Published online Jun 19, 2024. doi: 10.5498/wjp.v14.i6.894
Revised: May 13, 2024
Accepted: May 24, 2024
Published online: June 19, 2024
Processing time: 99 Days and 4.4 Hours
Postoperative pain management and cognitive function preservation are crucial for patients undergoing thoracoscopic surgery for lung cancer (LC). This is achieved using either a thoracic paravertebral block (TPVB) or sufentanil (SUF)-based multimodal analgesia. However, the efficacy and impact of their combined use on postoperative pain and postoperative cognitive dysfunction (POCD) remain unclear.
To explore the analgesic effect and the influence on POCD of TPVB combined with SUF-based multimodal analgesia in patients undergoing thoracoscopic radical resection for LC to help optimize postoperative pain management and improve patient outcomes.
This retrospective analysis included 107 patients undergoing thoracoscopic radical resection for LC at The Affiliated Cancer Hospital of Zhengzhou Univer
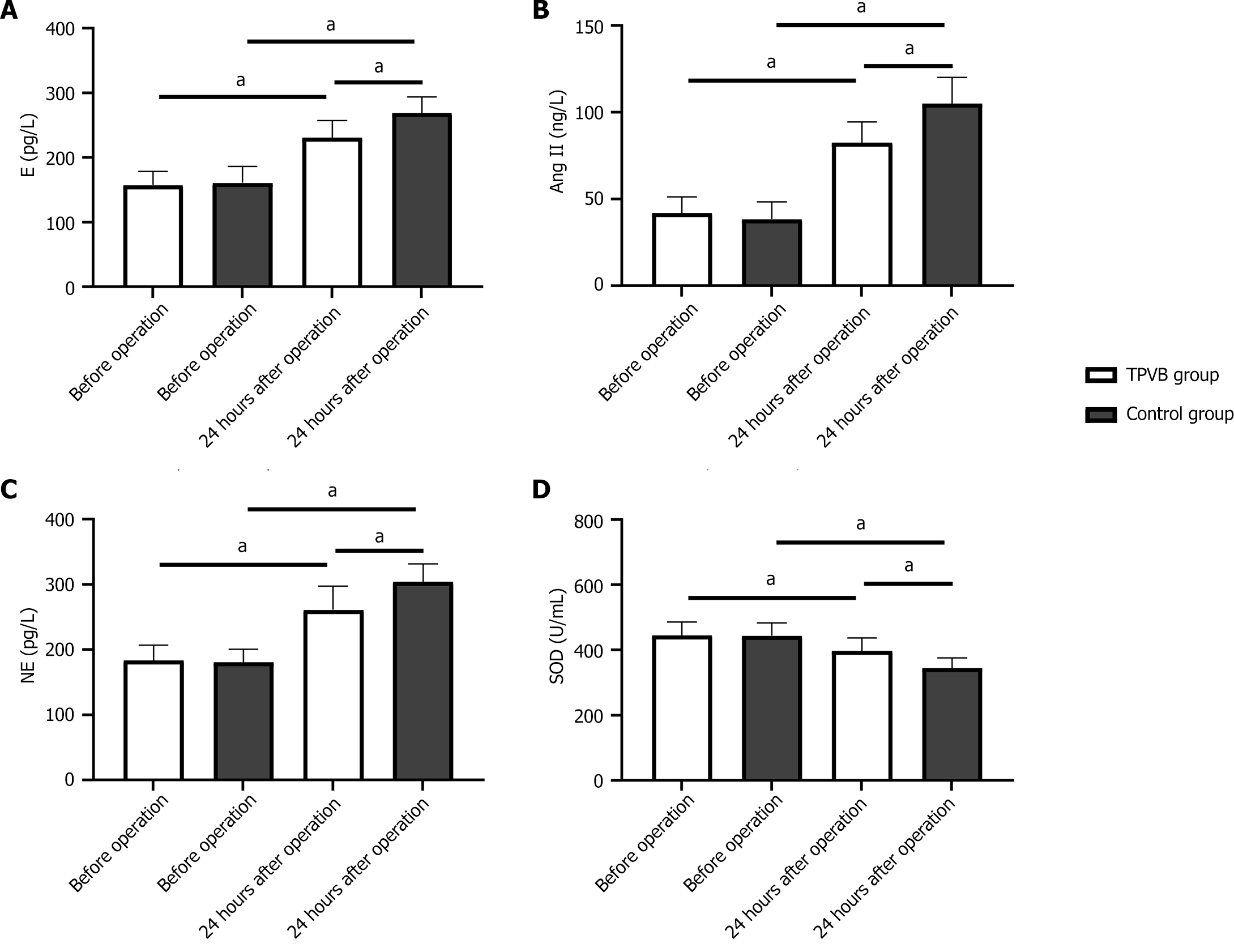
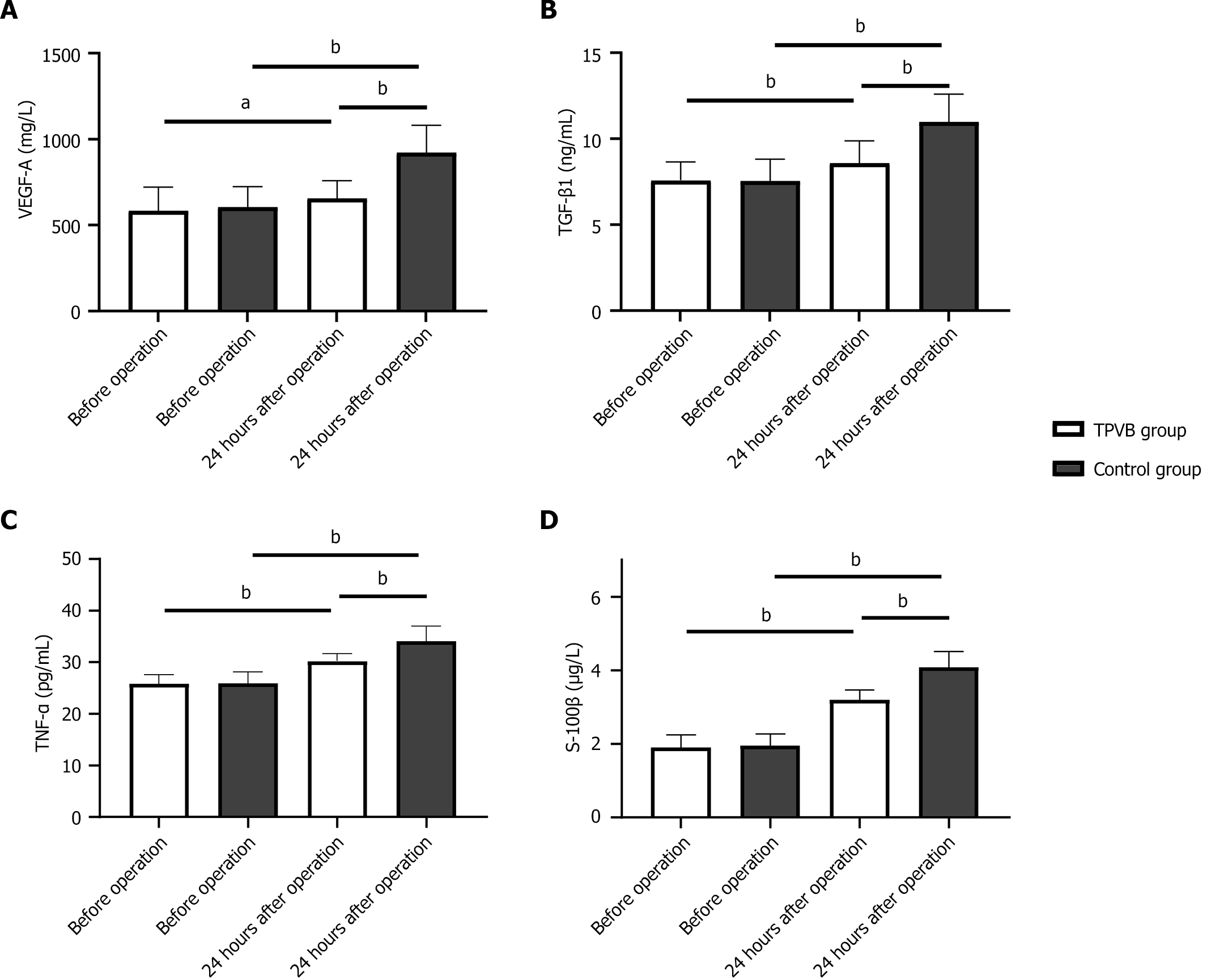
There were no significant time point, between-group, and interaction effects in Ramsay sedation scores between the two groups (P > 0.05). Significantly, there were notable time point effects, between-group differences, and interaction effects observed in VAS scores both at rest and with cough (P < 0.05). The VAS scores at rest and with cough at 12 and 24 h after surgery were lower than those at 2 h after surgery and gradually decreased as postoperative time increased (P < 0.05). The TPVB group had lower VAS scores than the control group at 2, 12, and 24 h after surgery (P < 0.05). The MMSE scores at postoperative days 1 and 3 were markedly higher in the TPVB group than in the control group (P < 0.05). The incidence of POCD was significantly lower in the TPVB group than in the control group within 5 days after surgery (P < 0.05). Both groups had elevated serum E, Ang II, and NE and decreased serum SOD levels at 24 h after surgery compared with the preoperative levels, with better indices in the TPVB group (P < 0.05). Marked elevations in serum levels of VEGF, TGF-β1, TNF-α, and S-100β were observed in both groups at 24 h after surgery, with lower levels in the TPVB group than in the control group (P < 0.05).
TPVB combined with SUF-based multimodal analgesia further relieves pain in patients undergoing thoracoscopic radical surgery for LC, enhances analgesic effects, reduces postoperative stress response, and inhibits postoperative increases in serum VEGF, TGF-β1, TNF-α, and S-100β levels. This scheme also reduced POCD and had a high safety profile.
Core Tip: This study demonstrates that the combination of thoracic paravertebral block with sufentanil-based multimodal analgesia in patients undergoing thoracoscopic surgery for lung cancer (LC) enhances analgesia and reduces the rate of postoperative cognitive dysfunction. Besides decreasing postsurgical stress responses and various serum biomarker levels, this combination scheme exhibits higher safety, potentially providing a more effective strategy for pain management and cognitive function preservation. Our findings pave the way for new standards in postoperative care for LC surgery.
- Citation: Wang DD, Wang HY, Zhu Y, Lu XH. Impact of thoracic paravertebral block and sufentanil on outcomes and postoperative cognitive dysfunction in thoracoscopic lung cancer surgery. World J Psychiatry 2024; 14(6): 894-903
- URL: https://www.wjgnet.com/2220-3206/full/v14/i6/894.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i6.894
The incidence of malignancies in China accounts for approximately 21.8% of cases worldwide[1]. Among all malignant tumor types, lung cancer (LC) ranks first in men and second in women, with a standardized mortality rate of 39.81 per 100000 population, which is the highest among all cancer types[2]. Although there are various treatment strategies for LC, surgery is considered the key approach and has been the preferred strategy in clinical practice in recent years. This is mainly due to rapid developments in minimally invasive thoracoscopic technology and its widespread clinical use[3]. Compared with traditional thoracotomy, minimally invasive thoracoscopic surgery involves smaller incisions and results in less trauma, milder pain, and faster postoperative recovery.
Patients undergoing thoracoscopic radical resection for LC usually receive a single general anesthesia that requires large doses of analgesic and sedative drugs and may greatly impact the cardiovascular and immune systems as well as postoperative cognitive function in older adults[4]. However, single general anesthesia cannot completely block the pain stimulation from the surgical area, potentially leading to an excessive stress reaction and an increased risk of postoperative complications and tumor recurrence and metastasis. Furthermore, although thoracoscopic surgery is minimally invasive, it still affects respiratory and circulatory function, thus affecting postoperative recovery[5]. Some patients are afraid to cough after surgery due to concerns about pain, resulting in delayed sputum discharge and reduced effective breathing times, leading to lung infection and atelectasis[6]. Therefore, the determination of an ideal analgesic method that relieves postoperative pain and reduces the rate of complications is crucial. Sufentanil (SUF)-based multimodal analgesia has a good analgesic effect, rapid onset, and little influence on cardiovascular function, making it a relatively ideal analgesic[7,8]. However, the analgesic effect may also be influenced by the number of drainage tubes, incision length, and other factors, resulting in unstable pain relief[9]. The single administration of a thoracic paravertebral block (TPVB) has been reported to relieve pain in intercostal incisions by blocking multiple intercostal nerves[10].
The effect of TPVB combined with SUF analgesia on patients undergoing thoracoscopic radical surgery for LC and its influence on postoperative cognitive dysfunction (POCD) is rarely reported, and the effect of this scheme on post-operative pain and cognitive dysfunction requires clarification. Therefore, the purpose of this study was to analyze the effects of TPVB combined with SUF-based multimodal analgesia on the analgesic effect and postoperative cognitive function of patients undergoing thoracoscopic radical surgery for LC to provide potential solutions for clinical treatment.
We retrospectively analyzed data on 107 patients who underwent thoracoscopic radical surgery for LC in The Affiliated Cancer Hospital of Zhengzhou University and Henan Cancer Hospital from May 2021 to January 2023. Patients were grouped into a TPVB group (n = 57) and a control group (n = 50) according to the different anesthesia schemes.
Patients aged ≥ 18 years diagnosed with LC who met the criteria for thoracoscopic radical resection and received surgical treatment, with normal preoperative coagulation function test results, American Society of Anesthesiologists physical status[11] grade I or II, clear consciousness, normal communication skills, and no distant metastasis were included in the study population.
Patients with the inability to communicate normally and cooperate with the research process due to language comprehension disorders and mental illness and those with severe cardiocerebrovascular diseases, history of preoperative radiotherapy and chemotherapy, history of other surgeries, deformity of the spine or thorax, and diseases of the immune system or central nervous system were excluded from the study population.
Patients in both groups underwent routine preoperative medical examinations, including routine blood, coagulation function, and urine tests, as well as an electrocardiogram. General anesthesia was administered prior to surgery using the following anesthetic drugs: midazolam (0.3 mg; Yichang Humanwell Pharmaceutical Co., Ltd.), SUF (0.3 μg/kg; Jiangsu Nhwa Pharmaceutical Co., Ltd.), etomidate (0.3 mg/kg; Jiangsu Enhua), and cisatracurium (0.25 mg/kg; Zhejiang Xianju Pharmaceutical Co., Ltd.). Routine endotracheal intubation and mechanical ventilation were performed, with sevoflurane (0.8–1.5 MAC; Fujian Highsea United Pharmaceutical Co., Ltd.), propofol (2.6-3.2 μg/kg; Beijing Sciecure Pharmaceutical Co., Ltd.), and remifentanil (0.3 μg/kg/min; Jiangsu Nhwa Pharmaceutical Co., Ltd.) used to maintain anesthesia. Cisatracurium (0.1 mg/kg) was administered intermittently, depending on the patient’s condition. The patient’s vital signs were closely monitored during the operation, and the drug dosage was adjusted accordingly. For the control group, SUF-based multimodal analgesia was administered after surgery, and patient-controlled intravenous analgesia was connected, where 100 μg SUF and 5 mg tropisetron (Shandong Luoxin Pharmaceutical Group Stock Co., Ltd.) were diluted with 100 mL normal saline for pumping. The TPVB group received a TPVB and SUF-based multimodal analgesia, with the latter being the same as that of the control group. For the TPVB, the patient was placed on their side before anesthesia, and a puncture point was selected in the T4-T7 paraspinal space on the operating side. The paravertebral nerve block was then performed with an atraumatic needle for peripheral nerve blocks under ultrasound guidance. When the needle reached below the transverse process, 0.5% ropivacaine (15 mL; Chengdu Baiyu Pharmaceutical Co., Ltd.) was injected, and the absence of cerebrospinal fluid, blood, and air was confirmed.
Clinical data and laboratory test results were collected from patients’ electronic medical records and surgical records, respectively. The clinical data included age, sex, pathological stage, pathological type, operation time, intraoperative blood loss, and history of diabetes and hypertension. The laboratory indices included epinephrine (E), norepinephrine (NE), angiotensin II (Ang Ⅱ), superoxide dismutase (SOD), vascular endothelial growth factor (VEGF), transforming growth factor-β1 (TGF-β1), tumor necrosis factor-α (TNF-α), and S-100 calcium-binding protein β (S-100β). The functional scores used included the Mini-Mental State Examination (MMSE)[12], the Ramsay Sedation Scale[13], and the visual analog scale (VAS)[14].
Before and 24 h after surgery, 5 mL of cubital venous blood was collected from all patients and centrifuged at 3000 rpm for 10 min. The resultant serum was stored at -70°C for later testing. E and NE were determined using radioimmunoassay (Shanghai Xinfan Biotechnology Co., Ltd.), Ang Ⅱ using chemiluminescence assay (Shenzhen Snibe Biomedical Engineering Co., Ltd.), and SOD, VEGF, TGF-β1, TNF-α, and S-100β using enzyme-linked immunosorbent assay (Hangzhou Haoxin Biotechnology Co., Ltd.).
Cognitive function was assessed using the MMSE (scale: 0-30). A score of 2 points lower than that on the day before surgery was considered an indicator of POCD. The Ramsay sedation score was determined as follows: anxious and restless, 1 point; tranquil and cooperative, 2 points; somnolent with prompt response to instructions, 3 points; light sleep with quick response to arousal, 4 points; sleeping with slow response to arousal, 5 points; and deep sleep with no response to arousal, 6 points. A score of 1, 2-4, and ≥ 5 indicated insufficient sedation, good sedation, and excessive se-dation, respectively. Pain was assessed using the VAS. The score ranges from 0 to 10 and is directly proportional to the pain level.
The primary outcome measures were differences in MMSE scores before surgery and 3 and 5 days after surgery, as well as differences in Ramsay Sedation Scale and VAS scores at 2, 12, and 24 h after surgery.
The secondary outcome measures included changes in VEGF, TGF-β1, TNF-α, S-100β, and stress function indices between the two groups before and after treatment. The number of adverse reactions was also reported.
All analyses were performed using SPSS v19 statistical software. P values < 0.05 were considered statistically significant. Quantitative data were expressed as mean ± SD. Paired t-test and independent sample t-test were used for intragroup and intergroup comparisons, respectively. analysis using Bonferroni test. Continuous data were expressed as numbers and rates Multiple time point comparisons were conducted using repeated measures ANOVA, and post hoc (%). χ2 tests were performed for categorical data.
There were no statistically significant differences in age, sex, pathological stage, pathological type, operation time, intraoperative blood loss, diabetes history, and hypertension history between the control and TPVB groups (P > 0.05; Table 1).
| Factors | TPVB group (n = 57) | Control group (n = 50) | χ2/t test | P value | |
| Age | 0.633 | 0.426 | |||
| ≥ 60 years | 31 | 31 | |||
| < 60 years | 26 | 19 | |||
| Sex | 0.342 | 0.558 | |||
| Male | 31 | 30 | |||
| Female | 26 | 20 | |||
| Pathological stage | 1.219 | 0.543 | |||
| I | 17 | 20 | |||
| II | 28 | 21 | |||
| III | 12 | 9 | |||
| Pathological type | 0.587 | 0.443 | |||
| Squamous cell carcinoma | 27 | 20 | |||
| Adenocarcinoma | 30 | 30 | |||
| Operation time | 147.35 ± 15.70 | 148.44 ± 13.30 | 0.384 | 0.701 | |
| Intraoperative blood loss (mL) | 141.05 ± 54.49 | 131.14 ± 53.54 | 0.946 | 0.346 | |
| History of diabetes | 0.679 | 0.409 | |||
| Yes | 10 | 12 | |||
| No | 47 | 38 | |||
| History of hypertension | 1.153 | 0.282 | |||
| Yes | 14 | 17 | |||
| No | 43 | 33 |
There was no statistically significant difference in the pretreatment MMSE scores between groups (P > 0.05). The MMSE scores of both groups were significantly lower on postoperative day 3 than on the day before surgery (P < 0.05), with significantly higher MMSE scores in the TPVB group compared with the control group (P < 0.001). The MMSE score was higher in the TPVB group than in the control group (P < 0.05) on postoperative day 5. MMSE scores in both groups were significantly higher on postoperative day 5 than on postoperative day 3 (P < 0.05). However, there was no difference in the MMSE scores on postoperative day 5 compared with the day before surgery in the TPVB group (P > 0.05), while MMSE scores on postoperative day 5 were significantly decreased compared with the day before surgery in the control group with (P < 0.05; Table 2). Seven patients in the TPVB group and 15 patients in the control group developed POCD within 5 days after surgery, suggesting a lower probability of POCD in the TPVB group compared with the control group (P < 0.05).
A comparison of the Ramsay scores at each time point revealed no statistical difference between the two groups (P > 0.05; Table 3).
| Grouping | 2 h after surgery | 12 h after surgery | 24 h after surgery |
| TPVB group (n = 57) | 2.91 ± 0.93 | 2.91 ± 0.74 | 2.70 ± 0.50 |
| Control group (n = 50) | 2.62 ± 0.64 | 2.66 ± 0.69 | 2.62 ± 0.49 |
| t value | 2.241 | 1.946 | 0.686 |
| P value | 0.388 | 0.791 | 0.945 |
A comparison of pre- and posttreatment VAS scores did not reveal any statistically significant intergroup differences at 2 h after surgery (P > 0.05). In both groups, the VAS scores decreased significantly at 12 h after surgery compared with 2 h after surgery (P < 0.05), with higher VAS scores in the TPVB group vs the control group (P < 0.05). At 24 h after surgery, the VAS score in the TPVB group was significantly lower than in the control group (P < 0.05). In both groups, the VAS score at 24 h after surgery was significantly lower than that at 12 h (P < 0.05) and at 2 h (P < 0.001) after surgery (Table 4).
We compared stress function indices of the two groups before and after treatment. There was no significant difference in preoperative levels of E, Ang II, NE, and SOD between the two groups (P > 0.05). In both groups, the levels of E, Ang II, and NE were significantly elevated at 24 h after surgery compared with their preoperative levels (P < 0.0001), while that of SOD decreased significantly (P < 0.0001). Moreover, the TPVB group had lower E, Ang II, and NE levels and higher SOD levels than the control group at 24 h after surgery (P < 0.0001; Figure 1).
We compared the pre- and posttreatment levels of VEGF, TGF-β1, TNF-α, and S-100β. The preoperative levels were similar between groups (P > 0.05). The levels of VEGF, TGF-β1, TNF-α, and S-100β were significantly increased in both groups at 24 h after surgery compared with the levels before surgery (P < 0.01). Moreover, the levels of VEGF, TGF-β1, TNF-α, and S-100β were significantly lower in the TPVB group than in the control group at 24 h after surgery (P < 0.0001; Figure 2).
Differences in the occurrence of adverse reactions between the two groups were not statistically significant (P > 0.05; Table 5).
| Grouping | Nausea and vomiting | Hypotension | Delayed recovery from anesthesia | Respiratory depression |
| TPVB group (n = 57) | 2 | 3 | 1 | 0 |
| Control group (n = 50) | 1 | 2 | 1 | 2 |
| χ2 | 0.222 | 0.095 | 0.001 | 2.323 |
| P value | 0.637 | 0.757 | 0.925 | 0.127 |
The prevalence and mortality of LC have continued to rise in recent years, seriously impacting the health and quality of life of those affected[15]. The older adult population has a high risk of LC development. Because they often suffer from multiple chronic diseases and have a relatively low tolerance for surgery and pain, the choice of an appropriate surgical modality is critical[16]. Compared with traditional thoracotomy, thoracoscopic radical resection for LC is less traumatic and has a faster recovery rate and fewer complications, making it the first choice for older adult patients. Although this procedure reduces the major trauma associated with thoracotomy and enables intercostal puncture, intrathoracic manipulation, and thoracic drainage and indwelling, narcotic drugs still trigger a substantial stress response[17]. Such intense stress reactions stimulate the production of a large number of inflammatory factors, which may lead to hemodynamic disturbance and increase the risk of postoperative complications and tumor recurrence and metastasis[18]. Therefore, when choosing perioperative anesthesia, it is necessary to both enhance the analgesic effect and reduce patient stress, inflammation, and postoperative adverse reactions to improve postoperative recovery.
Combination analgesic schemes[19] can achieve a good analgesic effect because a variety of analgesic drugs can be used in combination to complement each other’s mechanism of action during the perioperative period, thereby enhancing the analgesic effect and relieving postoperative pain. The SUF-based multimodal analgesia scheme has been widely used in surgical procedures. Although this scheme allows patients to relieve postoperative pain without the need for supplementary analgesia, there are some drawbacks, such as drug dependence in some patients with limited efficacy[20]. TPVB involves the injection of local anesthetic drugs that act on sympathetic nerves to achieve a local block. There is no obvious effect on hemodynamics, and the occurrence of respiratory depression is reduced[21]. Clinically, TPVB combined with SUF-based multimodal analgesia can be considered to relieve postoperative pain in patients undergoing thoracoscopic surgery for LC, and this may be a new and effective intervention scheme. Our study revealed that the TPVB group had higher MMSE scores on postoperative day 1 and day 3, a lower incidence of POCD, and no significant differences in the incidence of postoperative adverse reactions compared with the control group. Thus, the combined use of TPVB and SUF enhanced the analgesic effect, effectively reduced postoperative cognitive impairment, and lowered the rate of adverse reactions in older adult patients undergoing thoracoscopic surgery for LC, thereby reducing the impact on cognitive function.
The injection of local anesthetic drugs into the thoracic paravertebral space for a TPVB ensures the blocking of multiple ipsilateral somatic segments and sympathetic nerves[22]. Notably, ultrasound-guided block enables direct observation of the block site, thereby improving the puncture success rate and ensuring sufficient block, which shortens the onset time. We found that compared with the control group, the Ramsay sedation score in the TPVB group was almost the same at 2, 12, and 24 h after surgery, but the VAS score was significantly reduced. This suggests that TPVB combined with SUF-based multimodal analgesia not only achieves a good sedative effect but also enhances the analgesic effect. Additionally, ropivacaine, which has a prolonged action time, better local anesthetic effect than lidocaine, low fat solubility, and shorter recovery time of motor nerve block, is also used in TPVB, enabling patients to start bed activities as soon as possible[23]. The use of ropivacaine to perform TPVB combined with general anesthesia has also been shown to cover the sensory nerves at the surgical site more comprehensively to block the pain conduction pathway, thereby alleviating pain[24]. Therefore, in cases where SUF-based multimodal analgesia is ineffective, TPVB can be supplemented to reduce pain more effectively and enhance the analgesic effect[25].
It is well known that surgical injury and anesthesia may cause a stress response that triggers changes in endocrine hormones. Increases in the levels of stress hormones, such as NE and E, indicate increased sympathetic nerve activity, and their entry into the bloodstream may cause vasoconstriction and trigger hemodynamic instability[26]. Ang Ⅱ activates the renin–angiotensin system and induces oxidative stress[27]. SOD exerts antioxidant effects by scavenging oxygen free radicals to reduce oxidative stress[28]. We found that the serum levels of E, Ang Ⅱ, and NE in the two groups increased within 24 h after surgery, and the SOD level decreased, which was mainly due to the stress reaction caused by surgical injury. However, compared with the control group, serum levels of E, Ang Ⅱ, and NE were lower and SOD was higher in the TPVB group, indicating that the treatment scheme used in the TPVB group alleviates the stress reaction. The main reason for this may be that TPVB combined with SUF-based multimodal analgesia further inhibits sympathetic nerve activity, thereby alleviating postoperative pain, promoting wound healing, and relieving postoperative stress.
VEGF and TGF-β1 are key regulators of vascular proliferation that stimulate vascular division and proliferation and promote neovascularization, promoting the widespread distribution and metastasis of cancer cells[29]. The higher the levels of VEGF and TGF-β1, the greater the risk of metastasis in cancer patients. When the body is under stress or in pain, TNF-α stimulates the release of neuroactive substances, which may exacerbate the inflammatory response, further damaging nerve function[30]. S-100β participates in the degradation of the extracellular matrix, and the more serious the inflammatory reaction, the higher its level[31]. Our findings showed that the serum levels of VEGF, TGF-β1, TNF-α, and S-100β were increased in both groups within 24 h after surgery. However, the levels were lower in the TPVB group, suggesting that TPVB combined with SUF-based multimodal analgesia inhibits the formation of new tumor blood vessels after surgery and alleviates inflammation. The rise in VEGF and TGF-β1 Levels may be caused by factors such as surgical procedures and local tissue pressure, which promote cancer cell spread, while the increased levels of TNF-α and S-100β are attributed to surgical injury-induced inflammatory reactions.
Our study confirmed the role of TPVB combined with SUF in preserving cognitive function and relieving pain in patients undergoing thoracoscopic radical resection for LC. However, there are some limitations that require further consideration. First, the sample size was limited due to the retrospective nature of the study. Second, because there was no follow-up, the influence of the two anesthesia schemes on patient prognosis requires further investigation. Therefore, prospective studies with adequate follow-up are necessary to validate our conclusions.
Our findings reveal the promising application of TPVB combined with SUF in thoracoscopic radical resection for LC. The combined scheme has an obvious analgesic effect and effectively reduces POCD risk, stress, and inflammation in older adults. This is highly beneficial for controlling pain, improving postoperative recovery, and reducing postoperative pain-induced stress responses.
| 1. | Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J (Engl). 2021;134:783-791. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1624] [Cited by in RCA: 1797] [Article Influence: 449.3] [Reference Citation Analysis (1)] |
| 2. | Cao M, Li H, Sun D, Chen W. Cancer burden of major cancers in China: A need for sustainable actions. Cancer Commun (Lond). 2020;40:205-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 226] [Cited by in RCA: 308] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 3. | Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Liu Y, Liu J, Zhang M, Qi J, Yu S, Afshin A, Gakidou E, Glenn S, Krish VS, Miller-Petrie MK, Mountjoy-Venning WC, Mullany EC, Redford SB, Liu H, Naghavi M, Hay SI, Murray CJL, Liang X. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145-1158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2594] [Cited by in RCA: 2402] [Article Influence: 400.3] [Reference Citation Analysis (1)] |
| 4. | Xu K, Cai W, Zeng Y, Li J, He J, Cui F, Liu J. Video-assisted thoracoscopic surgery for primary lung cancer resections in patients with moderate to severe chronic obstructive pulmonary diseases. Transl Lung Cancer Res. 2021;10:2603-2613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Geng C, Tong C, Li H, Shi S, Yu J, Huang L. Effects of Thoracic Paravertebral Block on Postoperative Anxiety and Depression for Patients Undergoing Thoracoscopic Lung Cancer Radical Surgery. Comput Math Methods Med. 2022;2022:7629012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Feng M, Wang L, Sun J, Chen Z, Fu J, Liu D, Zhang R, Li Y, Zhang Y, Zhang H, Zhang W, Feng C. Thoracic Paravertebral Block Combined with General Anaesthesia or General Anaesthesia Alone for Thoracoscopic Lung Adenocarcinoma Surgery: A Retrospective Study. Cancer Manag Res. 2022;14:953-965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Vergari A, Di Muro M, De Angelis A, Nestorini R, Meluzio MC, Frassanito L, Tamburrelli FC, Rossi M. Sublingual sufentanil nanotab patient-controlled analgesia system/15 mcg in a multimodal analgesic regimen after vertebral surgery: a case-series analysis. J Biol Regul Homeost Agents. 2019;33:1615-1621. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Dias S, Trovisco S, Neves I, Miranda L, Valente R. Efficacy and Safety of Sufentanil Infusion for Postoperative Analgesia in Cancer Surgery: A Retrospective Cohort Study. Cureus. 2023;15:e38993. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Hu Z, Zhou Y, Zhao G, Zhang X, Liu C, Xing H, Liu J, Wang F. Effects of quadratus lumborum block on perioperative multimodal analgesia and postoperative outcomes in patients undergoing radical prostatectomy. BMC Anesthesiol. 2022;22:213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Haager B, Schmid D, Eschbach J, Passlick B, Loop T. Regional versus systemic analgesia in video-assisted thoracoscopic lobectomy: a retrospective analysis. BMC Anesthesiol. 2019;19:183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, Fiadjoe JE, Greif R, Klock PA, Mercier D, Myatra SN, O'Sullivan EP, Rosenblatt WH, Sorbello M, Tung A. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136:31-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 568] [Article Influence: 189.3] [Reference Citation Analysis (0)] |
| 12. | Jia X, Wang Z, Huang F, Su C, Du W, Jiang H, Wang H, Wang J, Wang F, Su W, Xiao H, Wang Y, Zhang B. A comparison of the Mini-Mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: a cross-sectional study. BMC Psychiatry. 2021;21:485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 347] [Article Influence: 86.8] [Reference Citation Analysis (0)] |
| 13. | Rasheed AM, Amirah MF, Abdallah M, P J P, Issa M, Alharthy A. Ramsay Sedation Scale and Richmond Agitation Sedation Scale: A Cross-sectional Study. Dimens Crit Care Nurs. 2019;38:90-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Hwang WY, Kim K, Cho HY, Yang EJ, Suh DH, No JH, Lee JR, Hwang JW, Do SH, Kim YB. The voiding VAS score is a simple and useful method for predicting POUR after laparoscopy for benign gynaecologic diseases: a pilot study. J Obstet Gynaecol. 2022;42:2469-2473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64590] [Article Influence: 16147.5] [Reference Citation Analysis (176)] |
| 16. | Komici K, Bencivenga L, Navani N, D'Agnano V, Guerra G, Bianco A, Rengo G, Perrotta F. Frailty in Patients With Lung Cancer: A Systematic Review and Meta-Analysis. Chest. 2022;162:485-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 69] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 17. | Gokten OE. Laparoscopic adrenalectomy for suspected adrenal mass in lung cancer: ganglioneuroma. Tumori. 2021;107:NP81-NP83. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Nguyen TK, Nguyen VL, Nguyen TG, Mai DH, Nguyen NQ, Vu TA, Le AN, Nguyen QH, Nguyen CT, Nguyen DT. Lung-protective mechanical ventilation for patients undergoing abdominal laparoscopic surgeries: a randomized controlled trial. BMC Anesthesiol. 2021;21:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Nikoo M, Moazen-Zadeh E, Nikoo N, Javidanbardan S, Kazemi A, Choi F, Vogel M, Gholami A, Tavakoli S, Givaki R, Jazani M, Mohammadian F, Markazi Moghaddam N, Goudarzi N, Schutz C, Jang K, Akhondzadeh S, Krausz M. Comparing opium tincture and methadone for medication-assisted treatment of patients with opioid use disorder: Protocol for a multicenter parallel group noninferiority double-blind randomized controlled trial. Int J Methods Psychiatr Res. 2019;28:e1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Pokorná P, Šíma M, Koch B, Tibboel D, Slanař O. Sufentanil Disposition and Pharmacokinetic Model-Based Dosage Regimen for Sufentanil in Ventilated Full-Term Neonates. Pharmacology. 2021;106:384-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Tang H, Li C, Wang Y, Deng L. Sufentanil Inhibits the Proliferation and Metastasis of Esophageal Cancer by Inhibiting the NF-κB and Snail Signaling Pathways. J Oncol. 2021;2021:7586100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Huang H, Wang S, Lin R, He Z. Sufentanil for Spinal Analgesia during Cesarean Section Delivery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int J Clin Pract. 2022;2022:4741141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 23. | Zhang JR, Jian JJ, Cao LL, Dong N. [Effect of Ropivacaine Combined with Dexmedetomidine for Serratus Anterior Plane Block Plus Patient-Controlled Intravenous Analgesia on Postoperative Recovery Quality of Patients Undergoing Thoracoscopic Radical Resection of Lung Cancer]. Sichuan Da Xue Xue Bao Yi Xue Ban. 2023;54:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 24. | Zhang HY, Jiang XJ, Li Q, Tang XH, Zhu T. Single-Injection Ultrasound-Guided Thoracic Paravertebral Block versus Local Anesthetic Infiltration in Peritoneal Dialysis Catheter Surgeries: A Randomized Controlled Trial. Blood Purif. 2020;49:426-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Miao Z, Wu P, Wang J, Zhou FC, Lin Y, Lu XY, Lv R, Hou QH, Wen QP. Whole-Course Application of Dexmedetomidine Combined with Ketorolac in Nonnarcotic Postoperative Analgesia for Patients with Lung Cancer Undergoing Thoracoscopic Surgery: A Randomized Control Trial. Pain Physician. 2020;23:E185-E193. [PubMed] |
| 26. | Zang H, Shao G, Lou Y. Sufentanil Alleviates Sepsis-Induced Myocardial Injury and Stress Response in Rats through the ERK/GSK-3β Signaling Axis. Evid Based Complement Alternat Med. 2022;2022:9630716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 27. | Qiu L, Zhong G, Hou Z, Lin J, Sun L. Protective Effect of Sufentanil on Myocardial Ischemia-Reperfusion Injury in Rats by Inhibiting Endoplasmic Reticulum Stress. Comput Math Methods Med. 2022;2022:6267720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Hu Q, Wang Q, Han C, Yang Y. Sufentanil attenuates inflammation and oxidative stress in sepsis-induced acute lung injury by downregulating KNG1 expression. Mol Med Rep. 2020;22:4298-4306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 29. | Elbialy ZI, Assar DH, Abdelnaby A, Asa SA, Abdelhiee EY, Ibrahim SS, Abdel-Daim MM, Almeer R, Atiba A. Healing potential of Spirulina platensis for skin wounds by modulating bFGF, VEGF, TGF-ß1 and α-SMA genes expression targeting angiogenesis and scar tissue formation in the rat model. Biomed Pharmacother. 2021;137:111349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 30. | An Y, Zhao L, Wang T, Huang J, Xiao W, Wang P, Li L, Li Z, Chen X. Preemptive oxycodone is superior to equal dose of sufentanil to reduce visceral pain and inflammatory markers after surgery: a randomized controlled trail. BMC Anesthesiol. 2019;19:96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Huang H, Xu X, Xiao Y, Jia J. The Influence of Different Dexmedetomidine Doses on Cognitive Function at Early Period of Patients Undergoing Laparoscopic Extensive Total Hysterectomy. J Healthc Eng. 2021;2021:3531199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |