Published online Feb 19, 2025. doi: 10.5498/wjp.v15.i2.99573
Revised: November 29, 2024
Accepted: December 19, 2024
Published online: February 19, 2025
Processing time: 75 Days and 0.3 Hours
Abdominal postoperative patients are susceptible to postoperative depression resulting from pain and stress, which can hinder their rehabilitation. Acupuncture has shown potential to relieve this condition.
To analyze the mechanism by which acupuncture relieves postoperative depre
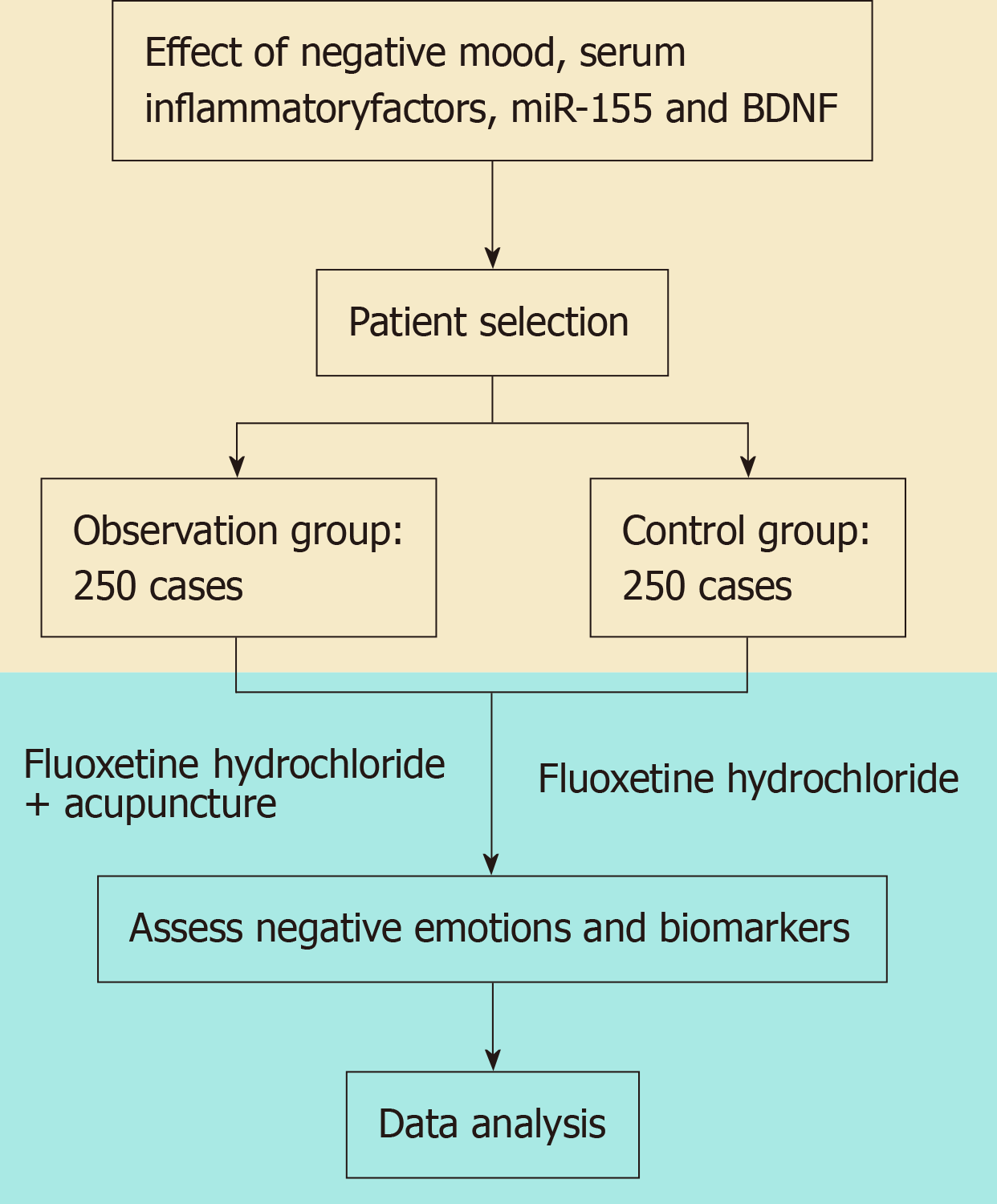
Abdominal postoperative patients with depression between January 2015 and December 2023 at the First Affiliated Hospital of Heilongjiang University of Chinese Medicine were enrolled. Patients were divided into two groups using the random throwing method: Observation (250 cases, fluoxetine hydrochloride + acupuncture treatment) and control (250 cases, fluoxetine hydrochloride trea
Significant improvements were observed in the observation group compared to the control group in all assessed parameters after six weeks (P < 0.05). This suggests that the combination of fluoxetine hydrochloride and acupuncture may be more effective in managing postoperative depression than medication alone.
Acupuncture complies with the principle of traditional Chinese medicine syndrome differentiation and ensures the pertinence and effectiveness of treatment. In addition, it not only actively improves depressive symptoms but also effectively regulates the serum level of inflammatory factors.
Core Tip: Syndrome differentiation acupuncture helps to reduce negative mood disorders, inhibit the inflammatory response, downregulate the expression of miR-155, enhance BDNF levels, and promote the rehabilitation process of patients with postoperative depression.
- Citation: Zhang Q, Zhao Y, Cheng GY. Effect of negative mood, serum inflammatory factors, miR-155, and brain-derived neurotrophic factor. World J Psychiatry 2025; 15(2): 99573
- URL: https://www.wjgnet.com/2220-3206/full/v15/i2/99573.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i2.99573
Abdominal surgery can be a traumatic event. Under the influence of surgical stress and anesthesia, postoperative patients have been known to exhibit notable negative psychoemotional symptoms, including those associated with postoperative depression. Fluoxetine hydrochloride is a selective serotonin reuptake inhibitor, which mainly exerts an antidepressant effect by inhibiting the reuptake of serotonin by neurons. It is often used in the treatment of depression. However, in clinical practice, it has been found to aggravate depressive symptoms in some patients[1]. In recent years, with growing support for traditional Chinese medicine (TCM), the application of TCM in clinical practice has become established. As a green TCM therapy, acupuncture dialectically treats the symptoms of patients. It can dredge the meridians, balance qi and blood, regulate Yin and Yang, and relieve symptoms[2]. However, at present, clinical research on the application of syndrome differentiation acupuncture treatment in patients with postoperative abdominal depression is scarce. To address this, in this study, the therapeutic effect of syndrome differentiation acupuncture treatment in abdominal postoperative patients was evaluated and the corresponding underlying mechanism was elucidated.
Five hundred patients admitted to the Treatment Center of the First Affiliated Hospital of Heilongjiang University of TCM after abdominal surgery between January 2015 and December 2023 were enrolled. The patients were divided into two groups random throwing method: An observation group and a control group. The observation group was comprised of 139 male patients (n = 250) and 111 female patients aged between 42 and 75 years (average age: 58.59 ± 5.54), among which 39 were illiterate and 113 had an educational attainment level below high school. The control group was comprised of 142 male patients (n = 250) and 108 female patients with ages between 45 and 73 years (average age: 59.07 ± 4.73), among which 42 were illiterate and 117 had an educational attainment of high school and above. Neither of the two groups was significantly different (P > 0.05).
The inclusion criteria were as follows: (1) Patients who underwent abdominal surgery and met the indications for surgical treatment; (2) Patients who completed a comprehensive clinical assessment[3]; (3) Patients who had not taken antidepressive drugs or other antipsychotics; and (4) Patients who provided informed consent. The exclusion criteria included: (1) Patients who had allergic reactions or showed intolerance to the materials used in the study; (2) Patients who had mental disorders before enrollment; (3) Patients with a history of alcohol and drug dependence; and (4) Patients who refused to participate or were participating in other studies.
Patients in the observation group were treated with acupuncture treatment. At present, there is a need to standardize the process of acupuncture treatment, including the steps of patient preparation, acupoint positioning, needle preparation, injection feeding, needle running, needle retention, and needle exit. Detailed operational criteria should be in place for each step to ensure the consistency and safety of treatment. Various goals can be achieved through the combination of different operation methods, including lifting and twisting. At the same time, different intensities should be applied based on the sensitivity of the patient (Figure 1).
The control group was administered fluoxetine hydrochloride: Fluoxetine hydrochloride capsules (20 mg) (HJ20160501; Lilly Suzhou Pharmaceutical Co. Ltd., France), once daily or 6 weeks. The observation group was administered syndrome differentiation acupuncture treatment: Mainly ditch, Baihui, Yintang, neiguan, Shenmen, Taichong, and Taichong, liver depression and qi deficiency, liver depression and kidney deficiency, and kidney Yu and three Yin. The acupuncture needle was kept for 30 minutes once daily, with a routine of 5 days of continuous treatment followed by 2 days of rest for 6 weeks.
Negative mood: Systems of negative mood disorders were assessed by the Hamilton Depression Scale 24 items (HAMD-24)[4]. The scale consists of seven categories (24 items), including somatization (6 items, 0-18 points), weight change (1 item, 0-2 points), cognitive impairment (6 items, 0-22 points), day/night change (1 item, 0-2 points), delay (4 items, 0-14 points), sleep disturbance (3 items, 0-6 points), and despair (3 items, 0-12 points). There were two evaluation time nodes: Pre-intervention and 6 weeks post-intervention.
Serum inflammatory factor level: Fasting elbow venous blood (3 mL) was collected by centrifugation at 2500 r/min for 10 minutes (no. 1411797; Eppendorf AG, National Drug Administration). The resulting supernatant was used to determine tumor necrosis factor α (TNF-α), serum interleukin (IL)-1β, and IL-6 by enzyme-linked immunosorbent testing. Detection was performed at the pre-intervention stage and 6 weeks post-intervention.
miR-155 expression level: In the fasting state, 1 mL of venous blood was collected. Then, RNA was extracted using an RNA extraction reagent and detected by real-time PCR. Detection was performed at the two aforementioned time nodes (pre-intervention and 6 weeks post-intervention).
BDNF level: Peripheral venous blood samples were collected after fasting (1 mL), placed in an anticoagulant tube, and centrifuged. The resulting supernatant was tested by enzyme-linked immunosorbent test. The levels were detected at the two aforementioned time nodes (pre-intervention and 6 weeks post-intervention).
The results were analyzed in SPSS (27.0). Count data performance was represented as a percentage (%) using the χ2 test. P < 0.05 was considered statistically significant.
Before intervention, the seven items in the HAMD-24 score were relatively balanced, with no statistically significant differences (P > 0.05). After 6 weeks of intervention, the differences between the above seven items were statistically significant (P < 0.05) (Table 1).
| Group | n | Somatization | Body weight change | Cognitive disorder | Diurnal fluctuation diurnal variation | Sluggish | Sleep disorder | Feeling of despair | |||||||
| Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | ||
| Control | 250 | 14.18 ± 2.46 | 11.39 ± 2.24a | 1.29 ± 0.35 | 0.84 ± 0.28a | 17.57 ± 2.42 | 13.15 ± 2.21a | 1.32 ± 0.27 | 0.71 ± 0.16a | 10.12 ± 2.27 | 7.37 ± 2.19a | 4.25 ± 0.82 | 2.03 ± 0.74a | 8.15 ± 2.09 | 5.13 ± 1.27a |
| Observation | 250 | 14.23 ± 2.30 | 10.87 ± 2.13a | 1.31 ± 0.28 | 0.79 ± 0.12a | 17.49 ± 2.36 | 12.61 ± 2.15a | 1.29 ± 0.31 | 0.68 ± 0.09a | 10.25 ± 2.30 | 6.89 ± 2.06a | 4.33 ± 0.76 | 1.87 ± 0.50a | 8.28 ± 2.14 | 4.85 ± 1.06a |
| t | 0.235 | 2.660 | 0.706 | 2.595 | 0.374 | 2.769 | 1.154 | 2.584 | 0.636 | 2.524 | 1.131 | 2.833 | 0.687 | 2.676 | |
| P value | 0.815 | 0.008 | 0.481 | 0.010 | 0.708 | 0.006 | 0.249 | 0.010 | 0.525 | 0.012 | 0.258 | 0.005 | 0.492 | 0.008 | |
Before intervention, the serum inflammatory factors levels between groups were also relatively well-balanced and showed no statistically significant differences (P > 0.05). After 6 weeks, significantly different levels were observed (P < 0.05) (Table 2).
Before intervention, the miR-155 expression levels were well-balanced with no significant differences (P > 0.05). After 6 weeks, significant differences were observed in the miR-155 expression levels between the groups (P < 0.05) (Table 3).
| Group | n | miR-155 | |||
| Before | After | t | P value | ||
| Control | 250 | 5.89 ± 0.52 | 4.02 ± 0.35 | 47.171 | < 0.001 |
| Observation | 250 | 5.91 ± 0.48 | 3.95 ± 0.21 | 59.150 | < 0.001 |
| t | 0.447 | 2.712 | |||
| P value | 0.655 | 0.007 | |||
Before intervention, the BDNF levels were also relatively well-balanced (P > 0.05). After 6 weeks, the BDNF levels between the groups were statistically significant (P < 0.05) (Table 4).
| Group | n | Before | After | t | P value |
| Control | 250 | 15.46 ± 1.03 | 20.80 ± 1.24 | 52.378 | < 0.001 |
| Observation | 250 | 15.54 ± 1.10 | 21.09 ± 1.30 | 51.530 | < 0.001 |
| t | 0.839 | 2.552 | |||
| P value | 0.402 | 0.011 |
From the perspective of modern medicine, potential reasons for depression arising in abdominal postoperative patients include: (1) Abdominal surgery itself is a psychological stressor, which can promote the increase of catecholamine levels in patients, leading to endogenous depression; (2) Under the influence of their own diseases, patients need to bear the pain caused by disease, making their mood change, thus causing or aggravating negative emotions, such as depression; and (3) A lack of understanding regarding their condition and its treatment may lead to feelings of fear, which can increase the risk of postoperative depression. Although treatment with fluoxetine hydrochloride has shown good results at relieving the symptoms of depression, long-term use of this medication can result in drug resistance, as well as potentially aggravating the condition. This leads patients to lose confidence in treatment and reduce medication compliance[5].
From the perspective of the TCM, abdominal postoperative depression belongs to the category of “depression syndrome”. Its pathogenesis is: (1) Caused by viscera dysfunction, resulting in human qi, blood, and fluid stasis; (2) Emotional and qi disorder; and (3) Emotional injury and viscera dysfunction by internal causes. Dialectical acupuncture treatment avoids creating a dependence on oral antidepressants, which can not only guarantee the safety of treatment, but also ensure the effectiveness of treatment.
The HAMD-24 score was found to be low in the treated patients after 6 weeks compared with the control group (P < 0.05). This suggests that dialectical acupuncture treatment relieved qi and the liver and promoted qi and blood circulation, replenished blood activation and replenish. For liver depression and kidney deficiency, treatment relieved the liver and qi. To achieve the best therapeutic effects, acupuncture needs to be personalized, respecting the individual differences of each patient. At the same time, a standardized protocol is needed to ensure the efficacy of dialectical acupuncture, as indicated by Yang et al[6].
Depression is often accompanied by a degree of inflammatory reaction. After 6 weeks of intervention, lower TNF-α, IL-1β, and IL-6 levels (P < 0.05) were observed in the observation group. TNF-α is an inflammatory factor that can cross the blood-brain barrier and activate glial cells, which may play a role in promoting the development of depressive symptoms[7]. IL-1β leads to dysfunction of serotonin metabolism in the brain, which can result in depression[8]. IL-6 can induce apoptosis of neuronal cells, affecting the transmission of neurotransmitters[9]. Overall, the expression levels of miR-155 in the observation group were reduced compared with the control group (P < 0.05). miR-155 mat play a role in the mechanism of immune dysfunction in patients with depression by regulating the expression of cytokines[10]. Fur
Acupuncture targets acupoints and pain points that belong to the meridians and related veins regulatory role via physical stimulation, in line with the holistic approach of TCM treatments. In doing so, it seeks to reduce the inflammatory response and restore balance in the immune response. Although this study provided insights into the clinical therapeutic effects of acupuncture in patients undergoing abdominal surgery, this study still has some limitations. Attempts were made to explain the mechanisms by which acupuncture treatment improves depressive symptoms and regulates related indicators; however, sufficient experimental evidence is lacking. For example, in explaining the mechanism by which acupuncture regulates the serum levels of inflammatory factors, only the correlation between inflammatory factors and depression was mentioned, and the specific signaling pathways by which acupuncture affects inflammatory factor expression are not known.
In summary, acupuncture treatment in patients with postoperative abdominal depression was found to be effective in relieving the symptoms of this negative mood disorder. This therapeutic approach conforms to the social-psychological-biomedical model of modern medicine, actively improving the negative emotions of patients. These findings suggest that this approach is worthy of clinical application.
| 1. | Shen D, Zhao H, Gao S, Li Y, Cheng Q, Bi C, Zhou Z, Li Y, Yu C. Clinical serum metabolomics study on fluoxetine hydrochloride for depression. Neurosci Lett. 2021;746:135585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Li M, Niu J, Yan P, Yao L, He W, Wang M, Li H, Cao L, Li X, Shi X, Liu X, Yang K. The effectiveness and safety of acupuncture for depression: An overview of meta-analyses. Complement Ther Med. 2020;50:102202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | McAllister-Williams RH. NICE guidelines for the management of depression. Br J Hosp Med (Lond). 2006;67:60-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Zimmerman M, Martinez JH, Young D, Chelminski I, Dalrymple K. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord. 2013;150:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 799] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 5. | Szoke-Kovacs Z, More C, Szoke-Kovacs R, Mathe E, Frecska E. Selective Inhibition of the Serotonin Transporter in the Treatment of Depression: Sertraline, Fluoxetine and Citalopram. Neuropsychopharmacol Hung. 2020;22:4-15. [PubMed] |
| 6. | Yang NN, Lin LL, Li YJ, Li HP, Cao Y, Tan CX, Hao XW, Ma SM, Wang L, Liu CZ. Potential Mechanisms and Clinical Effectiveness of Acupuncture in Depression. Curr Neuropharmacol. 2022;20:738-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 69] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 7. | Yao L, Pan L, Qian M, Sun W, Gu C, Chen L, Tang X, Hu Y, Xu L, Wei Y, Hui L, Liu X, Wang J, Zhang T. Tumor Necrosis Factor-α Variations in Patients With Major Depressive Disorder Before and After Antidepressant Treatment. Front Psychiatry. 2020;11:518837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Sardar M, Zia K, Ashraf S, Malik HN, Jabeen A, Khan KM, Ul-Haq Z. Interface inhibitory action on Interleukin-1β using selected anti-inflammatory compounds to mitigate the depression: A computational investigation. Comput Biol Chem. 2022;101:107774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Kelly KM, Smith JA, Mezuk B. Depression and interleukin-6 signaling: A Mendelian Randomization study. Brain Behav Immun. 2021;95:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 10. | Dai J, Pan JY, Liao N, Shi J, Zeng Q, Huang L, Chen LP. Influence of miR-155 on behaviors of depression mice through regulating Wnt/β-catenin signaling pathway. Eur Rev Med Pharmacol Sci. 2020;24:1398-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 11. | Colucci-D'Amato L, Speranza L, Volpicelli F. Neurotrophic Factor BDNF, Physiological Functions and Therapeutic Potential in Depression, Neurodegeneration and Brain Cancer. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 401] [Cited by in RCA: 534] [Article Influence: 106.8] [Reference Citation Analysis (0)] |