Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.100427
Revised: December 5, 2024
Accepted: December 27, 2024
Published online: June 18, 2025
Processing time: 189 Days and 9 Hours
Normothermic liver machine perfusion (NMP) is a novel technology used to preserve and evaluate the function of liver allografts.
To assess NMP utilization in liver transplant (LT) practices.
All adult deceased-donor LT recipients between January 2021 and September 2023 in the United States were analyzed. Outcomes including discard rates, survival, preservation time and timing of surgery were compared between two groups: NMP vs non-NMP.
Between 2021 and 2023, NMP was utilized in 1493 (6.3%) of all LTs in the United States. Compared to non-NMP group, NMP group had lower allograft discard rate (6.5% vs 10%, P < 0.001), older recipients’ age (median: 47 vs 42 years, P < 0.001), and higher utilization of donors from donation after circulatory death (DCD) (55% vs 11%, P < 0.001). NMP group also had longer distances between recipient and donor hospitals (median: 156 vs 138 miles, P < 0.001), longer preservation time (median: 12.2 vs 5.8 hours, P < 0.001), and more daytime reperfusion (74% vs 55%, P < 0.001). Post-transplant survival outcomes were comparable between the two groups. In a subgroup analysis of NMP, recipients in the long preservation time (≥ 8 hours) group had higher daytime reperfusion (78% vs 55%, P < 0.001) and similar post-transplant survival when compared to the short preservation time (< 8 hours) group.
The utilization of NMP is associated with lower discard rates and increased DCD organs for LT. NMP allows for prolonging the preservation time and increased occurrence of daytime LT, without any impact on the survival outcomes.
Core Tip: The utilization of normothermic liver machine perfusion is associated with lower discard rates, increased utilization of donation after circulatory death liver allografts and an ability to expand the distance between recipient and donor hospitals, prolong preservation time, and higher occurrence of daytime liver transplant without any negative impact on the survival outcomes.
- Citation: Okumura K, Dhand A, Hasjim BJ, Misawa R, Sogawa H, Veillette G, Nishida S. Liver transplant practices in the era of normothermic machine perfusion in the United States. World J Transplant 2025; 15(2): 100427
- URL: https://www.wjgnet.com/2220-3230/full/v15/i2/100427.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i2.100427
The burden of end-stage liver disease is increasing globally, resulting in a growing demand for liver transplantation (LT)[1]. Despite a steady increase in the number of LTs performed, mortality rates while on the transplant waiting list in the United States remains high due to a shortage of available organs[1]. To expand the donor pool, marginal liver allografts, including liver grafts from donation after cardiac death (DCD), have been increasingly utilized in recent years[2-4].
Normothermic liver machine perfusion (NMP) has emerged as a novel technology with a critical role in the expansion of the donor pool. NMP can help increase the utilization of available liver allografts by reducing ischemic injury and facilitating the assessment of liver physiology before LT[5-8]. Two NMP devices, the Organ Care System and OrganOx metra, were approved by the United States Food and Drug Administration in 2021, and since then the utilization of NMP for LT has been steadily increasing in the United States[9]. Historically, liver allografts were preserved using static cold storage and the goal was to minimize the ischemic time, thereby reducing any potential ischemic injury and associated post-transplant complications. Since NMP enables ongoing allograft perfusion and assessment of its function, it can obviate the critical limiting factor of a shorter ischemic time when using the traditional static cold storage.
Use of NMP is associated with improvement in LT outcomes, especially when using marginal liver allografts[5,10]. However, data regarding its real-world impact on transplant practices, including the timing of transplantation, remains limited. The aim of this study was to assess NMP utilization in LT practices in the United States.
Adult (age ≥ 18 years) deceased donor LT recipients transplanted between January 2021 and September 2023 were analyzed in the de-identified database from the Organ Procurement and Transplant Network (OPTN) Standard Transplant Analysis and Research (STAR) file datasets. The variable “LI_MACHINE_PERFUSION: Liver machine perfusion” was used to identify the liver machine utilization. “LI_MACHINE_ PERFUSION_TYPE: Liver machine perfusion type” was used to identify the type of NMP of liver. The transplant demographics were compared between two groups: NMP and non-NMP. Retransplant and multi-organ transplantation were excluded from the analysis.
Preservation time was defined as the time between donor cross-clamp time and organ reperfusion using cold ischemia time (CIT) in the database since the duration of NMP utilization was not available in the database. Reperfusion time was calculated from the time of donor cross-clamp and CIT. Daytime surgery was defined as surgery between 8 am and 8 pm, which was defined based on previous studies[11,12]. As a subgroup analysis of NMP, the transplant demographics were compared between two groups: Short NMP (preservation time less than 8 hours) vs long NMP (preservation time ≥ 8 hours[13].
Continuous variables were presented as median (interquartile). Mann-Whitney U test was used to compare continuous variables between two groups. A χ2 or Fisher’s exact test was performed for categorical variables. The overall survival and graft survival were calculated from the date of transplant to the date of event using the Kaplan-Meier Method. The log-rank test was used to compare survival curves. Cox-Hazard regression analysis was also applied to analyze with overall and graft survivals. Results were presented as hazard ratios (HR) and reported with 95%CI and two-sided P values. For all statistical analyses, a significance level of P < 0.05 was considered. The statistical analyses were performed using R-Studio using R Version 4.1.1 (R Studio, Boston, MA, United States).
During the study period, a total of 23793 adult LT recipients were identified, of which 1493 (6.3%) of all LT cases utilized NMP.
Compared to non-NMP group, LT recipients in NMP group were older (median age NMP: 59 years vs non-NMP: 57 years, P < 0.001), had lower rates of underlying alcohol liver disease (NMP: 34% vs non-NMP: 44%), higher rate of hepatocellular carcinoma (NMP: 7.8% vs non-NMP: 4.2%), higher prevalence of diabetes (NMP: 32% vs non-MP: 26%, P < 0.001), higher rate of previous abdominal surgery (NMP: 50% vs non-NMP: 45%, P = 0.005), lower model for end-stage liver disease (MELD) score (NMP: 20 vs non-NMP: 26, P < 0.001), lower rate of MELD exception point (NMP: 3.9 % vs non-NMP: 8.7%, P < 0.001), lower rate of hemodialysis utilization (NMP: 8.1% vs non-NMP: 15%, P < 0.001), and a longer waiting time (median NMP: 77 days vs non-NMP: 31 days, P < 0.001) (Table 1). At time of transplant, more recipients in the NMP group were in the outpatient setting (NMP: 70% vs non-NMP: 56%) and less in intensive care unit setting (NMP: 9.0% vs non–NMP: 15%, P < 0.001).
| Variable | NMP (n = 1083) | Non-NMP (n = 18515) | P value |
| Recipient | |||
| Age | 59.0 (51.0-65.0) | 57.0 (47.0-64.0) | < 0.001 |
| Male, | 711 (66) | 11799 (64) | 0.20 |
| Race (White) | 768 (71) | 13096 (71) | 0.088 |
| Black | 48 (4.4) | 1178 (6.4) | |
| Hispanic | 205 (19) | 3179 (17) | |
| Asian | 45 (4.2) | 745 (4.0) | |
| Others | 17 (1.6) | 317 (1.7) | |
| Body mass index (kg/m2) | 28.8 (25.1-32.7) | 28.5 (24.8-32.9) | 0.50 |
| Blood type (A) | 401 (37) | 6621 (36) | < 0.001 |
| AB | 38 (3.5) | 965 (5.2) | |
| B | 107 (9.9) | 2532 (14) | |
| O | 537 (50) | 8397 (45) | |
| Primary diagnosis of liver disease (ALD) | 372 (34) | 8141 (44) | < 0.001 |
| MASH | 240 (22) | 3,809 (21) | |
| Hepatitis C virus | 60 (5.5) | 945 (5.1) | |
| Hepatitis B virus | 15 (1.4) | 312 (1.7) | |
| Acute liver failure | 5 (0.5) | 344 (1.9) | |
| Hepatocellualr carcinoma | 84 (7.8) | 774 (4.2) | |
| Others | 307 (28) | 4190 (23) | |
| Diabetes | 349 (32) | 4838 (26) | < 0.001 |
| HCV seropositive status | 126 (13) | 2209 (12) | 0.77 |
| HCV NAT positive status | 29 (3.3) | 498 (3.7) | 0.57 |
| Previous abdominal surgery | 495 (50) | 8075 (45) | 0.005 |
| Portal vein thrombosis | 147 (15) | 2316 (13) | 0.089 |
| Dialysis at transplant | 86 (8.1) | 2747 (15) | < 0.001 |
| TIPSS | 87 (8.1) | 1316 (7.2) | 0.25 |
| MELD | 20 (13-27) | 26 (17-33) | < 0.001 |
| MELD exception | 42 (3.9) | 1602 (8.7) | < 0.001 |
| Ventilation at transplant | 26 (2.4) | 571 (3.1) | 0.20 |
| Waiting days | 77 (14-272) | 31 (6-198) | < 0.001 |
| Location of patient (missing) | 80 (7.4) | 474 (2.6) | < 0.001 |
| ICU | 98 (9.0) | 2816 (15) | |
| Inpatient | 145 (13) | 4798 (26) | |
| Outpatient | 760 (70) | 10427 (56) | |
| Donor | |||
| Age | 47.0 (34.0-57.0) | 42.0 (31.0-55.0) | < 0.001 |
| Male | 695 (64) | 11528 (62) | 0.21 |
| Race (White) | 724 (67) | 11427 (62) | 0.001 |
| Black | 153 (14) | 3509 (19) | |
| Hispanic | 157 (14) | 2813 (15) | |
| Asian | 31 (2.9) | 500 (2.7) | |
| Others | 18 (1.7) | 266 (1.4) | |
| Blood type (A) | 407 (38) | 6764 (37) | 0.052 |
| AB | 17 (1.6) | 533 (2.9) | |
| B | 118 (11) | 2200 (12) | |
| O | 541 (50) | 9018 (49) | |
| BMI | 28.5 (24.4-33.5) | 27.4 (23.7-32.0) | < 0.001 |
| HCV nucleic acid testing positive | 34 (3.1) | 948 (5.1) | 0.004 |
| HCV antibody positive | 83 (7.7) | 1794 (9.7) | 0.028 |
| DCD donor | 598 (55) | 1976 (11) | < 0.001 |
| Share type: Local | 417 (39) | 6743 (36) | 0.27 |
| Regional | 311 (29) | 5302 (29) | |
| National | 355 (33) | 6470 (35) | |
| Preservation time | 12.20 (8.98-15.79) | 5.75 (4.70-7.00) | < 0.001 |
| Day-time: Recipient reperfusion | 74% | 55% | < 0.001 |
| Day-time: Donor cross-clamp | 60% | 60% | 0.99 |
| DRI | 2.23 (1.85-2.72) | 1.70 (1.45-2.04) | < 0.001 |
| Distance ($) | 156 (43-354) | 138 (40-302) | < 0.001 |
| Length of post-transplant stay | 8 (6-13) | 10 (7-17) | < 0.001 |
Compared to non-NMP group, donors in the NMP group were older (median age NMP group: 47 years vs non-MP: 42 years, P < 0.001), had higher body mass index (NMP: 28.5 vs non-NMP: 27.4, P < 0.001), lower HCV nucleic acid testing positive status (NMP: 3.1% vs non-NMP: 5.1%, P = 0.004), and a higher rate of DCD (NMP: 55% vs non-NMP: 11%, P < 0.001). Overall, the NMP group had the same percentage of local, regional and national donor sharing. The median distance between the donor and the recipient’s hospital was longer in NMP group (NMP: 156 miles vs non-NMP: 138 miles, P < 0.001). The median preservation time was longer in the NMP group (NMP: 12.2 hours vs non-NMP: 5.75 hours, P < 0.001). Donor risk index[13] (DRI) was higher in NMP group (NMP: 2.23 vs non-NMP 1.70, P < 0.001).
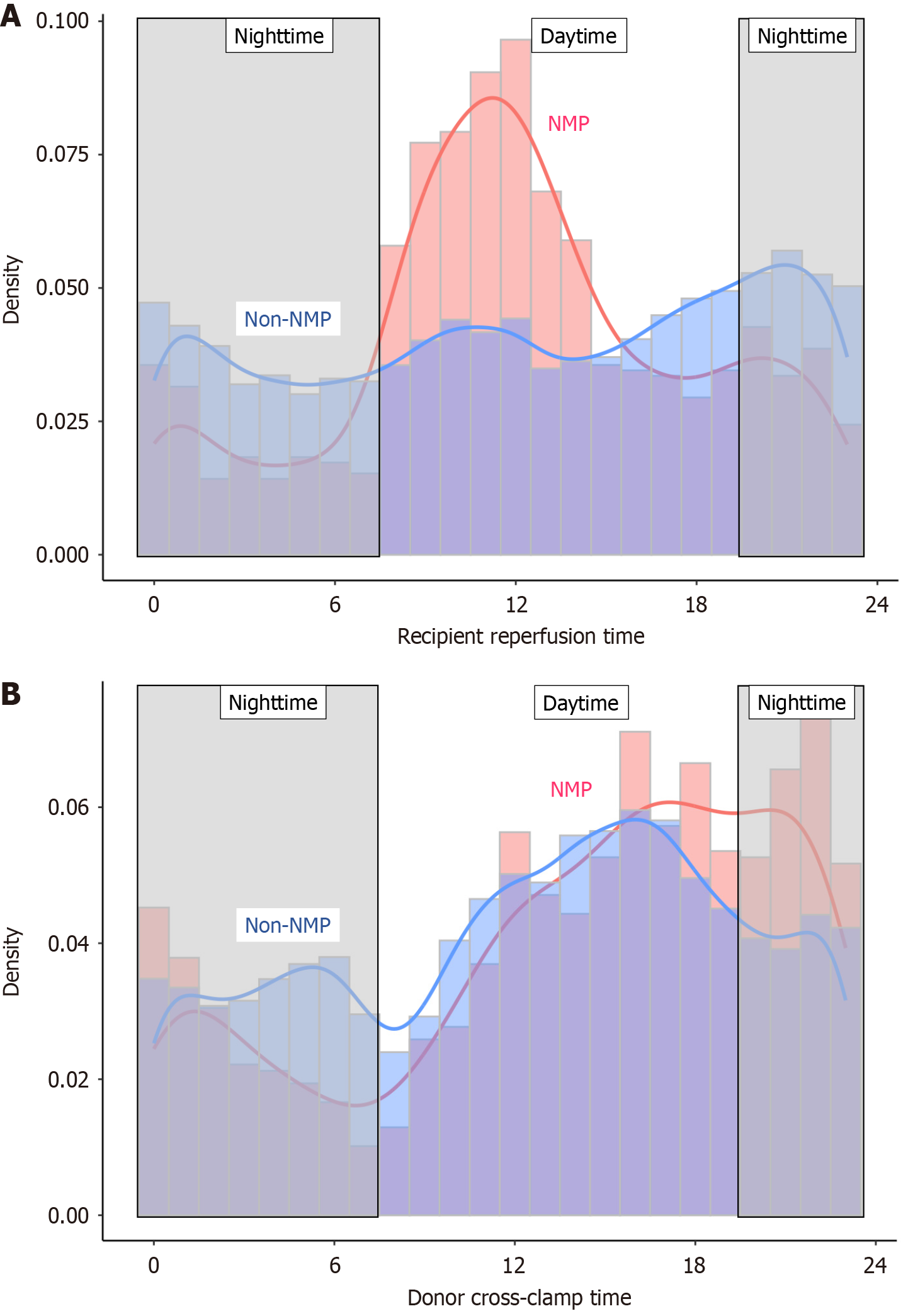
The peak time of reperfusion was 12 p.m. in the NMP group and 9 p.m. in the non-NMP group (Figure 1). The recipient reperfusion time was more during daytime in NMP group (NMP 74% vs non-NMP 55%, P < 0.001), while daytime donor cross-clamp time was same (NMP 60% vs non-NMP 60%, P = 0.99).
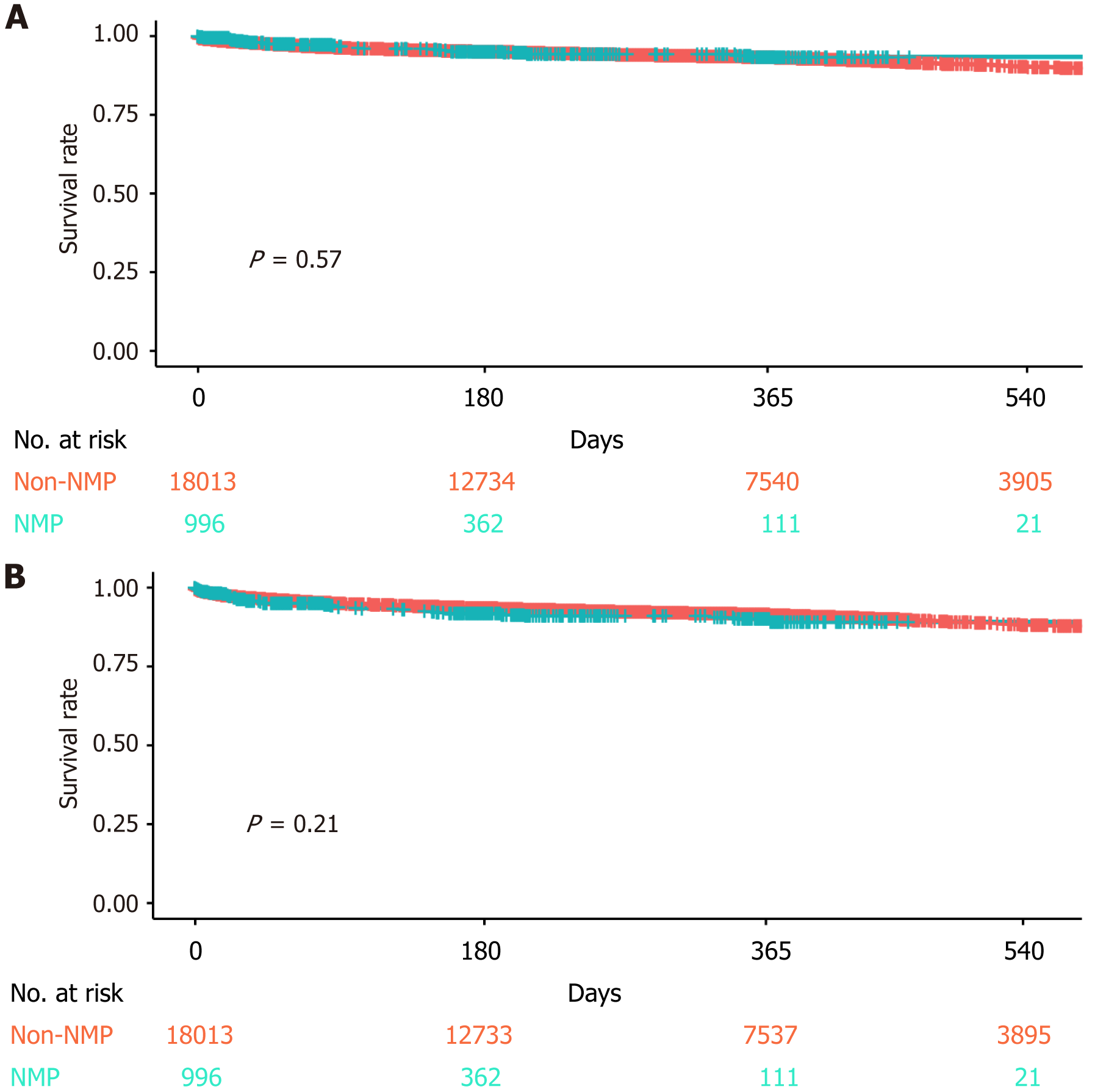
The organ discard rate was significantly lower in NMP group (NMP 6.5% vs non-NMP 10.0%, P < 0.001). The length of post-transplant hospital stay was shorter in NMP group (NMP: 8 days vs non-NMP 10 days, P < 0.001). Post-transplant outcomes were comparable for overall one-year survival (NMP: 93.4% vs non-NMP: 93.3%, HR = 0.90, 95%CI: 0.64-1.28, log-rank P = 0.57) and one-year graft survival (NMP: 90.2% vs non-NMP: 91.6%, HR = 1.18, 95%CI: 0.91-1.54, log-rank P = 0.21) (Figure 2).
In subgroup analysis of NMP group, the median preservation time was 13.5 hours in long NMP and 6.1 hours in short NMP. Recipients of livers with long NMP had higher rate of portal vein thrombosis (long NMP: 16% vs short NMP: 8.8%, P = 0.011) and a lower rate of hemodialysis at the time of LT (long NMP: 6.7% vs short NMP: 12%, P = 0.024), while all other recipient variables were similar between two groups (Supplementary Table 1). Long NMP group included more DCD organs (long NMP: 58% vs short NMP: 48%, P = 0.017). The long NMP group had a higher percentage of national share (long NMP: 34% vs short NMP: 24%) and lower local donor sharing (long NMP: 37% vs short NMP 45%, P = 0.024) with longer distance between donor’s hospital and transplant’s hospital (long NMP: 168 miles vs short NMP: 102 miles, P < 0.001). DRI was higher in long NMP (long NMP: 2.33 vs short NMP: 2.00, P < 0.001). The timing of reperfusion was more during daytime in long NMP (long NMP: 78% vs short NMP: 55%, P < 0.001), even though cross-clamp time was less during daytime in NMP (long NMP 59%: vs short NMP 70%, P = 0.006) (Supplementary Figure 1). The length of post-transplant hospital stay was shorter in long NMP (long NMP: 8 days vs short-NMP: 9 days, P < 0.001). Post-transplant outcomes were comparable for overall one-year survival (long NMP: 93.1% vs short NMP: 95.1%, HR = 1.59, 95%CI: 0.60-4.21, log-rank P = 0.35) and one-year graft survival (long NMP: 89.8% vs short NMP: 92.2%, HR = 1.48, 95%CI: 0.72-3.04, log-rank P = 0.29) (Supplementary Figure 2).
Our study highlights that the utilization of NMP is associated with significant advances in LT practices in the United States. These include a decrease in liver allograft discard rate, increased utilization of DCD organs, and decreased reliance on short ischemia times which result in expanded distances between the donor and transplant hospitals and greater ability to perform LT during daytime hours. When using NMP, longer allograft preservation time did not impact the one-year patient and graft survival.
To improve conventional LT outcomes, efforts to minimize the ischemic time are critical[13,14]. These efforts can impact organ utilization and discard rates, surgeon performance, and place significant demands on the transplant support teams and organ procurement organizations. Since NMP can safely extend the preservation time, one of the proposed benefits of NMP is the ability to schedule LT as a “semi-elective” procedure[8,15]. Our study confirms that when utilizing NMP, the peak timing of reperfusion can be successfully shifted to daytime hours. Although the shift to more daytime reperfusion was associated with longer perfusion times, it exhibited no impact on post-transplant outcomes. Transplant teams led by surgeons and fellows work long and unpredictable hours, perform technically difficult surgeries, and face complex real time patient-care decisions[16]. Because of this challenging lifestyle, transplant surgery is now one of the least popular fellowships among United States-trained graduates[17]. Despite transplant surgeons reporting high level of satisfaction with their choice of careers, the rate of burn-out is very high[18-20]. While several factors contribute to high burn-out among surgeons in general, working for irregular long hours is one of the major factors of physical and mental exhaustion. Sleep deprivation is a known challenge in the transplant surgery community[17]. By using NMP, surgeons have the option of controlling the timing of transplant surgery and avoid sleep deprivation, thereby improving the well-being of transplant surgeons and fellows. Shifting operations to daytime may also improve the overall LT team dynamics.
Since its introduction, NMP in LT has been increasingly utilized in the United States[8,9]. NMP has helped to expand the utilization of marginal liver allografts and has yielded excellent post-transplant outcomes[5,8]. Our group previously showed that, when using machine perfusion for LT, the transplant outcomes between donation after brain death (DBD) and DCD organs were comparable[7]. Increasing the utilization of DCD organs in LT would also help mitigate waitlist mortality and significantly contribute to expanding the donor pool. Without NMP, DCD organ utilization in LT is very time-sensitive, requiring minimization of CIT to avoid the risk of worse outcomes[13,21]. Therefore, by allowing for adjustment in the timing of recipient surgery, NMP can further consolidate its important role in increasing the utilization of DCD organs and in the expansion of the donor pool.
We previously showed that during the early period of NMP in the US, median distance between donor and recipient hospitals when utilizing machine perfusion was short[7]. However, in the present study the median distance for NMP group was longer compared to non-NMP LTs, reflecting the current real-world clinical practices beyond the initial results from the clinical trials. In our subgroup analysis, the long NMP period was associated with a longer distance between transplant hospitals and a higher percentage of national share. While this longer NMP could be attributed to a longer travel time, it may also be related to prolonged assessment of a marginal donor graft under NMP or delaying the surgery to daytime electively. However, since the actual time of utilizing NMP is unknown from the dataset, these causes remain unclear.
There are several limitations of this study utilizing the OPTN STAR datasets. Our analysis was limited to data on transplanted livers, and we lacked granular information such as the duration of NMP, indication of NMP and the additional cost of utilizing NMP, etc. since it was not provided in the database. The changing of the LT timing might not only be at surgeon’s discretion but also influenced by the need of allograft assessment under NMP and by increased travel time. Given that LT is a lengthy procedure, our study used the timing of reperfusion as a marker, but this may not accurately reflect the timing of surgery. Due to the limitations of STAR dataset, this study was not able to analyze other important outcomes such as the biliary or other surgical complications, hospital readmission, or other quality measures.
In summary, the utilization of NMP has helped to advance the field of LT in the United States. It has helped to increase the utilization of liver allografts including DCD, thus lowing the discard rate, extended the preservation time allowing for longer distance between the donor and transplant hospitals, and enabled more daytime transplant surgery. These advances are not only associated with excellent transplant outcomes, but they also contribute to wellness and satisfaction among transplant team members.
The data reported here have been supplied by the United Network for Organ Sharing as the contractor for the OPTN. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the OPTN or the United States Government.
| 1. | Kwong AJ, Ebel NH, Kim WR, Lake JR, Smith JM, Schladt DP, Schnellinger EM, Handarova D, Weiss S, Cafarella M, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2021 Annual Data Report: Liver. Am J Transplant. 2023;23:S178-S263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 181] [Reference Citation Analysis (0)] |
| 2. | Casavilla A, Ramirez C, Shapiro R, Nghiem D, Miracle K, Bronsther O, Randhawa P, Broznick B, Fung JJ, Starzl T. Experience with liver and kidney allografts from non-heart-beating donors. Transplantation. 1995;59:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 273] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 3. | Croome KP, Taner CB. The Changing Landscapes in DCD Liver Transplantation. Curr Transplant Rep. 2020;7:194-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Durand F, Renz JF, Alkofer B, Burra P, Clavien PA, Porte RJ, Freeman RB, Belghiti J. Report of the Paris consensus meeting on expanded criteria donors in liver transplantation. Liver Transpl. 2008;14:1694-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 212] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 5. | Markmann JF, Abouljoud MS, Ghobrial RM, Bhati CS, Pelletier SJ, Lu AD, Ottmann S, Klair T, Eymard C, Roll GR, Magliocca J, Pruett TL, Reyes J, Black SM, Marsh CL, Schnickel G, Kinkhabwala M, Florman SS, Merani S, Demetris AJ, Kimura S, Rizzari M, Saharia A, Levy M, Agarwal A, Cigarroa FG, Eason JD, Syed S, Washburn WK, Parekh J, Moon J, Maskin A, Yeh H, Vagefi PA, MacConmara MP. Impact of Portable Normothermic Blood-Based Machine Perfusion on Outcomes of Liver Transplant: The OCS Liver PROTECT Randomized Clinical Trial. JAMA Surg. 2022;157:189-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 258] [Article Influence: 86.0] [Reference Citation Analysis (0)] |
| 6. | Nasralla D, Coussios CC, Mergental H, Akhtar MZ, Butler AJ, Ceresa CDL, Chiocchia V, Dutton SJ, García-Valdecasas JC, Heaton N, Imber C, Jassem W, Jochmans I, Karani J, Knight SR, Kocabayoglu P, Malagò M, Mirza D, Morris PJ, Pallan A, Paul A, Pavel M, Perera MTPR, Pirenne J, Ravikumar R, Russell L, Upponi S, Watson CJE, Weissenbacher A, Ploeg RJ, Friend PJ; Consortium for Organ Preservation in Europe. A randomized trial of normothermic preservation in liver transplantation. Nature. 2018;557:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 851] [Article Influence: 121.6] [Reference Citation Analysis (0)] |
| 7. | Okumura K, Dhand A, Misawa R, Sogawa H, Veillette G, Nishida S. Outcomes of Liver Transplantation Using Machine Perfusion in Donation after Cardiac Death vs Brain Death in the US. J Am Coll Surg. 2023;236:73-80. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Yamamoto T, Atthota S, Agarwal D, Crisalli K, MacConmara M, Nakamura T, Teo R, Dageforde LA, Kimura S, Elias N, Yeh H, Bozorgzadeh A, Kawai T, Markmann JF. Impact of Portable Normothermic Machine Perfusion for Liver Transplantation From Adult Deceased Donors. Ann Surg. 2023;278:e922-e929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Okumura K, Dhand A, Misawa R, Sogawa H, Veillette G, Nishida S. Utilization of liver machine perfusion is associated with increase in center level liver transplant volume. HPB (Oxford). 2024;26:316-319. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | MacConmara M, Hanish SI, Hwang CS, De Gregorio L, Desai DM, Feizpour CA, Tanriover B, Markmann JF, Zeh H 3rd, Vagefi PA. Making Every Liver Count: Increased Transplant Yield of Donor Livers Through Normothermic Machine Perfusion. Ann Surg. 2020;272:397-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 11. | Lonze BE, Parsikia A, Feyssa EL, Khanmoradi K, Araya VR, Zaki RF, Segev DL, Ortiz JA. Operative start times and complications after liver transplantation. Am J Transplant. 2010;10:1842-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | George TJ, Arnaoutakis GJ, Merlo CA, Kemp CD, Baumgartner WA, Conte JV, Shah AS. Association of operative time of day with outcomes after thoracic organ transplant. JAMA. 2011;305:2193-2199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, Greenstein SM, Merion RM. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1435] [Cited by in RCA: 1486] [Article Influence: 78.2] [Reference Citation Analysis (0)] |
| 14. | Lozanovski VJ, Döhler B, Weiss KH, Mehrabi A, Süsal C. The Differential Influence of Cold Ischemia Time on Outcome After Liver Transplantation for Different Indications-Who Is at Risk? A Collaborative Transplant Study Report. Front Immunol. 2020;11:892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 15. | Das I, Mathur AK, Aqel B, Harnois D, Mao S, Taner CB, Croome KP. " To sleep-perchance to dream ": Daytime surgery start times for liver transplantation with ex situ normothermic machine perfusion. Liver Transpl. 2024;30:763-767. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Jesse MT, Abouljoud M, Eshelman A. Determinants of burnout among transplant surgeons: a national survey in the United States. Am J Transplant. 2015;15:772-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | Vaysburg DM, Delman AM, Sisak S, Turner KM, Ammann AM, Cortez AR, Shah SA, Quillin Iii RC. Biophysiological stress and sleep deprivation among abdominal transplant surgery fellows: A prospective multi-institutional study using a wearable device. Am J Surg. 2023;225: 962-966. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Bertges Yost W, Eshelman A, Raoufi M, Abouljoud MS. A national study of burnout among American transplant surgeons. Transplant Proc. 2005;37:1399-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 87] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Balch CM, Shanafelt TD. Burnout among surgeons: whether specialty makes a difference. Arch Surg. 2011;146:385-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Kassam AF, Cortez AR, Winer LK, Conzen KD, El-Hinnawi A, Jones CM, Matsuoka L, Watkins AC, Collins KM, Bhati C, Selzner M, Sonnenday CJ, Englesbe MJ, Diwan TS, Dick AAS, Quillin RC 3rd. Extinguishing burnout: National analysis of predictors and effects of burnout in abdominal transplant surgery fellows. Am J Transplant. 2021;21:307-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Paterno F, Guarrera JV, Wima K, Diwan T, Cuffy MC, Anwar N, Woodle ES, Shah S. Clinical Implications of Donor Warm and Cold Ischemia Time in Donor After Circulatory Death Liver Transplantation. Liver Transpl. 2019;25:1342-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |