Published online Oct 18, 2021. doi: 10.5500/wjt.v11.i10.421
Peer-review started: February 23, 2021
First decision: May 3, 2021
Revised: May 19, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: October 18, 2021
Processing time: 233 Days and 7 Hours
As the population of the United States ages, there has been an increasing number of elderly patients with cirrhosis listed for transplant. Previous studies have shown variable results in terms of the relative survival benefit for elderly liver transplant (LT) recipients. There may be factors that are associated with a poor post-transplant outcome which may help determine which elderly patients should and should not be listed for LT.
To identify factors associated with futility of transplant in elderly patients.
This was a retrospective study of all patients above the age of 45 who underwent liver transplantation at our tertiary care center between January 2010 and March 2020 (n = 1019). “Elderly” was defined as all patients aged 65 years and older. Futile outcome was defined as death within 90 d of transplant. Logistic regression analysis was performed to determine what variables, if any were associated with futile outcome in elderly patients. Secondary outcomes such as one year mortality and discharge to facility (such as skilled nursing facility or long-term acute care hospital) were analyzed in the entire sample, compared across three age groups (45-54, 55-64, and 65 + years).
There was a total of 260 elderly patients who received LT in the designated time period. A total of 20 patients met the definition of “futile” outcome. The mean Model of End-Stage Liver Disease scores in the futile and non-futile group were not significantly different (21.78 in the futile group vs 19.66 in the “non-futile” group). Of the variables tested, only congestive heart failure was found to have a statistically significant association with futile outcome in LT recipients over the age of 65 (P = 0.001). Of these patients, all had diastolic heart failure with normal ejection fraction and at least grade I diastolic dysfunction as measured on echocardiogram. Patients aged 65 years and older were more likely to have the outcomes of death within 1 year of LT [hazard ratio: 1.937, confidence interval (CI): 1.24-3.02, P = 0.003] and discharge to facility (odds ratio: 1.94, CI: 1.4-2.8, P < 0.001) compared to patients in younger age groups.
Diastolic heart failure in the elderly may be a predictor of futility post liver transplant in elderly patients. Elderly LT recipients may have worse outcomes as compared to younger patients.
Core Tip: This was a retrospective study to identify factors associated with futility of liver transplant (LT) in elderly recipients, as well as investigate the risk of certain outcomes such as discharge to facility in elderly LT recipients. Diastolic congestive heart failure (CHF) was found to be a predictor of futility of LT in elderly recipients (P = 0.001). Elderly patients also had nearly twice the risk of being discharged to a facility and had decreased survival at one year. Diastolic CHF may be an important comor
- Citation: Kleb C, Faisal MS, Quintini C, Miller CM, Menon KVN, Modaresi Esfeh J. Factors predicting futility of liver transplant in elderly recipients: A single-center experience. World J Transplant 2021; 11(10): 421-431
- URL: https://www.wjgnet.com/2220-3230/full/v11/i10/421.htm
- DOI: https://dx.doi.org/10.5500/wjt.v11.i10.421
As the population of the United States ages, the average age of patients awaiting liver transplantation has increased as well[1]. In 2018, adults aged 65 or older made up 24.1% of the United States liver transplant waiting list. This is twice the proportion of patients in this age group on the waiting list 10 years prior[2]. Along with the aging of the entire United States population, the increase in older patients awaiting transplant can also in part be attributed to the aging of those born between 1945 and 1965, a cohort that has high rates of hepatitis C virus infection[1,3]. The current American Association for the Study of Liver Disease (AASLD) guidelines state that age by itself is not a contraindication to liver transplant (LT), and when deciding whether or not to list a patient aged 70 years or older, functional status and comorbidities must be considered[4].
Transplant committees are faced with a difficult decision when deciding whether to list elderly recipients for LT. Despite efforts to expand the donor organ pool through practices such as living donor, split organ, and expanding eligible organs to include donation after cardiac death organs, there remains a critical shortage of donor organs in the United States[5]. Considering the scarcity of organs, transplant committees may be more motivated to allocate this precious resource to patients who would benefit the most from organ transplantation in terms of survival. For these reasons, avoiding futility in LT plays a major role in decision making.
In the literature, futility in LT has been defined in several different ways. Various definitions include situations in which the patient’s post-transplant mortality is greater than the waiting list mortality, death within one year of transplant, death within 90 d, or more qualitative definitions such as poor quality of life and inability to survive outside of an intensive care unit (ICU) setting post-transplant[6].
Despite the extensive amount of research that exists on this topic, there is no conclusive guideline for how to select which elderly patients are suitable for LT. Nevertheless, it is important to avoid futility in transplant, especially when the donor pool is scarce. The purpose of this study is to identify LT recipient factors in the elderly associated with futility of LT. We also aimed to investigate whether certain secondary outcomes such as mortality at one year, discharge to facility [such as skilled nursing facility (SNF) or long-term acute care hospital] and hospital length of stay (LOS) are more common in elderly LT recipients.
This was a study of patients who underwent LT at our center. Inclusion criteria included having received LT between January 2010 and March of 2020, and age of 45 years and above. Exclusion criteria included patients who had multi-organ transplants or repeat transplants. This study was approved by our center’s Institutional Review Board. All statistical work was done using SPSS v.26.0.
From these patients, we sought to identify factors associated with futility of LT. We defined a “futile” outcome as death within 90 d after transplant. We defined “elderly” as a patient aged 65 years or older. Student t-test or Mann-Whitney-U test were used to compare continuous variables. Kruskal Wallis test was used to compare continuous variables across three categories. Categorical variables were compared using chi-square tests or Fisher exact test.
From these results, multifactorial binary logistic regression analysis was carried out to analyze futile transplant data for ages greater than 65 years. Variables that were thought to have higher effect size and high clinical significance were chosen for the model [Model of End-Stage Liver Disease (MELD)-Sodium, Child-Pugh Score (CPS), age at transplant].
In addition to the futility analysis, we also investigated several other outcomes (one year mortality, ICU LOS, hospital LOS, and discharge to facility) in three age groups (45-54 years, 55-64 years, and 65 years and older). For comparison of ICU LOS and total hospital LOS, patients with death during the hospitalization were excluded to eliminate bias in the results, as they would have a falsely decreased LOS. Multi
From our original sample of all patients who received LT at our center between January 2010 and March of 2020 aged 45 years and older (n = 1147), 128 patients who had multi-organ transplants or repeat transplants were excluded, resulting in a total sample size of 1019 patients. 266 patients were between the ages of 45 and 54 (26.1%), and 493 patients were between the ages of 55 and 64 (48.4%). 260 patients (25.5%) were 65 years of age or above. The average ages in the 45-54, 55-64, and 65 years and older groups were 50.7, 59.5 and 67.8, respectively. 67.3% of patients in the study population were male and 32.7% were female. All three age groups were majority male as well (63.2%, 71.0% and 64.3% in the 45-54, 55-64 and 65 years and older age groups, respectively). The most common underlying causes of liver disease were alcohol related cirrhosis (33.1%) in patients aged 45-54, viral hepatitis in the 55-64 years age group (33.7%) and non-alcoholic steatohepatitis in the 65 years and older age group (33.1%). The mean MELD-Na scores in the 45-54, 55-64, and 65 years and older groups were 21.4, 20.4 and 19.8, respectively (P = 0.236).
Of the 260 patients above the age of 65, twenty of these met the definition of futile outcome (death within 90 d after transplant). The mean MELD-Na in the futile group was 21.8, compared with 19.7 in the non-futile group (P = 0.236). The mean age in the futile group was 67.3 years and 67.8 years in the non-futile group (P = 0.821).
Of the factors we investigated, including various comorbidities, Karnofsky performance index (KPI), and indicators of severity of liver disease (MELD-Na and CPS), only congestive heart failure (CHF) was more common in the patient group with futile outcome (30% in the futile group as compared to 5% in the non-futile group, P = 0.001) (Table 1). Chart review indicated that all these patients in both the futile and non-futile group had heart failure with preserved ejection fraction, and all had diastolic dysfunction seen on echocardiogram prior to LT. Four of these patients (20%) had grade I diastolic dysfunction, and 16 (80%) had grade II diastolic dysfunction.
| Characteristic | Death within 90 d, N = 20 | Survival beyond 90 d, N = 240 | P value |
| Age, mean ± SD | 67.30 ± 1.78 | 67.81 ± 2.71 | 0.821 |
| Year of transplant, median (percentiles) | 2014 (2012-2016) | 2015 (2013-2018) | 0.183 |
| Comorbid conditions, n (%) | |||
| Obesity | 6 (30.0) | 57 (23.8) | 0.590 |
| CHF | 6 (30.0) | 12 (5.0) | 0.001a |
| CKD | 1 (5.0) | 23 (9.6) | 0.705 |
| HTN | 14 (70.0) | 152 (63.3) | 0.550 |
| DM | 9 (45.0) | 109 (45.4) | 0.971 |
| CAD | 8 (40.0) | 73 (30.4) | 0.374 |
| PH | 2 (10.0) | 9 (3.8) | 0.203 |
| Arrhythmias | 3 (15.0) | 32 (13.3) | 0.739 |
| Pre-transplant severity of disease | |||
| Ascites | |||
| None | 2 (10.0) | 34 (14.2) | 0.269 |
| Mild | 7 (35.0) | 111 (46.3) | |
| Moderate | 3 (15.0) | 45 (18.8) | |
| Severe | 8 (40.0) | 50 (20.8) | |
| Encephalopathy | |||
| None | 3 (15.0) | 61 (25.4) | 0.397 |
| Grade 1-2 | 17 (85.0) | 172 (71.7) | |
| Grade 3-4 | 0 (0) | 7 (2.9) | |
| Child-Pugh Score | 9.8 +/- 1.7 | 9.08 +/- 2.0 | 0.127 |
| A | 0 (0) | 26 (10.5) | 0.257 |
| B | 8 (40) | 116 (48.3) | |
| C | 12 (60.0) | 98 (40.8) | |
| Karnofsky performance index | 53.50 ± 20.1 | 55.69 ± 21.6 | 0.555 |
| Indication for transplant, n (%) | |||
| Cirrhosis | 16 (80.0) | 147 (56.5) | 0.143 |
| NASH | 6 (30.0) | 54 (22.5) | 0.419 |
| Autoimmune | 2 (10.0) | 3 (1.3) | 0.049 |
| Alcohol | 2 (10.0) | 32 (13.3) | 0.999 |
| Hepatitis C | 2 (10.0) | 18 (7.5) | 0.658 |
| Cryptogenic | 1 (5.0) | 14 (5.8) | 0.999 |
| PSC | 0 (0) | 11 (4.6) | 0.999 |
| PBC | 2 (10.0) | 11 (4.6) | 0.263 |
| Hemochromatosis | 0 (0) | 4 (1.7) | 0.999 |
| HCC and cirrhosis | 4 (20.0) | 87 (36.3) | 0.143 |
| Acute liver failure | 0 (0) | 6 (2.5) | 0.999 |
| Primary etiology of liver disease, n (%) | |||
| Alcohol related cirrhosis | 2 (10) | 46 (19.2) | 0.55 |
| NASH cirrhosis | 8 (40) | 78 (32.5) | 0.49 |
| Cirrhosis due to viral hepatitis | 2 (10) | 48 (20) | 0.38 |
| Other | 8 (40) | 68 (28.3) | 0.27 |
| Lab values, mean ± SD | |||
| Sodium | 135.70 ± 4.3 | 136.12 ± 4.3 | 0.678 |
| INR | 1.51 ± 0.4 | 1.49 ± 0.5 | 0.241 |
| Creatinine | 1.68 ± 1.0 | 1.45 ± 1.0 | 0.133 |
| Total Bili | 6.34 ± 6.8 | 5.46 ± 7.8 | 0.271 |
| MELD-Sodium | 21.78 ± 8.6 | 19.66 ± 9.0 | 0.236 |
| Albumin | 3.16 ± 0.6 | 3.18 ± 0.6 | 0.889 |
We performed binary logistic regression analysis to determine if CHF was an independent predictor of the outcome of death within 90 d of transplant after adjusting for possible confounders such as MELD-Sodium, age at transplant, and CPS. We found that even after adjusting for these factors, a diagnosis of diastolic CHF was still associated with mortality within 90 d of transplant with an adjusted odds ratio (OR) of 9.44 [confidence interval (CI): 2.89-30.81, P < 0.0001]. MELD-Sodium, age, and CPS were not predictors of 90 d mortality (Table 2).
| Variable | Adjusted OR | Confidence interval | P value |
| MELD-Na | 1.02 | 0.95-1.09 | 0.615 |
| Age at transplant | 1.09 | 0.89-1.32 | 0.421 |
| CPS-C vs CPS A and B | 3.25 | 0.86-12.25 | 0.081 |
| CHF | 9.44 | 2.89-30.81 | < 0.0001 |
In addition to investigating factors associated with futility of LT, we also investigated several additional outcomes in patients split into three age groups, to see if these outcomes were more likely to occur in the older cohort. Table 3 shows the results of our analysis of secondary outcomes between the three age groups. Our analysis found that patients aged 65 and older were more likely to have the outcome of death within one year of LT, and had longer total hospital lengths of stay (16.8 +/- standard deviation of 23.9 d, compared to 13.22 +/- 15.4 and 14.14 +/- 24 d in the 45-54 years and 55-64 years age groups, respectively). Patients aged 65 years and older were also less likely to be discharged to home or home with home health care, compared to discharge to facilities such as rehabilitation or nursing facilities. Patients 65 or older were almost twice as likely to be discharged to a facility: Long term acute care hospital/SNF/acute rehab facility, OR: 1.94 (CI: 1.4-2.8, P < 0.001) compared to patients younger than 65. Patients who died during hospitalization following LT were excluded from this analysis.
| Age category | 45-54 years | 55-64 years | ≥ 65 years | P value |
| 30-d mortality (n, %) | 8 (3.0) | 12 (2.4) | 10 (3.8) | 0.55 |
| 1-yr mortality (n, %) | 32 (12.0) | 75 (15.2) | 59 (22.7) | 0.03 |
| ICU LOS | ||||
| mean ± SD | 3.80 ± 6.8 | 3.99 ± 6.8 | 4.17 ± 6.6 | 0.320 |
| Median (IQR) | 2.0 (1.0-3.0) | 2.0 (1.0-4.0) | 2.0 (1.0-4.0) | |
| Total hospitalization | ||||
| mean ± SD | 13.22 ± 15.4 | 14.14 ± 24.0 | 16.8 ± 23.9 | 0.034 |
| Median (IQR) | 10.0 (7.0-14.0) | 10.0 (7.0-15.0) | 11.0 (8.0-17.0) | |
| Discharge disposition (n = 890) (n, %) | ||||
| Home | 182 (76.2) | 314 (73.4) | 133 (59.6) | 0.000 |
| Home or HHC | 190 (79.5) | 329 (76.9) | 142 (63.7) | 0.000 |
| Any facility other than home [excluding patients who died during hospitalization, n = 854)] | 42 (18.1) | 84 (20.3) | 67 (32.1) | 0.001 |
| Acute Rehab | 13 (5.4) | 7 (4.0) | 9 (4.0) | |
| LTAC | 9 (3.8) | 21 (4.9) | 13 (5.8) | |
| SNF | 20 (8.4) | 45 (10.5) | 45 (20.2) | |
| Deceased | 7 (2.9) | 15 (3.5) | 14 (6.3) | |
| Hospice | 0 | 1 (0.2) | 0 |
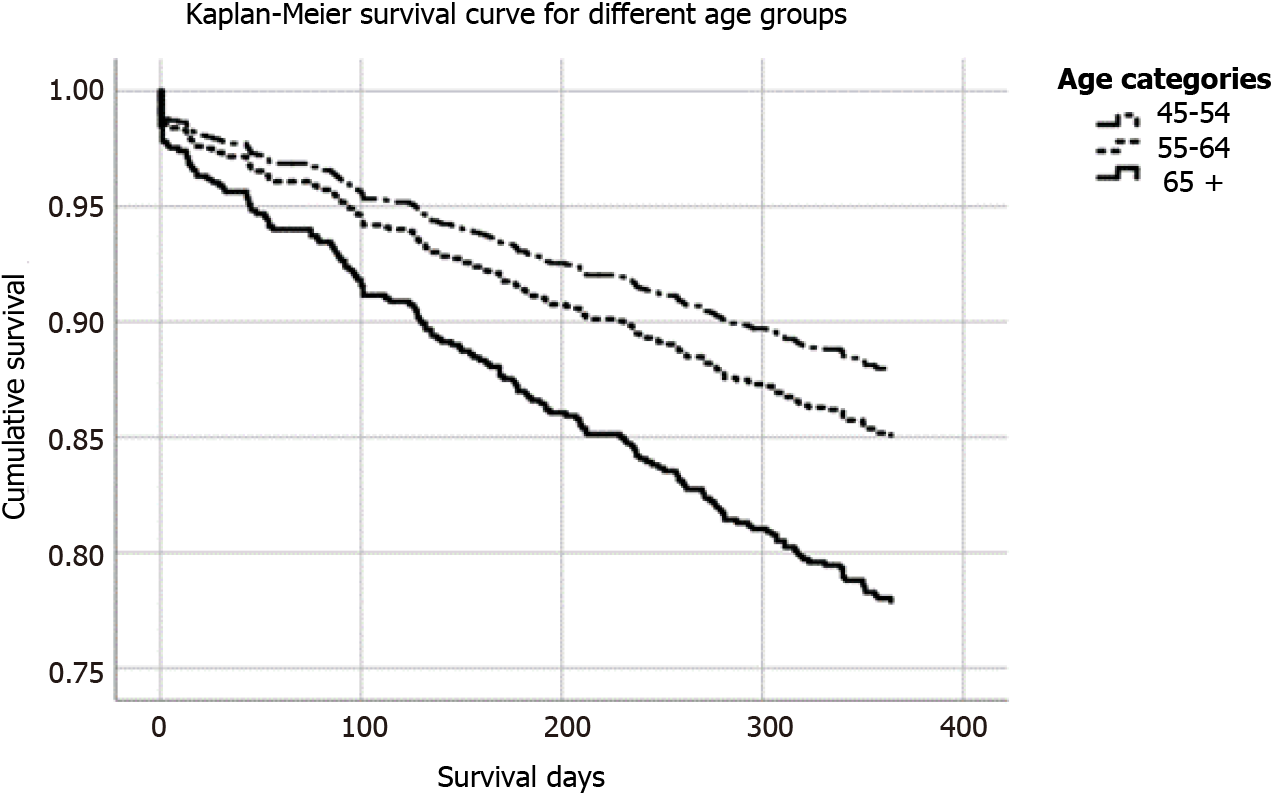
In addition, we also performed Cox Regression Survival Analysis to determine if patients 65 years and older had increased mortality after one year after adjusting for severity of liver disease and comorbidities (Table 4, Figure 1). This showed that even after adjusting for severity of liver disease with MELD-Sodium and multiple co
| Factor | Hazard ratio | P value | 95%CI | |
| Lower | Upper | |||
| MELD-Na | 1.011 | 0.174 | 0.995 | 1.028 |
| CHF | 1.425 | 0.210 | 0.819 | 2.480 |
| Obesity | 0.907 | 0.618 | 0.617 | 1.333 |
| Hypertension | 0.967 | 0.839 | 0.697 | 1.341 |
| Type 2 diabetes | 1.210 | 0.252 | 0.873 | 1.678 |
| Coronary artery disease | 1.054 | 0.781 | 0.726 | 1.532 |
| Age 55-64 vs Age < 55 | 1.252 | 0.293 | 0.824 | 1.902 |
| Pulmonary hypertension | 1.209 | 0.539 | 0.660 | 2.217 |
| Age > 65 vs Age <65 | 1.937 | .003 | 1.244 | 3.017 |
The purpose of this study was to identify factors that are associated with futility of LT in elderly recipients, in order to help with difficult decisions LT selection committees face when choosing whether to list elderly patients. Regardless of their age, LT candidates must go through rigorous screening processes before being listed for LT[4]. This is to ensure that the donor organ, which is a scarce resource in our country[5] is going to candidates that will benefit the most from it. This decision is made even more complex when the candidate in question is elderly, and by virtue of age already has a shorter life expectancy than younger candidates.
Previous research has produced conflicting results about survival in elderly LT recipients as compared to younger patients. A 2007 single-center study of survival outcomes in orthotopic liver transplantation recipients aged 70 years and older as compared to those aged 50 to 59 years found that the unadjusted patient survival at 1, 3, 5 and 10 years was not significantly different between these two groups. This study also found that on multivariate analysis in this population, age ≥ 70 was not an independent predictor of increased mortality in this population[7]. However, a 2018 Korean study found that patients aged 70 years or older had a fourfold higher risk of in-hospital mortality when adjusting for baseline cause of liver disease, and a threefold higher risk of in-hospital mortality when controlling for cause of liver disease and perioperative complications such as need for vasopressor support, ventilator support and extracorporeal membrane oxygenation[8]. A large-scale study utilizing data from the United Network for Organ Sharing (UNOS) transplant database found that post-transplant survival decreased with increased age. However, when stratifying patients with the same MELD score into different age groups, there was no statistically significant difference in survival benefit at five years between these groups. However, this study noted that the reason that the survival benefit was preserved in older age groups was likely because pre-transplantation survival (i.e., waitlist mortality) and post-transplantation survival were equally reduced in older patients. Therefore, the net difference in waitlist and post-transplantation life expectancy was the same between elderly patients and younger cohorts[1].
There have been a few studies investigating what factors are associated with futility of LT. One study found that in patients who received LT while requiring ICU level care, factors associated with the primary outcome of 90-d mortality included high pre-transplant lactate level and the presence of acute respiratory distress syndrome[9]. A second study identifying factors associated with futility of LT in patients with MELD score ≥ 40 (defined as death within 90 d of transplant) found that pretransplant septic shock, cardiac risk, and comorbidities were independent predictors of this outcome[10]. There have also been some studies investigating which recipient factors are associated with a poor outcome in elderly patients. A study of LT patients above the age of 60 who received LT between 2004 and 2010 at our own center showed that hepatic encephalopathy, significant thrombocytopenia (platelet count less than 45000), total serum bilirubin > 3.5 mg/dL, and hypoalbuminemia (< 2.65 mg/dL) were independent predictors of one year mortality[11]. A second study using data from the UNOS database found that on multivariate analysis, factors such as low albumin, recipient diabetes mellitus, elevated creatinine, and recipient hepatitis C positivity were associated with increased mortality in LT recipients above the age of 60 years[12].
For the purpose of this study, we defined “futile” as death within 90 d of transplant. This definition was derived from previous studies that have defined futility in this way[9,10]. Our study found that patients who had a futile outcome after LT were significantly more likely to have a diagnosis of heart failure with preserved ejection fraction, with diastolic dysfunction seen on echocardiogram (30% vs 5%, P = 0.001). This association persisted with logistic regression modeling adjusting for MELD, age at transplant and CPS. Other factors such as KPI, MELD, CPS or other comorbidities did not show any significant difference in scale or incidence between the futile and non-futile groups.
Though to our knowledge ours is the first study to demonstrate the strong linkage between futility of LT in elderly patients and diastolic heart failure, there has been some research in the past on diastolic dysfunction’s role in patients with cirrhosis. One study found that diastolic dysfunction seen on echocardiogram was associated with decreased survival, was a predictor of hepatorenal syndrome, and that survival decreased with increased severity of diastolic dysfunction (i.e., grade I vs grade II)[13]. This is thought to be due to the phenomenon of “cirrhotic cardiomyopathy”, characterized by a blunted cardiovascular response to stress and impaired relaxation of the ventricles. Cirrhotic cardiomyopathy has been attributed to various physiologic and chemical changes in cirrhotic patients, and is essentially heart failure due to impaired diastolic function that occurs in the absence of primary heart disease. It is thought that in patients with cirrhotic cardiomyopathy, after an event such as liver transplantation there is a dramatic increase in preload to a heart that has profound diastolic dys
Since we have found that diastolic CHF was an independent predictor of futile outcome in elderly patients, it may be useful to screen elderly patients more carefully for diastolic dysfunction, and use this as a tool when deciding whether to list elderly patients for LT. However, heart failure with preserved ejection fraction is difficult to diagnose based on echocardiogram as there are many different echocardiographic features that can be associated with diastolic heart failure, but few that are diagnostic[15]. The clinical diagnosis of heart failure with preserved ejection fraction includes the presence of exertional dyspnea and peripheral edema; however, these are symptoms that can be seen as a result of liver disease as well, so it may be difficult to make the diagnosis of diastolic heart failure in these patients[14].
The presence of coronary artery disease (CAD) was not significantly different between the futile and non-futile group, nor between patients who died within one year of transplant and patients who survived beyond one year. Interestingly, this is in contrast to a 2014 study done at our institution of patients aged 60 years or older who received LT between the years of 2004-2010, which found that CAD was an in
A clear limitation to our futility analysis is the small number of people who met our definition of “futile outcome”, or death within 90 d of LT. In our sample, only 20 patients aged 65 and older died within 90 d of LT, out of 260 total patients in this age group that received LT at our center. This small number reduced our study’s power. Therefore, it may be that some of the factors we investigated (MELD, CPS, KPI and various comorbidities) are linked to futility and our small sample size prevents us from seeing these associations. An interesting future direction would be to expand this analysis to include multiple centers to see if any of the other factors we investigated would be significantly associated with futility if the study were adequately powered. The small sample size also prohibited us from adjusting for more than a few covariates in our logistic regression analysis. We chose to adjust for MELD, CPS, and age at transplant since we thought these might be the biggest confounders, but there are other factors such as concurrent comorbidities that may have confounded our data.
The fact that elderly LT recipients have longer hospital LOS and are more likely to be discharged to facility is an important finding because both longer LOS and facility care are costly to our healthcare system[16]. This is also important because im
Survival analysis showed that patients aged 65 years or older had decreased one-year survival even when adjusting for severity of liver disease and comorbidities. This adds to the body of literature that has produced somewhat conflicting results about whether age has a significant impact on post-LT survival. However, it should be noted that though we found that one year mortality after LT was higher in elderly patients, it may be that these results are confounded by the fact that elderly patients have decreased survival overall. One previous study accounted for this in their survival analysis and found that though survival after LT is reduced in elderly patients, the survival benefit is preserved[1]. It may be that this is also the case in our patient population, but calculation of survival benefit is complex and beyond the scope of this paper.
In conclusion, heart failure with preserved ejection fraction and diastolic dysfunction should be used as an important tool when prognosticating elderly LT candidates. Diastolic dysfunction may be an indicator of cirrhotic cardiomyopathy, which is associated with very severe liver disease[14] and may be an indicator of poor outcome after LT as well. It may be useful to consider screening for diastolic heart failure more aggressively in elderly patients. When considering elderly patients for LT, patients and transplant committees should be aware that elderly LT recipients may be more likely to need post-acute placement in a facility and have a longer hospital course, which have important financial implications. It is important to consider the impact of transplanting elderly individuals may have on healthcare expenditures, and make these patients aware of the possible need for an extended recovery. We hope that this study will contribute to the body of evidence on this topic to aid LT selection committees in the allocation of a precious resource.
The average age of patients awaiting liver transplant (LT) in the United States is increasing. Previous research on the effect of age on post-LT outcomes has produced conflicting results.
The donor pool for LT remains limited and donor organs is a precious resource. Thus, avoiding futility of transplant is important.
The objective of this study was to identify factors associated with futility of LT in elderly patients, to help inform the decision whether or not to list elderly patients with liver disease for transplant. We also aimed to investigate relevant post-transplant outcomes in elderly patients.
This study included all patients above the age of 45 who underwent LT at our center over a ten-year period (2010-2020). Of these patients, 260 were 65 years of age or older. In the elderly cohort, several patient factors were analyzed to determine if they were associated with a “futile” outcome defined as death within 90 d after transplant. We also analyzed three different age groups for secondary outcomes such as hospital length of stay (LOS), intensive care unit LOS and discharge to facility.
Diastolic congestive heart failure (CHF) was independently associated with futility of LT after adjusting for potential confounders. Elderly LT recipients had higher one year mortality, longer hospital LOS and were more likely to be discharged to a facility.
Diastolic CHF may be a prognostic indicator for futility of LT in elderly patients. This comorbidity should be considered as part of the pre-LT evaluation.
Further research is needed with a larger sample size, perhaps including multiple centers to determine if there are any other patient comorbidities (or other factors such as functional status and primary cause of liver disease) are associated with futility of LT in elderly patients.
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Wang K S-Editor: Wang JJ L-Editor: A P-Editor: Yuan YY
| 1. | Su F, Yu L, Berry K, Liou IW, Landis CS, Rayhill SC, Reyes JD, Ioannou GN. Aging of Liver Transplant Registrants and Recipients: Trends and Impact on Waitlist Outcomes, Post-Transplantation Outcomes, and Transplant-Related Survival Benefit. Gastroenterology. 2016;150:441-53.e6; quiz e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 151] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 2. | Kwong A, Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, Noreen SM, Foutz J, Miller E, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2018 Annual Data Report: Liver. Am J Transplant. 2020;20 Suppl s1:193-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 312] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 3. | Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62:1353-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 334] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 4. | Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 691] [Article Influence: 62.8] [Reference Citation Analysis (1)] |
| 5. | Saidi RF, Hejazii Kenari SK. Challenges of organ shortage for transplantation: solutions and opportunities. Int J Organ Transplant Med. 2014;5:87-96. [PubMed] |
| 6. | Linecker M, Krones T, Berg T, Niemann CU, Steadman RH, Dutkowski P, Clavien PA, Busuttil RW, Truog RD, Petrowsky H. Potentially inappropriate liver transplantation in the era of the "sickest first" policy - A search for the upper limits. J Hepatol. 2018;68:798-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 84] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 7. | Lipshutz GS, Hiatt J, Ghobrial RM, Farmer DG, Martinez MM, Yersiz H, Gornbein J, Busuttil RW. Outcome of liver transplantation in septuagenarians: a single-center experience. Arch Surg. 2007;142:775-781; discussion 781-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Chen HP, Tsai YF, Lin JR, Liu FC, Yu HP. Recipient Age and Mortality Risk after Liver Transplantation: A Population-Based Cohort Study. PLoS One. 2016;11:e0152324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Michard B, Artzner T, Lebas B, Besch C, Guillot M, Faitot F, Lefebvre F, Bachellier P, Castelain V, Maestraggi Q, Schneider F. Liver transplantation in critically ill patients: Preoperative predictive factors of post-transplant mortality to avoid futility. Clin Transplant. 2017;31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Petrowsky H, Rana A, Kaldas FM, Sharma A, Hong JC, Agopian VG, Durazo F, Honda H, Gornbein J, Wu V, Farmer DG, Hiatt JR, Busuttil RW. Liver transplantation in highest acuity recipients: identifying factors to avoid futility. Ann Surg. 2014;259:1186-1194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 151] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 11. | Sonny A, Kelly D, Hammel JP, Albeldawi M, Zein N, Cywinski JB. Predictors of poor outcome among older liver transplant recipients. Clin Transplant. 2015;29:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Aloia TA, Knight R, Gaber AO, Ghobrial RM, Goss JA. Analysis of liver transplant outcomes for United Network for Organ Sharing recipients 60 years old or older identifies multiple model for end-stage liver disease-independent prognostic factors. Liver Transpl. 2010;16:950-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Ruíz-del-Árbol L, Achécar L, Serradilla R, Rodríguez-Gandía MÁ, Rivero M, Garrido E, Natcher JJ. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology. 2013;58:1732-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 14. | Zardi EM, Zardi DM, Chin D, Sonnino C, Dobrina A, Abbate A. Cirrhotic cardiomyopathy in the pre- and post-liver transplantation phase. J Cardiol. 2016;67:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Obokata M, Reddy YNV, Borlaug BA. Diastolic Dysfunction and Heart Failure With Preserved Ejection Fraction: Understanding Mechanisms by Using Noninvasive Methods. JACC Cardiovasc Imaging. 2020;13:245-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 174] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 16. | De Nardi M, French E, Jones JB, McCauley J. Medical Spending of the US Elderly. Fisc Stud. 2016;37:717-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |