Copyright
©The Author(s) 2025.
World J Rheumatol. Feb 18, 2025; 12(2): 103837
Published online Feb 18, 2025. doi: 10.5499/wjr.v12.i2.103837
Published online Feb 18, 2025. doi: 10.5499/wjr.v12.i2.103837
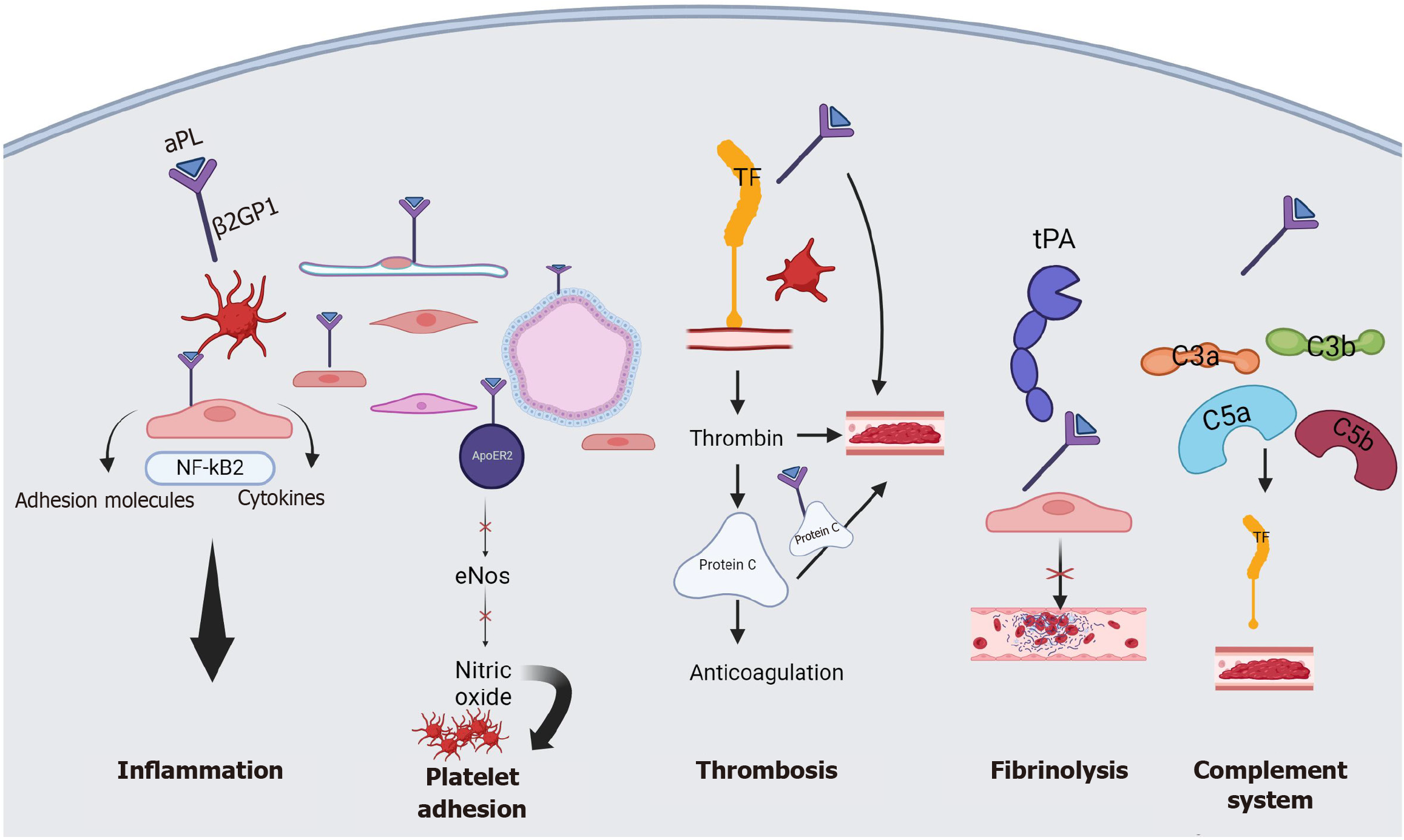
Figure 1 Pathogenesis of antiphospholipid syndrome.
Antiphospholipid antibodies (aPL) impact various components of the hemostatic system. The aPL interacts with β2-glycoprotein-1 antibodies (β2GP1) on the surface of endothelial cells, platelets, and trophoblasts. Nuclear factor kappa B is activated, along with the production of cytokines and adhesion molecules that further inflammation. The aPL also interacts with apolipoprotein E2 receptor to reduce nitric oxide production encouraging platelet adhesion. Anti-β2GP1 antibodies trigger production of tissue factor (TF) but reduces the production of protein C to increase the risk of thrombosis. The aPL prevents the binding of tissue plasminogen activator to its receptor on endothelial cells contributing to hypofunction of the fibrinolytic system. Increased complement activation by aPL increases the risk of thrombosis by increasing TF production and leading to thrombosis. APL: Antiphospholipid antibodies; ApoER2: Apolipoprotein E2 receptor; ENos: Endothelial nitric oxide synthase; NF-κB: Nuclear factor kappa B; TF: Tissue factor; TPA: Tissue plasminogen activator; β2GP1: β2-glycoprotein-1.
- Citation: Akankwasa P, Kakooza J, Katongole J, Namutosi E, Lewis C, Okurut E. Antiphospholipid syndrome in pregnancy: A comprehensive review. World J Rheumatol 2025; 12(2): 103837
- URL: https://www.wjgnet.com/2220-3214/full/v12/i2/103837.htm
- DOI: https://dx.doi.org/10.5499/wjr.v12.i2.103837