Published online Apr 19, 2024. doi: 10.5498/wjp.v14.i4.541
Peer-review started: January 19, 2024
First decision: February 5, 2024
Revised: February 19, 2024
Accepted: March 28, 2024
Article in press: March 28, 2024
Published online: April 19, 2024
Processing time: 88 Days and 19.9 Hours
Hematological tumors are common malignant tumors, with high morbidity and mortality rates. Most patients with hematological malignancies develop sleep disorders that seriously affect their life and health because of acute onset of disease, rapid progression, high recurrence rates, complex treatment methods, and treatment costs.
To explore the mediating effect of resilience on fear of disease progression and sleep quality in patients with hematological malignancies.
A cross-sectional analysis of 100 patients with hematological malignancies, treated in the First Affiliated Hospital of Jinzhou Medical University between August 2022 and August 2023, was conducted. Patients were assessed using a general data survey, a simplified scale for the fear of progression (FoP) of disease, a resilience scale, and the Pittsburgh Sleep Quality Index. Statistical analysis was conducted to determine the relationship between various patient characteristics and FoP, resilience, and sleep quality. Spearman’s correlation analysis was used to examine the correlations between mental resilience, FoP, and sleep quality.
The total FoP score mean value in patients with hematological malignancies was 38.09 ± 5.16; the total resilience score mean value was 40.73 ± 7.04; and the Pittsburgh Sleep Quality Index score mean value was 10.72 ± 1.90. FoP, resilience, and sleep quality of the patients were associated with family per capita monthly income and patient education level (P < 0.05). Spearman correlation analysis revealed that FoP was negatively correlated with resilience and sleep quality scores (r = -0.560, -0.537, P < 0.01), respectively, and resilience was significantly associated with sleep quality scores (r = 0.688, P < 0.01). Mediation analysis showed that the mediating effect of resilience between FoP and sleep quality in patients with hematological malignancies was -0.100 and accounted for 50.51% of the total effect. This indicated that FoP directly and indirectly affected sleep quality through the mesomeric effect of resilience.
Resilience is an intermediary variable between FoP and sleep quality in patients with hematological malignancies. Medical staff should evaluate and follow-up FoP and resilience to implement measures to improve sleep quality.
Core Tip: Hematological tumors are common malignant tumors. Most patients with hematological malignancies develop sleep disorders that seriously affect their quality of life and health, owing to the acute onset, rapid progression, and high recurrence rate of these tumors. In this study, we conducted a cross-sectional analysis of 100 patients with hematological malignancies in the oncology department of our hospital. A general data survey, simplified fear of disease progression scale, resilience scale, and the Pittsburgh Sleep Quality Index were used to investigate the mediating effect of resilience between fear of disease progression and sleep quality in patients with hematological malignancies.
- Citation: Tian Y, Wang YL. Resilience provides mediating effect of resilience between fear of progression and sleep quality in patients with hematological malignancies. World J Psychiatry 2024; 14(4): 541-552
- URL: https://www.wjgnet.com/2220-3206/full/v14/i4/541.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i4.541
In recent years, the incidence and mortality of hematological tumors in China have increased[1]. Owing to the characteristics of hematological malignancies, such as acute onset, rapid progression, easy recurrence, complex treatment methods, and high treatment costs[2], concern about the progression or recurrence of the disease may seriously affect physical and mental health as well as sleep quality in patients. The term fear of progression (FoP) denotes a psychological condition marked by apprehension, fear, or worry regarding the potential advancement or recurrence of a medical condition[3]. Studies have shown that FoP is one of the most common pain symptoms in patients with carcinomas and other chronic diseases. An increase in these levels may lead to patient dysfunction and affect happiness, quality of life, and social function[4]. It is difficult to provide an effective relief of symptoms in cancer patients who have an obvious fear of disease progression. FoP is an urgent problem that must be addressed in patients with hematological tumors.
Elevated FoP levels in patients with cancer and other chronic diseases may lead to health dysfunction, including sleep problems. Sleep is an important marker of related functions in the human body and is crucial for maintaining individual physical and mental health[5]. Saletin et al[6] proposed a simple definition of sleep: A reversible behavioral state that is detached and unresponsive to the environment. The typical characteristics of sleep include closed eyes, lying supine, behavioral immobility, and reduced reactivity[6]. However, abnormal conditions may also occur during sleep, such as individuals exhibiting certain behaviors (sleepwalking, somniloquy, grinding teeth) or sleep problems (insomnia, dreaminess, wakefulness)[6]. In view of this, researchers have proposed the concept of sleep quality to better probe the sleep status in individuals. Sleep quality refers to a person’s subjective evaluation of sleep quality, including the evaluation of sleep duration, sleep continuity, and wake-up feelings[7]. However, there is currently no standardized definition of sleep quality. Subjective and objective indicators are used to measure sleep quality, and some instruments convert sleep-related physiological indicators into sleep quality indicators[8,9]. Several studies have shown that patients with cancer have difficulties in initiating or maintaining sleep, wake up earlier than expected, and are unable to fall back to sleep; furthermore, they experience excessive daytime sleepiness and other sleep disorders, which remain as well during the recovery period[10]. Studies have shown that the stronger the fear of recurrence in patients with cancer, the worse their sleep quality[11].
Research has confirmed that the occurrence of sleep disorders is associated with individual negative emotions and mental disorders[12]. Bad mood can lead to decreased sleep quality, and approximately 80% of patients with depression have sleep disorders such as insomnia, early waking, and excessive sleep[13]. Resilience has attracted the attention of many researchers in the field of positive psychology. Resilience refers to an individual’s positive internal coping abilities and good adaptation processes in the face of adversity and trauma. It is a complex internal psychological potential that has a significant impact on the development and growth of an individual[14]. Studies have found that the degree of mental resilience in patients after cancer surgery is inversely proportional to the degree of FoP[15]. Furthermore, resilience has been demonstrated to improve sleep quality[16]. Overall, hematologic malignancies, such as leukemia, lymphoma, and myeloma, usually involve long-term and complex treatment processes, posing significant psychological and emotional burdens on patients and their families. Therefore, psychological resilience plays a crucial role in the study of patients with hematologic malignancies, affecting not only their mental health but also significantly impacting their treatment outcomes and quality of life.
Based on previous studies, in this study, we aimed to investigate the relationship between FoP and quality of sleep in patients with hematological malignancies. To the best of our knowledge, this is the first attempt to explore the mediating effect of resilience on FoP and sleep quality in this group of patients, providing a theoretical basis and practical reference for promoting quality of sleep in these patients from the perspective of FoP.
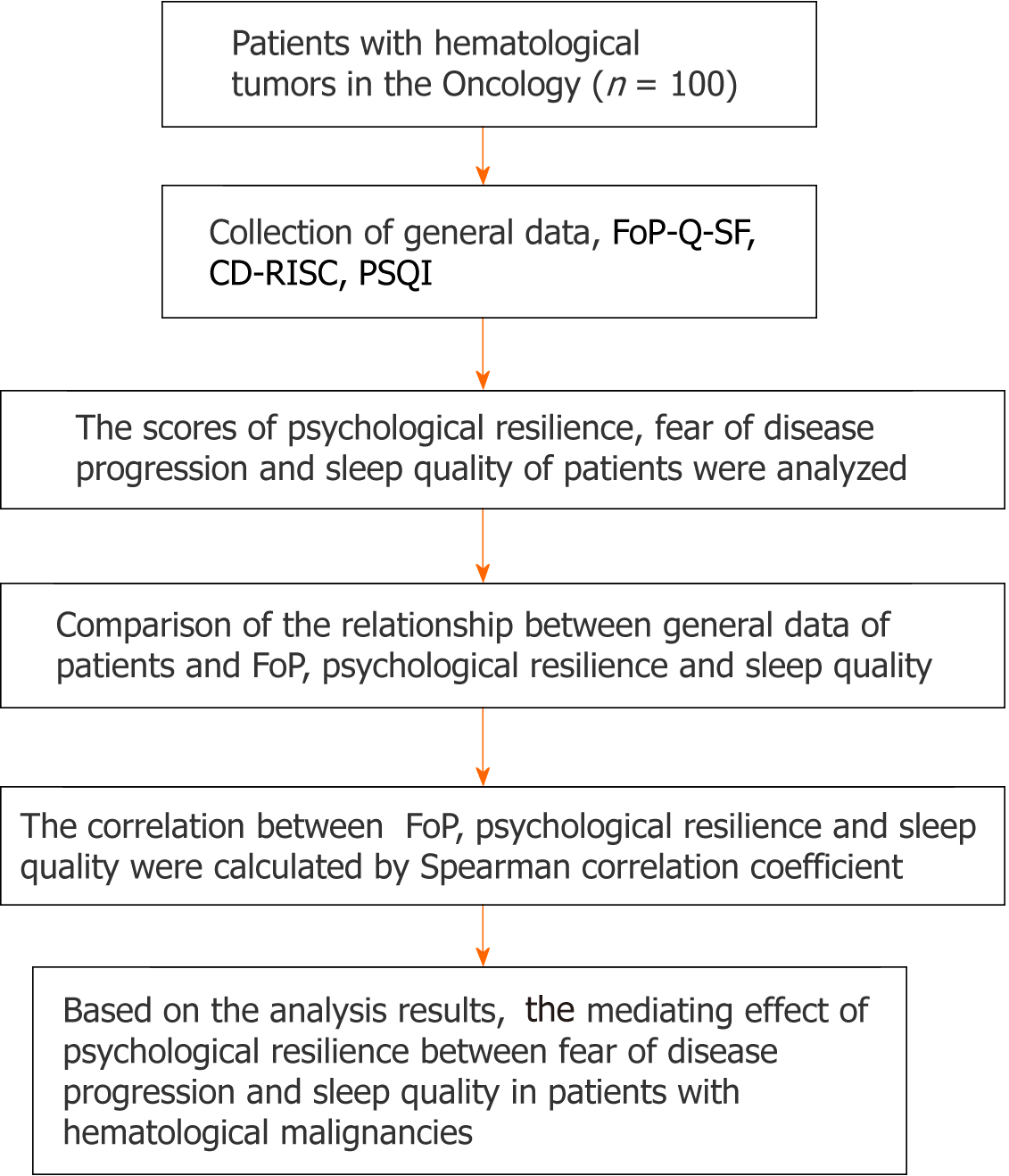
A cross-sectional design was used in this study. The research process is illustrated in Figure 1. One hundred patients with hematologic malignancies treated at the First Affiliated Hospital of Jinzhou Medical University between August 2022 and August 2023 were included in this study. The inclusion criteria were as follows: (1) Patients with hematological malignancies; (2) Age ≥18 years old; (3) Primary school or above education level, able to correctly communicate and answer the questions included in the tests; and (4) Awareness of their illness and willingness to cooperate with the study. The following exclusion criteria were applied: (1) Impairment of cognitive function or other psychiatric diseases; (2) Serious damage to vital organs such as the heart, brain, and kidneys; (3) Malignant tumors at other sites; and (4) Other primary sleep disorders such as sleep apnea syndrome.
Patient data collection: Data regarding sex, age, marital status, education level, average monthly family income, medical payment method, place of residence, occupation type, illness course, religious beliefs, and family history were collected.
FoP Questionnaire-short Form: This instrument was developed by Mehnert et al[17] and translated into Chinese by Cheng et al[18]. The questionnaire includes 12 items and two dimensions: Physical health (six items) and social family (six items) assessed on a 5-point Likert scale (1 = never and 5 = always). Cronbach’s α coefficient was 0.820. On a scale of 12-60 points, the score was correlated to the severity of fear.
Connor-Davidson Resilience scale: The scale was translated and revised into Chinese by Xie et al[19] and included three dimensions: Toughness respectively (13 items), optimism (4 items), and self-strengthening (8 items), with a total of 25 items assessed on a 5-point Likert scale (0 = “never” and 4 = “almost”). Cronbach’s α coefficient was 0.897 and Cronbach’s α coefficient for each table was 0.66-0.88. On a scale of 0-100 points, the higher the sum of the scores in each dimension, the stronger the mental resilience in patients.
Pittsburgh Sleep Quality Index: Buysse et al[8] evaluated sleep quality in hospitalized patients. Cronbach’s α coefficient for the table was 0.750. The scale comprises 18 items, categorized into seven dimensions including sleep efficiency, sleep disorders, sleep time, sleep quality, daytime dysfunction, and use of hypnotic drugs. Each table is scored on a 0-3 scale, with a total score of 0-21. Scores ≥ 8 indicate a sleep disorders. Cronbach’s α coefficient was 0.850.
IBM SPSS (version 26.0) was used to analyze the data. Measurement data are described as mean ± SD, and counting data are described as component ratio (%). Spearman’s rank correlation analysis was used to test the correlations between fear of disease progression, mental resilience, and sleep quality. The macro program Process in IBM SPSS 26.0 was applied to inspect the mediating effect between fear of disease progression, resilience, and sleep quality, and the bootstrap method was applied to verify the mediating effect between mental resilience and fear of disease progression and sleep quality. The test level was α = 0.05, and a P value < 0.05 was considered statistically significant.
The total FoP score mean value in patients with hematologic malignancies was 38.09 ± 5.16. The total resilience score mean value was 40.73 ± 7.04. The total sleep quality score mean value was 10.72 ± 1.90. The scores for each scale are presented in Table 1.
| Project | Number of items | Rating range | Score |
| Fear of disease progression | 12 | 12-60 | 38.09 ± 5.16 |
| Physical health | 6 | 6-30 | 19.56 ± 3.01 |
| Social family | 6 | 6-30 | 18.53 ± 4.06 |
| Resilience | 25 | 0-100 | 40.73 ± 7.04 |
| Toughness | 13 | 0-52 | 19.69 ± 5.45 |
| Optimistic | 4 | 0-16 | 6.33 ± 2.92 |
| Self-strengthening | 8 | 0-32 | 14.70 ± 3.60 |
| Sleep quality | 18 | 0-21 | 10.72 ± 1.90 |
| Sleep efficiency | 1 | 0-3 | 1.30 ± 0.90 |
| Sleep disorders | 9 | 0-3 | 2.36 ± 0.62 |
| Sleeping time | 2 | 0-3 | 2.52 ± 0.64 |
| Sleep time | 1 | 0-3 | 0.56 ± 0.37 |
| Sleep quality | 1 | 0-3 | 2.04 ± 0.77 |
| Daytime dysfunction | 3 | 0-3 | 1.26 ± 0.83 |
| Use of hypnotic drugs | 1 | 0-3 | 0.67 ± 0.56 |
Statistical analysis showed that the FoP, resilience, and sleep quality in patients with hematological malignancies were associated with per capita monthly household income and education level (P < 0.05). The per capita monthly income of households and education level were inversely proportional to the FoP score and directly proportional to the resilience and sleep quality scores (Tables 2-4).
| Projects | Number, n (%) | Score | t/F | P value |
| Sex | ||||
| Male | 49 (49) | 36.46 ± 4.30 | 3.232 | 0.002 |
| Female | 51 (51) | 39.65 ± 5.47 | ||
| Age (yr) | ||||
| ≤ 35 | 34 (34) | 38.69 ± 5.37 | 0.426 | 0.654 |
| 35-60 | 36 (36) | 37.55 ± 3.83 | ||
| ≥ 60 | 30 (30) | 38.04 ± 6.30 | ||
| Marital status | ||||
| Married | 27 (27) | 37.09 ± 4.55 | 0.190 | 0.827 |
| Unmarried | 48 (48) | 39.19 ± 5.55 | ||
| Divorce/widowhood | 25 (25) | 37.04 ± 4.74 | ||
| Family per capita monthly income (RMB) | ||||
| < 3000 | 32 (32) | 41.71 ± 4.65 | 32.112 | 0.000 |
| 3000-5000 | 38 (38) | 38.62 ± 3.27 | ||
| > 5000 | 30 (30) | 33.54 ± 4.23 | ||
| Medical expenses payment method | ||||
| Medical insurance | 46 (46) | 37.54 ± 5.09 | 0.896 | 0.412 |
| Agricultural insurance | 51 (51) | 38.39 ± 5.14 | ||
| Other | 3 (3) | 41.21 ± 7.24 | ||
| Educational level | ||||
| Junior high school and below | 40 (40) | 38.65 ± 4.75 | 3.189 | 0.046 |
| High school/technical secondary school | 41 (41) | 38.76 ± 4.88 | ||
| College degree or above | 19 (19) | 35.45 ± 5.98 | ||
| Type of occupation | ||||
| Employment | 46 (46) | 37.10 ± 4.39 | 1.782 | 0.078 |
| Unemployment | 54 (54) | 38.93 ± 5.65 | ||
| Type of residence | ||||
| Rural | 34 (34) | 39.08 ± 4.09 | 1.396 | 0.166 |
| Town | 66 (66) | 37.57 ± 5.60 | ||
| Disease course | ||||
| Less than 2 yr | 50 (50) | 37.64 ± 5.08 | -0.859 | 0.393 |
| 2 yr and above | 50 (50) | 38.53 ± 5.26 | ||
| Religious beliefs | ||||
| Yes | 5 (5) | 37.99 ± 5.60 | -0.806 | 0.422 |
| No | 95 (95) | 39.90 ± 5.15 | ||
| Family history | ||||
| Yes | 16 (16) | 38.79 ± 4.41 | -0.594 | 0.554 |
| No | 84 (84) | 37.95 ± 5.30 | ||
| Tumor type | ||||
| Leukemia | 29 (29) | 39.15 ± 6.07 | 1.068 | 0.366 |
| Lymphoma | 30 (30) | 37.95 ± 3.79 | ||
| Multiple myeloma | 21 (21) | 36.54 ± 5.21 | ||
| Myelodysplastic syndrome | 20 (20) | 38.38 ± 5.43 |
| Projects | Number, n (%) | Score | t/F | P value |
| Sex | ||||
| Male | 49 (49) | 41.87 ± 7.08 | -1.615 | 0.110 |
| Female | 51 (51) | 39.62 ± 6.88 | ||
| Age (yr) | ||||
| ≤ 35 | 34 (34) | 41.94 ± 5.81 | 1.386 | 0.255 |
| 35-60 | 36 (36) | 40.98 ± 6.73 | ||
| ≥ 60 | 30 (30) | 39.05 ± 8.44 | ||
| Marital status | ||||
| Married | 27 (27) | 40.82 ± 6.23 | 0.877 | 0.419 |
| Unmarried | 48 (48) | 41.48 ± 7.28 | ||
| Divorce/widowhood | 25 (25) | 39.18 ± 7.40 | ||
| Family per capita monthly income (RMB) | ||||
| < 3000 | 32 (32) | 33.56 ± 4.29 | 121.749 | 0.000 |
| 3000-5000 | 38 (38) | 40.54 ± 2.96 | ||
| > 5000 | 30 (30) | 48.60 ± 4.16 | ||
| Medical expenses payment method | ||||
| Medical insurance | 46 (46) | 43.30 ± 6.68 | 2.231 | 0.113 |
| Agricultural insurance | 51 (51) | 39.45 ± 7.21 | ||
| Other | 3 (3) | 38.23 ± 5.98 | ||
| Educational level | ||||
| Junior high school and below | 40 (40) | 38.32 ± 7.23 | 7.744 | 0.001 |
| High school/technical secondary school | 41 (41) | 40.84 ± 5.96 | ||
| College degree or above | 19 (19) | 45.55 ± 6.52 | ||
| Type of occupation | ||||
| Employment | 46 (46) | 41.68 ± 6.96 | -1.25 | 0.214 |
| Unemployment | 54 (54) | 39.92 ± 7.07 | ||
| Type of residence | ||||
| Rural | 34 (34) | 40.58 ± 7.31 | -0.147 | 0.883 |
| Towns | 66 (66) | 40.80 ± 6.95 | ||
| Disease course | ||||
| Less than 2 yr | 50 (50) | 40.92 ± 7.11 | 0.277 | 0.782 |
| 2 yr and above | 50 (50) | 40.53 ± 7.03 | ||
| Religious beliefs | ||||
| Yes | 5 (5) | 40.50 ± 3.59 | 0.073 | 0.942 |
| No | 95 (95) | 40.74 ± 7.18 | ||
| Family history | ||||
| Yes | 16 (16) | 40.79 ± 7.21 | 0.192 | 0.848 |
| No | 84 (84) | 40.42 ± 6.23 | ||
| Tumor type | ||||
| Leukemia | 29 (29) | 39.67 ± 6.71 | 0.841 | 0.475 |
| Lymphoma | 30 (30) | 39.92 ± 7.50 | ||
| Multiple myeloma | 21 (21) | 41.90 ± 7.82 | ||
| Myelodysplastic syndrome | 20 (20) | 42.23 ± 5.90 |
| Projects | Number, n (%) | Score | t/F | P value |
| Sex | ||||
| Male | 49 (49) | 10.87 ± 1.90 | -0.762 | 0.448 |
| Female | 51 (51) | 10.58 ± 1.99 | ||
| Age (yr) | ||||
| ≤ 35 | 34 (34) | 10.80 ± 1.68 | 0.248 | 0.781 |
| 35-60 | 36 (36) | 10.82 ± 1.70 | ||
| ≥ 60 | 30 (30) | 1.52 ± 2.35 | ||
| Marital status | ||||
| Married | 27 (27) | 10.62 ± 1.74 | 0.599 | 0.551 |
| Unmarried | 48 (48) | 10.93 ± 2.10 | ||
| Divorce/widowhood | 25 (25) | 10.44 ± 1.65 | ||
| Family per capita monthly income (RMB) | ||||
| < 3000 | 32 (32) | 8.98 ± 1.23 | 58.580 | 0.000 |
| 3000-5000 | 38 (38) | 10.76 ± 1.21 | ||
| > 5000 | 30 (30) | 12.53 ± 1.44 | ||
| Medical expenses payment method | ||||
| Medical insurance | 46 (46) | 10.93 ± 1.83 | 0.558 | 0.574 |
| Agricultural insurance | 51 (51) | 10.56 ± 1.91 | ||
| Other | 3 (3) | 10.24 ± 3.11 | ||
| Educational level | ||||
| Junior high school and below | 40 (40) | 10.13 ± 1.75 | 8.12 | 0.001 |
| High school/technical secondary school | 41 (41) | 10.67 ± 1.70 | ||
| College degree or above | 19 (19) | 12.11 ± 1.98 | ||
| Type of occupation | ||||
| Employment | 46 (46) | 10.82 ± 1.64 | -0.48 | 0.632 |
| Unemployment | 54 (54) | 10.64 ± 2.10 | ||
| Type of residence | ||||
| Rural | 34 (34) | 10.36 ± 1.55 | -1.388 | 0.168 |
| Towns | 66 (66) | 10.91 ± 2.04 | ||
| Disease course | ||||
| Less than 2 yr | 50 (50) | 10.78 ± 1.79 | 0.292 | 0.771 |
| 2 yr and above | 50 (50) | 10.67 ± 2.01 | ||
| Religious beliefs | ||||
| Yes | 5 (5) | 11.21 ± 2.13 | -0.586 | 0.559 |
| No | 95 (95) | 10.70 ± 1.89 | ||
| Family history | ||||
| Yes | 16 (16) | 10.76 ± 1.91 | 0.509 | 0.612 |
| No | 84 (84) | 10.50 ± 1.84 | ||
| Tumor type | ||||
| Leukemia | 29 (29) | 10.38 ± 1.98 | 0.890 | 0.449 |
| Lymphoma | 30 (30) | 10.75 ± 1.80 | ||
| Multiple myeloma | 21 (21) | 11.26 ± 2.12 | ||
| Myelodysplastic syndrome | 20 (20) | 10.63 ± 1.66 |
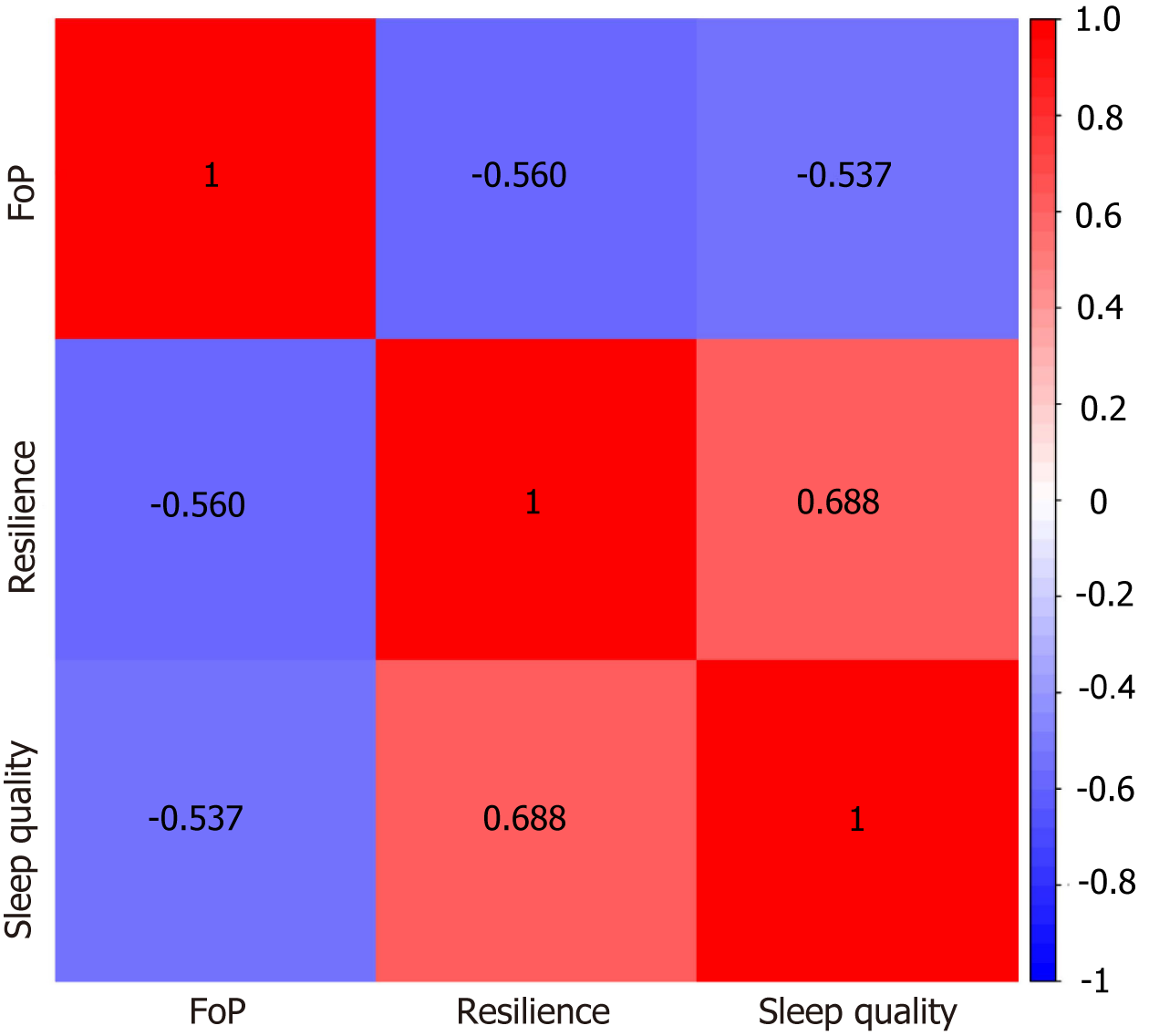
Spearman’s correlation analysis was performed on the FoP, resilience, and sleep quality in patients with hematological malignancies, and the results revealed that FoP was negatively correlated with resilience and sleep quality scores (r = -0.560, -0.537, P < 0.01). Resilience was significantly associated with sleep quality scores (r = 0.688, P < 0.01) (Table 5 and Figure 2).
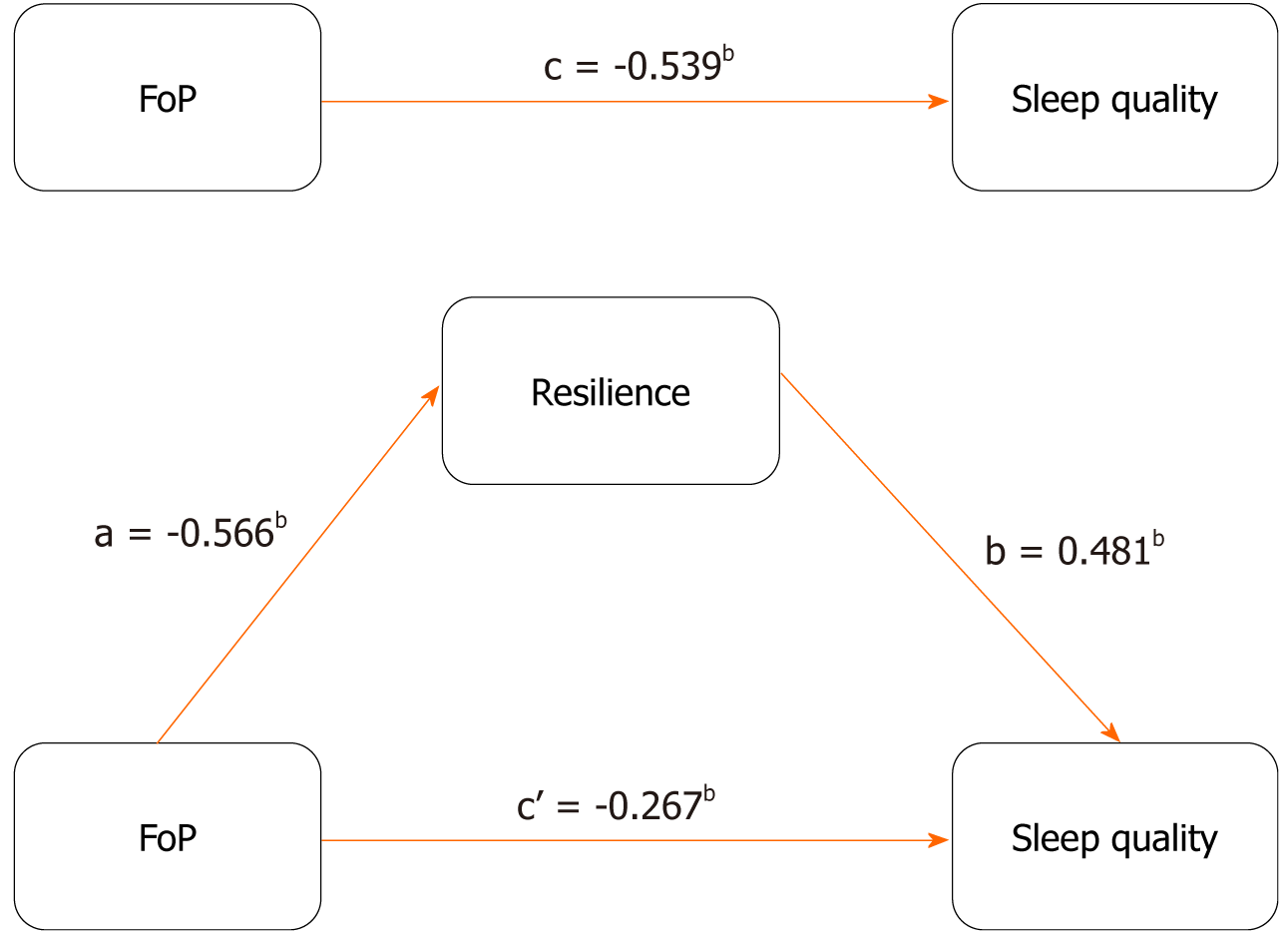
Using the FoP in patients with hematological malignancies as an independent variable (X), resilience as a mediating variable (M), and sleep quality (Y) as a dependent variable, SPSS 26.0, Macro Process Model 4 was applied to analyze the mediating effect of resilience. Regression analysis indicated that the total effect value “c” of FoP on sleep quality was -0.539 (P < 0.05). The regression coefficient “a” of FoP on resilience was -0.566 (P < 0.05). The regression coefficient “b” of resilience on sleep quality was 0.481 (P < 0.05). When resilience was added, the direct effect value “c’” of FoP on resilience was -0.267, which was still significant (P < 0.05). These results suggest that resilience mediates the relationship between FoP and sleep quality in patients with hematological malignancies. The bootstrap method was used to further examine the mediating effects of resilience. The results showed that the mediating effect value was -0.100 (95% confidence interval: -0.139 to -0.068), indicating that the mediating effect of resilience was established and accounted for 50.51% of the total effect (Tables 6 and 7, Figure 3).
| Effect relationship | Effect value | Standard error | 95%CI | Proportion of effect (%) | |
| Lower limit | Upper limit | ||||
| Total effect | -0.198 | 0.031 | -0.260 | -0.136 | 100.00 |
| Direct effect | -0.098 | 0.034 | -0.165 | -0.031 | 49.49 |
| Indirect effect | -0.100 | 0.018 | -0.139 | -0.068 | 50.51 |
Hematological malignancies are common; owing to characteristics such as acute onset, long treatment cycle, and high risk of recurrence, these tumors have a considerable physical and mental impact on patients. Optimizing the sleep quality in patients has recently attracted significant research attention. In this study, a cross-sectional analysis of 100 patients with hematologic malignancies in our hospital showed that FoP could affect patient sleep quality directly as well as indirectly through the mediating effect of resilience.
The purpose of this study was to improve our understanding of the mediating effect of resilience between FoP and sleep quality in patients with hematologic malignancies. This study utilized a cross-sectional design to ascertain the prevalence of blood cancers in certain populations, along with associated risk or protective factors. Cross-sectional designs are advantageous owing to their cost-efficiency and ease of implementation, enabling concurrent investigation into the progression of blood cancers, psychological resilience, and sleep quality. Nevertheless, the simultaneous data collection precludes direct demonstration of causality between variables or the observation of how these variables change over time. Consequently, in this study, we have advanced to using mediation effect analysis to assess the causal links among variables. Additionally, future studies should incorporate longitudinal research to better understand the dynamic interrelations among the variables.
First, using general data and FoP Questionnaire-short Form, Connor-Davidson Resilience scale and Pittsburgh Sleep Quality Index surveys, we found that the total FoP score mean value in patients with hematological malignancies was 38.09 ± 5.16, which was slightly higher than that described by Zhang et al[20]. The total resilience score of 40.73 ± 7.04 was consistent with the results reported by Greup et al[21] in a study on young patients with cancer. The total sleep quality score of 10.72 ± 1.90 was similar to that reported by Fox et al[10] in a study on sleep quality in patients with cancer during chemotherapy[22]. Furthermore, the FoP, resilience, and sleep quality in patients were associated with per capita monthly family income and educational level, which was consistent with results of both domestic and international research[23-25]. Family per capita monthly income and education level are among the problems faced by patients with hematologic tumors. Enhancing sleep quality necessitates a heightened focus on individual patient factors during the disease management process, encompassing aspects such as family income, educational attainment, and occupational stress levels.
Second, Spearman’s correlation analysis demonstrated that the progression of fear of disease was negatively correlated with resilience and sleep quality scores (r = -0.560, -0.537, P < 0.01), and resilience was significantly associated with sleep quality scores (r = 0.688, P < 0.01). The reasons for these results may be as follows: The factors of FoP in patients with hematological malignancies mainly include persistent pain, fatigue, anxiety, and depression related to the disease itself and its treatment[26], which also affect sleep quality to varying degrees[27]. However, external factors played an important role in the degree of pressure affecting the patients in this study. These included concerns over practical problems caused by the disease, such as poor mental state and decreased physical function, family economic difficulties, lower career competitiveness after returning to work, and the possibility of cancer recurrence or metastasis. Decreased ability to regulate negative emotions[28,29]. Patients with poor mental resilience often immerse themselves in their own thoughts, which aggravates the production of negative emotions and affects their sleep quality. Therefore, fear of recurrence, resilience, and sleep quality in patients with cancer are correlated.
Finally, in the results of mediation analysis, we found that resilience played a mediating role between the FoP of disease and sleep quality. That is, FoP (c = -0.539, P < 0.05) and resilience (b = 0.481, P < 0.05) had predictive effects on quality of sleep in patients with hematological malignancies. In addition, the FoP of disease could indirectly predict sleep quality in patients with hematologic malignancies through resilience (c’ = -0.267, P < 0.05), with a mediating effect size of 50.51%. There are several explanations for these results. First, FoP has an important impact on sleep quality. Cancer is a major stressor and negative event in individuals. Patients are prone to negative emotions such as loneliness, meaninglessness, worthlessness, and guilt due to decreased physical function, changes in social roles, increased leisure time, and high treatment costs, leading to sleep disorders[30-32]. Moderate fear can be the driving force of self-health management among patients; however, excessive fear can further aggravate negative emotions and sleep disorders. Second, poor mental resilience aggravates sleep disorders. Patients with fear of the disease experience significant psychological pressure and are more prone to anxiety and depression. It is necessary to show positive emotions such as optimism, tenacity, and self-improvement, and take actions such as actively seeking external support to promote physical and mental health and alleviate negative emotions[33]. In contrast, patients with hematological malignancies with low psychological resilience are prone to social withdrawal, avoidance of social activities, and other escape behaviors when facing stressful events. Thus, these patients receive less social support and are more likely to breed negative emotions, such as pessimism and despair, which further aggravates the FoP and affects their sleep quality[34]. Among them, cognitive-behavioral therapy, meditation, stress management training, relaxation techniques, and adjustments in daily routines are effective to enhance patients’ psychological resilience. Notably, family and social support for blood cancer patients are of utmost importance. A supportive social environment and peaceful, joyful family life often significantly boost patients’ psychological resilience, which in turn improves their sleep quality and prognosis. Therefore, it is important that medical intervention targeting sleep disorders in patients with hematological malignancies strengthens their resilience. In clinical practice, clinicians should pay attention to the psychological status in patients, help them establish a strong, optimistic, and self-strengthening mentality, and reduce negative psychological problems. Fur
This study has some limitations. First, owing to the limitations of manpower and material resources, this study only selected patients with hematological malignancies from one hospital; therefore, the sampling was not sufficiently comprehensive. Second, a questionnaire survey was used to measure the studied variables, and patient attitudes when completing these questionnaires may have affected the validity of the research results. Therefore, in future research, qualitative interviews should be conducted.
This cross-sectional investigation explored the mediating role of resilience on FoP and sleep quality in patients with hematological malignancies. Our results showed that sleep quality in patients was suboptimal. Further, FoP can directly affect sleep quality and play an indirect role through resilience, which may furnish treatment decisions for the intervention in patients with blood tumors who have FoP. Medical staff should focus on the progression of fear of disease and the level of resilience in patients with hematological malignancies, to implement effective measures to reduce excessive fear in patients, improve the effectiveness of disease management, and promote sleep quality.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single-blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Giannouli V, Greece S-Editor: Wang JJ L-Editor: A P-Editor: Zhang YL
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64104] [Article Influence: 16026.0] [Reference Citation Analysis (174)] |
| 2. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12667] [Cited by in RCA: 15276] [Article Influence: 3055.2] [Reference Citation Analysis (4)] |
| 3. | Clarke RT, Van den Bruel A, Bankhead C, Mitchell CD, Phillips B, Thompson MJ. Clinical presentation of childhood leukaemia: a systematic review and meta-analysis. Arch Dis Child. 2016;101:894-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 78] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | McCarten KM, Nadel HR, Shulkin BL, Cho SY. Imaging for diagnosis, staging and response assessment of Hodgkin lymphoma and non-Hodgkin lymphoma. Pediatr Radiol. 2019;49:1545-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 5. | Cheng W, Rolls E, Gong W, Du J, Zhang J, Zhang XY, Li F, Feng J. Sleep duration, brain structure, and psychiatric and cognitive problems in children. Mol Psychiatry. 2021;26:3992-4003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 109] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 6. | Saletin JM, Hilditch CJ, Dement WC, Carskadon MA. Short Daytime Naps Briefly Attenuate Objectively Measured Sleepiness Under Chronic Sleep Restriction. Sleep. 2017;40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Buysse DJ. Sleep health: can we define it? Sleep. 2014;37:9-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1315] [Cited by in RCA: 1444] [Article Influence: 131.3] [Reference Citation Analysis (0)] |
| 8. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17520] [Cited by in RCA: 21864] [Article Influence: 607.3] [Reference Citation Analysis (0)] |
| 9. | McCarter SJ, Hagen PT, St Louis EK, Rieck TM, Haider CR, Holmes DR, Morgenthaler TI. Physiological markers of sleep quality: A scoping review. Sleep Med Rev. 2022;64:101657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 10. | Fox RS, Ancoli-Israel S, Roesch SC, Merz EL, Mills SD, Wells KJ, Sadler GR, Malcarne VL. Sleep disturbance and cancer-related fatigue symptom cluster in breast cancer patients undergoing chemotherapy. Support Care Cancer. 2020;28:845-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 104] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 11. | Kim H, Cho IK, Lee D, Kim K, Lee J, Cho E, Park CHK, Chung S. Effect of Cancer-Related Dysfunctional Beliefs About Sleep on Fear of Cancer Progression in the Coronavirus Pandemic. J Korean Med Sci. 2022;37:e272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 12. | Herrero-Sánchez MD, García-Iñigo Mdel C, Nuño-Beato-Redondo BS, Fernández-de-Las-Peñas C, Alburquerque-Sendín F. Association between ongoing pain intensity, health-related quality of life, disability and quality of sleep in elderly people with total knee arthroplasty. Cien Saude Colet. 2014;19:1881-1888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Doghramji K. Treatment strategies for sleep disturbance in patients with depression. J Clin Psychiatry. 2003;64 Suppl 14:24-29. [PubMed] |
| 14. | Presley CJ, Arrato NA, Shields PG, Carbone DP, Wong ML, Benedict J, Reisinger SA, Han L, Gill TM, Allore H, Andersen BL, Janse S. Functional Trajectories and Resilience Among Adults With Advanced Lung Cancer. JTO Clin Res Rep. 2022;3:100334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Fernandes CFL, Coelho BP, Souza MCDS, Boccacino JM, Soares SR, Araújo JPA, Melo-Escobar MI, Lopes MH. Extracellular vesicles throughout development: A potential roadmap for emerging glioblastoma therapies. Semin Cell Dev Biol. 2023;133:32-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Wallace RA, Webb PM, Schluter PJ. Environmental, medical, behavioural and disability factors associated with Helicobacter pylori infection in adults with intellectual disability. J Intellect Disabil Res. 2002;46:51-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. [Fear of progression in breast cancer patients--validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF)]. Z Psychosom Med Psychother. 2006;52:274-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 159] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 18. | Cheng HL, Li MC, Leung DYP. Psychometric Testing of the Traditional Chinese Version of the Fear of Progression Questionnaire-Short Form in Cancer Survivors. J Nurs Meas. 2022;30:707-720. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Xie Y, Peng L, Zuo X, Li M. The Psychometric Evaluation of the Connor-Davidson Resilience Scale Using a Chinese Military Sample. PLoS One. 2016;11:e0148843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Zhang L, Shi Y, Deng J, Yi D, Chen JA. The effect of health literacy, self-efficacy, social support and fear of disease progression on the health-related quality of life of patients with cancer in China: a structural equation model. Health Qual Life Outcomes. 2023;21:75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 21. | Greup SR, Kaal SEJ, Jansen R, Manten-Horst E, Thong MSY, van der Graaf WTA, Prins JB, Husson O. Post-Traumatic Growth and Resilience in Adolescent and Young Adult Cancer Patients: An Overview. J Adolesc Young Adult Oncol. 2018;7:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 22. | Herschbach P, Dinkel A. Fear of progression. Recent Results Cancer Res. 2014;197:11-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 23. | VanMeter F, Cicchetti D. Resilience. Handb Clin Neurol. 2020;173:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 24. | Price S, Hamann HA, Halaby L, Trejo J, Rogers FC, Weihs K. Collaborative depression care sensitive to the needs of underserved patients with cancer: Feasibility, acceptability and outcomes. J Psychosoc Oncol. 2024;42:90-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 25. | Melhem SJ, Nabhani-Gebara S, Kayyali R. Informational needs and predictors of Jordanian breast and colorectal cancer survivors: a national cross-sectional study. Support Care Cancer. 2022;30:6827-6837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 26. | Chen D, Yin Z, Fang B. Measurements and status of sleep quality in patients with cancers. Support Care Cancer. 2018;26:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 88] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 27. | Bluethmann SM, Basen-Engquist K, Vernon SW, Cox M, Gabriel KP, Stansberry SA, Carmack CL, Blalock JA, Demark-Wahnefried W. Grasping the 'teachable moment': time since diagnosis, symptom burden and health behaviors in breast, colorectal and prostate cancer survivors. Psychooncology. 2015;24:1250-1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 28. | Damen MDC, Westerweel PE, Levin MD, Pelle AJ. Unmet supportive care needs, anxiety and depression in haematology patients during watch-and-wait. Psychooncology. 2022;31:176-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Kim SH, Lee S, Kim SH, Ok ON, Kim IR, Choi E, Kang YK, Kim SJ, Lee MH. Unmet needs of non-Hodgkin lymphoma survivors in Korea: prevalence, correlates, and associations with health-related quality of life. Psychooncology. 2017;26:330-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Kuang X, Long F, Chen H, Huang Y, He L, Chen L, Xie L, Li J, Luo Y, Tao H. Correlation research between fear of disease progression and quality of life in patients with lung cancer. Ann Palliat Med. 2022;11:35-44. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Hanprasertpong J, Geater A, Jiamset I, Padungkul L, Hirunkajonpan P, Songhong N. Fear of cancer recurrence and its predictors among cervical cancer survivors. J Gynecol Oncol. 2017;28:e72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 32. | Faghani S, Mohammadian R, Rahmani A, Mohajjel-Aghdam AR, Hassankhani H, Azadi A. Supportive Care Needs of Iranian Cancer Survivors and Relationships with Social Support. Asian Pac J Cancer Prev. 2015;16:6339-6345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Haviland J, Sodergren S, Calman L, Corner J, Din A, Fenlon D, Grimmett C, Richardson A, Smith PW, Winter J; members of Study Advisory Committee, Foster C. Social support following diagnosis and treatment for colorectal cancer and associations with health-related quality of life: Results from the UK ColoREctal Wellbeing (CREW) cohort study. Psychooncology. 2017;26:2276-2284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 34. | Sivertsen B, Harvey AG, Pallesen S, Hysing M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J Sleep Res. 2015;24:11-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |