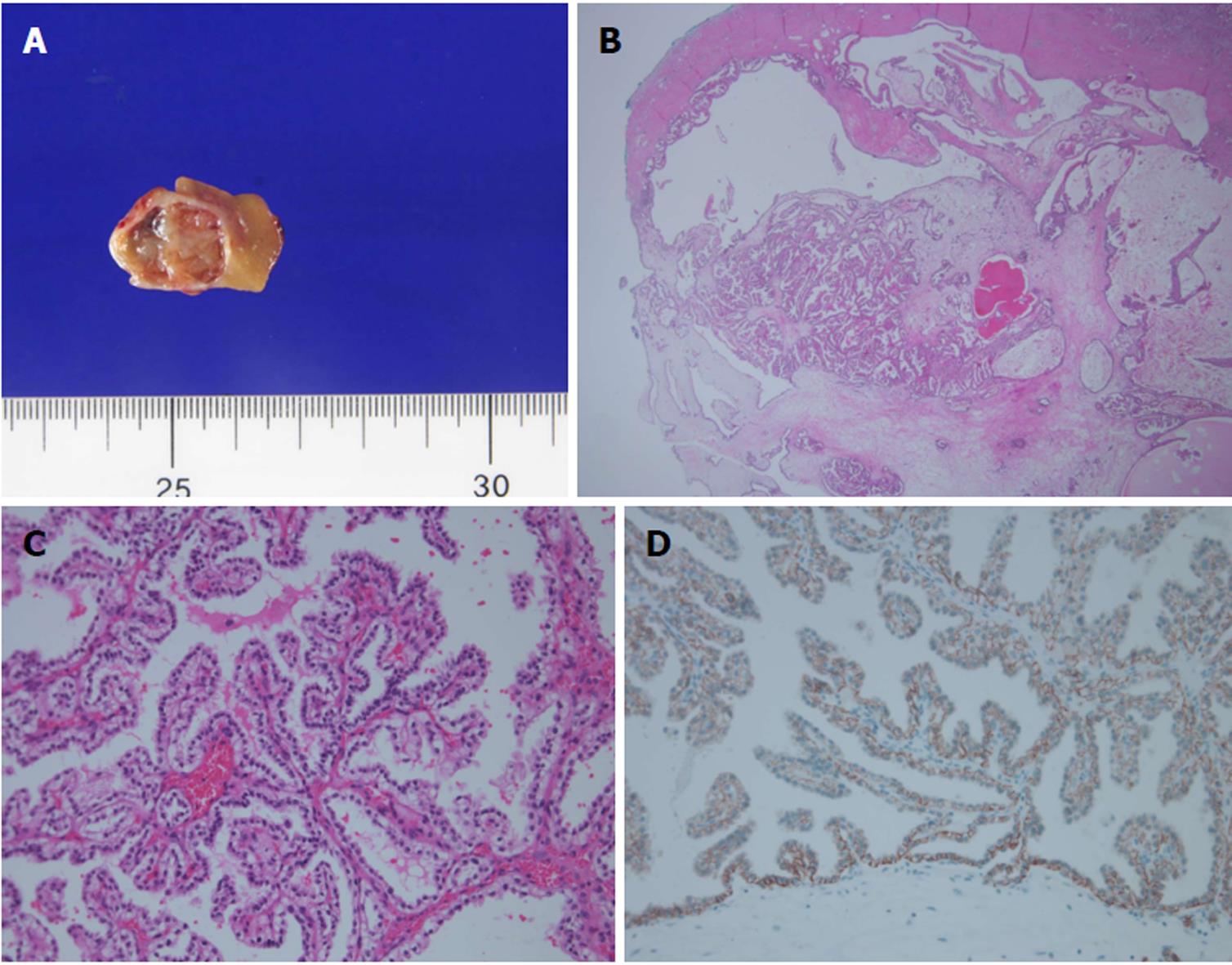
Following a full metastatic work-up, the patient underwent open right-sided partial nephrectomy. Subsequent pathology revealed a tumor measuring 1.7 cm × 1.4 cm × 1.0 cm with a capsule abutting, leading to a diagnosis of a grade 2 ccpRCC without necrosis and a final pathologic stage of T1aN × M0 (Figure 2). The patient was routinely followed at the urology outpatient clinic without any further adjuvant plan for 9 mo postoperatively.
According to the ISUP (ISUP) Vancouver Classification 2012, ccpRCC, which has also been described as clear cell tubulopapillary RCC or renal angio adenomatous tumor (RAT), is a recently recognized type of indolent epithelial tumor of the renal cortex, with a prevalence rate of 1%-4% among all resected asymptomatic renal tumors[7,10]. These tumors exhibit no age or sex prevalence, and no cases of local or nodal recurrence or distant metastasis have been reported[11,12]. However, despite the generally asymptomatic nature of ccpRCC, some patients, including the subject of this case, complain of abdominal or flank pain. Although these tumors may occur in patients with end-stage renal disease or von Hippel-Lindau (VHL) syndrome, most affect normal kidneys[1,2]. The finding that most ccpRCCs are diagnosed as stage 1 (excepting two stage 2 cases)[2,4,9,11] led to the designation of “low malignant potential” in the recent ISUP classification[12].
Imaging studies of ccpRCC indicate hypodense areas with cystic changes or cyst formation on CT and areas of isointensity and hypointensity on T1- and T2-weighted MRI, respectively[13]. ccpRCC frequently appears as a well-defined, well-encapsulated tumor with cystic changes or the formation of cysts[11,12] filled with serosanguinous fluid or colloid-like regions[9]. Morphologically, ccpRCC appears to be an intermediate between ccRCC and pRCC, with low nuclear grading, tubular and papillary arrangement of clear epithelial cells, a predominantly linear nuclear alignment distal from the basement membrane, and a distinctive immunohistochemical profile similar to that of RAT. Multifocality and bilaterality are rarely reported[8,10]. Macroscopically, the cut surface is whitish-tan, with variable surface coloration. Microscopically, most ccpRCCs are small and lack necrosis or invasion of the lymphatic vasculature and renal sinus, but are well-circumscribed and encapsulated with common cystic changes. Proteineous secretions are often observed within the lumina or acini of tubules[3]. Although foamy macrophages, psammoma bodies, and hemosiderin deposits are rarely observed[14], fibrous stroma is common[1] and usually indicates the association of a smooth muscle metaplasia with the tumor capsule[11]. Some previously diagnosed renal angiomyoadenomatous tumors with a predominantly smooth muscle histology have since been recognized as examples of ccpRCC.
Immunohistochemically, ccpRCC is positive for cytokeratin (CK)-7, CA-9, high-molecular-weight CK, Pax2 and Px8, and 34βE12 and negative for CD10 and alpha-methylacyl-CoA racemase[7,8,10]. Concurrent strong, diffuse CK-7 expression and a cup- shaped CA-9 expression pattern is usually considered an immunohistochemical hallmark of ccpRCC; this pattern corresponds with the shape of the neoplastic cell, which is typically cuboidal to low columnar, with round and generally uniform nuclei and inconspicuous linearly arranged nucleoli distal from the basal membrane.
Genetic analysis can be used to further differentiate ccpRCC from ccRCC and pRCC, and comparative genomic hybridization can differentiate sporadic ccpRCC from cases associated with end-stage renal disease. Although VHL mutation is a hallmark of ccRCC, mutations in this gene have been described in 15%-30% of ccpRCC cases. Furthermore, pRCC exhibits a loss of heterogeneity, although this is not accompanied by mutation or promoter methylation. Rather than VHL alterations, pRCC is known to harbor trisomies of chromosomes 7 and 17 and losses of Y, whereas ccpRCC does not exhibit these changes[15]. ccpRCC may occur in normal kidney, non-cystic end stage renal disease and acquired cystic disease[3,11,16,17]. Two cases of ccpRCC occurred within 10 years of hemodialysis[18].
Some cases have been associated with von Hippel-Lindau disease[19]. The association with other renal cancers such as papillary RCC, clear cell RCC, chromophobe RCC, multilocular cystic RCC, acquired cystic disease-associated RCC and renal oncocytoma have also been reported[11,16,20].
Total or partial nephrectomy is generally performed when surgical resection is feasible and the tumor is solitary[1]. Because these tumors are generally indolent, active surveillance with strict follow-up may be possible in selective cases.
In conclusion, this report describes the first case of partial nephrectomy for a ccpRCC that was incidentally diagnosed in an elderly male patient during the imaging follow-up of previously treated tumors. More comprehensive sampling may be warranted to identify the characteristics of ccpRCC with prognostic variables.
The patient was referred to the urology department for a right-sided renal mass (size: 2 cm) detected during routine annual imaging follow-up for a malignant right inguinal fibrous histocytoma and liposarcoma that had been diagnosed 6 and 4 years earlier, respectively.
A routine computed tomography (CT) scan detected a right-sided enhancing mid-pole renal mass measuring 2.3.
Immunohistochemistry revealed carbonic anhydrase 9 (CA9) expression could be helpful for differential diagnosis.
A routine CT scan detected a right-sided enhancing mid-pole renal mass measuring 2.3 cm.
pathology revealed a tumor measuring 1.7 cm × 1.4 cm × 1.0 cm with a capsule abutting, leading to a diagnosis of a grade 2 ccpRCC without necrosis and a final pathologic stage of T1aN × M0.
The patient underwent open right-sided partial nephrectomy.
Patients who have previously been treated with tumor need careful follow-up.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
P- Reviewer: Choi MR, Ekpenyong CEE, Yong D S- Editor: Ji FF L- Editor: A E- Editor: Bian YN
| 1. | Adam J, Couturier J, Molinié V, Vieillefond A, Sibony M. Clear-cell papillary renal cell carcinoma: 24 cases of a distinct low-grade renal tumour and a comparative genomic hybridization array study of seven cases. Histopathology. 2011;58:1064-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Gobbo S, Eble JN, Grignon DJ, Martignoni G, MacLennan GT, Shah RB, Zhang S, Brunelli M, Cheng L. Clear cell papillary renal cell carcinoma: a distinct histopathologic and molecular genetic entity. Am J Surg Pathol. 2008;32:1239-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 189] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 3. | Williamson SR, Eble JN, Cheng L, Grignon DJ. Clear cell papillary renal cell carcinoma: differential diagnosis and extended immunohistochemical profile. Mod Pathol. 2013;26:697-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Gilani SM, Tashjian R, Qu H. Clear cell papillary renal cell carcinoma with characteristic morphology and immunohistochemical staining pattern. Pathologica. 2012;104:101-104. [PubMed] |
| 5. | Tickoo SK, dePeralta-Venturina MN, Harik LR, Worcester HD, Salama ME, Young AN, Moch H, Amin MB. Spectrum of epithelial neoplasms in end-stage renal disease: an experience from 66 tumor-bearing kidneys with emphasis on histologic patterns distinct from those in sporadic adult renal neoplasia. Am J Surg Pathol. 2006;30:141-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 314] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 6. | Aron M, Chang E, Herrera L, Hes O, Hirsch MS, Comperat E, Camparo P, Rao P, Picken M, Michal M. Clear cell-papillary renal cell carcinoma of the kidney not associated with end-stage renal disease: clinicopathologic correlation with expanded immunophenotypic and molecular characterization of a large cohort with emphasis on relationship with renal angiomyoadenomatous tumor. Am J Surg Pathol. 2015;39:873-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Kristiansen G, Delahunt B, Srigley JR, Lüders C, Lunkenheimer JM, Gevensleben H, Thiesler T, Montironi R, Egevad L. [Vancouver classification of renal tumors: Recommendations of the 2012 consensus conference of the International Society of Urological Pathology (ISUP)]. Pathologe. 2015;36:310-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur Urol. 2016;70:93-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1478] [Cited by in RCA: 2070] [Article Influence: 230.0] [Reference Citation Analysis (0)] |
| 9. | Aydin H, Chen L, Cheng L, Vaziri S, He H, Ganapathi R, Delahunt B, Magi-Galluzzi C, Zhou M. Clear cell tubulopapillary renal cell carcinoma: a study of 36 distinctive low-grade epithelial tumors of the kidney. Am J Surg Pathol. 2010;34:1608-1621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 10. | Moch H, Humphrey PA, Ulbright TM, Reuter VE, Eds . Clear cell papillary renal cell carcinoma, vol. 1. 4th ed. Lyon, France: IARC 2016; . |
| 11. | Alexiev BA, Drachenberg CB. Clear cell papillary renal cell carcinoma: Incidence, morphological features, immunohistochemical profile, and biologic behavior: A single institution study. Pathol Res Pract. 2014;210:234-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, Hes O, Moch H, Montironi R, Tickoo SK. The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia. Am J Surg Pathol. 2013;37:1469-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 736] [Cited by in RCA: 754] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 13. | Sahni VA, Hirsch MS, Silverman SG. Renal angiomyoadenomatous tumour: Imaging features. Can Urol Assoc J. 2012;6:E140-E143. [PubMed] |
| 14. | Ross H, Martignoni G, Argani P. Renal cell carcinoma with clear cell and papillary features. Arch Pathol Lab Med. 2012;136:391-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 15. | Shao T, Yousef P, Shipilova I, Saleeb R, Lee JY, Krizova A. Clear cell papillary renal cell carcinoma as part of histologically discordant multifocal renal cell carcinoma: A case report and review of literature. Pathol Res Pract. 2016;212:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Park JH, Lee C, Suh JH, Moon KC. Clear cell papillary renal cell carcinoma: a report of 15 cases including three cases of concurrent other-type renal cell carcinomas. Korean J Pathol. 2012;46:541-547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Bhatnagar R, Alexiev BA. Renal-cell carcinomas in end-stage kidneys: a clinicopathological study with emphasis on clear-cell papillary renal-cell carcinoma and acquired cystic kidney disease-associated carcinoma. Int J Surg Pathol. 2012;20:19-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Nouh MA, Kuroda N, Yamashita M, Hayashida Y, Yano T, Minakuchi J, Taniguchi S, Nomura I, Inui M, Sugimoto M. Renal cell carcinoma in patients with end-stage renal disease: relationship between histological type and duration of dialysis. BJU Int. 2010;105:620-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Rao P, Monzon F, Jonasch E, Matin SF, Tamboli P. Clear cell papillary renal cell carcinoma in patients with von Hippel-Lindau syndrome--clinicopathological features and comparative genomic analysis of 3 cases. Hum Pathol. 2014;45:1966-1972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Zhou H, Zheng S, Truong LD, Ro JY, Ayala AG, Shen SS. Clear cell papillary renal cell carcinoma is the fourth most common histologic type of renal cell carcinoma in 290 consecutive nephrectomies for renal cell carcinoma. Hum Pathol. 2014;45:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |