Published online Dec 19, 2024. doi: 10.5498/wjp.v14.i12.1845
Revised: October 26, 2024
Accepted: November 1, 2024
Published online: December 19, 2024
Processing time: 63 Days and 3.4 Hours
Owing to the particularities of their physical characteristics, older patients undergoing surgery under general anesthesia experience great surgical traumas. Thus, exploring more refined and individualized nursing approaches is an urgent need to mitigate the negative effects of surgery on such patients.
To analyze the influence of preoperative comprehensive education on anxiety, depression, pain, and sleep in older patients who underwent surgery under general anesthesia.
In total, 163 older adults who underwent surgery under general anesthesia between June 2022 and November 2023 were selected, 77 of them received routine nursing care (control group), and 86 received preoperative comprehensive education (research group). Subsequently, comparative analyses were performed from the following perspectives: Surgical indicators (operation time, time to complete regain of consciousness, and temperature immediately after the proce
The research group had significantly lower operation time and time to complete regain of consciousness than the control group after nursing care and markedly better recovery of postoperative body temperature and body temperature at awakening. In addition, more notable decreases in SAS, SDS, VAS, and PSQI scores were observed in the research group than in the control group. Furthermore, the incidence rate of sleep disturbance (8.14% vs 29.87%) and adverse events (4.65% vs 19.48%) were lower in the research group than in the control group.
Preoperative comprehensive education in older patients who underwent surgery under general anesthesia can improve postoperative indicators, effectively reduce the occurrence of anxiety and depression, alleviate postoperative pain, and improve sleep quality.
Core Tip: This study primarily analyzed the influence of preoperative comprehensive education on anxiety, depression, pain, and sleep in older patients who underwent surgery under general anesthesia to address the relatively greater surgical traumas endured by older patients owing to their particular physical characteristics. We conducted a comprehensive analysis from multiple dimensions, including surgical indicators, negative emotions, pain levels, sleep quality, incidence of sleep disturbances, and the incidence of adverse events. Providing comprehensive preoperative education to older patients undergoing surgery under general anesthesia can improve postoperative indicators, significantly reduce anxiety and depression, alleviate postoperative pain, and enhance patients’ sleep quality. Our findings can provide more optimized management options for older patients undergoing general anesthesia surgery.
- Citation: Qu L, Ma R, Ma YK, Zhao X, Jin J, Zhu QQ, Chen XY, Xu GP. Influence of preoperative comprehensive education on anxiety, depression, pain, and sleep in elderly patients operated under general anesthesia. World J Psychiatry 2024; 14(12): 1845-1853
- URL: https://www.wjgnet.com/2220-3206/full/v14/i12/1845.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i12.1845
Anesthesia plays a crucial role in the surgical process because it can inhibit the function of the central and peripheral nervous systems, thereby temporarily depriving the patient of pain sensation and providing a guarantee for smooth surgical progress[1]. General anesthesia is a frequently employed form of anesthesia in surgical procedures[2]. However, for patients who underwent surgery under general anesthesia, particularly older adults who require higher doses of drugs to achieve anesthesia and analgesia, their health is compromised to a certain extent[3]. Considering the particular physical characteristics of older patients and surgical trauma, appropriate preventive measures must be taken when performing surgery under general anesthesia[4].
As the number of patients receiving general anesthesia continues to increase, optimizing and improving the overall quality of care have become core issues in surgical care[5]. However, surgery as a strong external stimulus often causes both physical and mental stress to patients, which may trigger adverse stress reactions and adversely affect patients’ recovery[6]. Therefore, more sophisticated and individualized care methods must be explored to reduce the negative effects of surgery on patients[7]. Routine nursing care for patients who underwent surgery under general anesthesia can help them quickly respond to complications and take timely measures to ensure patient safety. However, this nursing model is ineffective in promoting rapid recovery and reducing complications, which limits its clinical application[8]. On the contrary, one-on-one preoperative physiotherapy education sessions were found to effectively shorten the postoperative hospital stay and reduce the number of postoperative visits in patients who underwent total arthroplasty[9]. Moreover, preoperative comprehensive education, as a form of preoperative physical therapy education, is essentially a cognitive orientation that elaborates on the anesthesia methods to be used in the operation and informs patients in advance of physical reactions they may encounter during their postoperative regain of consciousness[10]. This education intervention aims to prepare the patient psychologically and adjust the patient’s perception of the procedure, thereby relieving tension and eliminating the effects of negative emotions[11]. Another study showed that for colorectal surgery requiring catheterization (using tetracaine mucus), patients who received preoperative simulated education experienced significantly mild catheter-induced bladder discomfort and postoperative pain within 6 hours after the operation compared with those who did not receive such education[12].
This study included 163 older patients who underwent surgery under general anesthesia to comparatively analyze the effects of preoperative comprehensive education on anxiety, depression, pain, and sleep in these patients.
This retrospective study included 163 patients who underwent surgery under general anesthesia between June 2022 and November 2023. Seventy-seven participants (control group) received routine nursing care, whereas 86 (research group) received comprehensive preoperative education.
Inclusion criteria: Patients who received surgical treatment and could tolerate general anesthesia, had normal temperature measured before surgery, and were > 65 years old.
Exclusion criteria: Preoperative fever and infection; abnormal function of vital organs, such as the heart, liver, kidneys, and lungs; cognitive dysfunction; recovery affected by other drug interventions; failure to effectively control diabetes and hypertension; and coagulation dysfunction.
The control group was cared for by routine nursing interventions: Patients received daily health education and psychological support to enhance their understanding of the surgery process under general anesthesia and help them lessen their psychological stress and negative emotions. In addition, they were guided to perform preoperative preparations such as fasting and water prohibition. The operating room temperature was adjusted to an appropriate level, and all instruments needed for the operation were comprehensively inspected to ensure that everything was in good condition. To manage possible emergencies, corresponding emergency items were also prepared. During the procedure, nurses worked closely with the anesthesiologists and surgeons and monitored the patient’s vital signs in real time to ensure the safety and smooth progress of the procedure.
The research group received comprehensive education interventions: (1) Admission evaluation: The patient underwent a comprehensive physical examination upon admission, and based on the results of the examination and questionnaire, a detailed admission evaluation form, particularly the assessment of anesthesia risk, was developed. For high-risk patients identified during anesthesia evaluation, specialized clinical coping strategies and nursing plans were formulated in advance to provide better medical services. Patients who undergo surgery under general anesthesia often bear a heavy psychological burden because of their severe and complex condition and aggravated anxiety because of upcoming major surgical procedures. Therefore, since admission to the hospital, the nursing staff explained the importance of surgical treatment and previous successful cases to appease their emotions and encourage them to wait for the surgery with peace of mind. The nursing staff also explained the necessity of general anesthesia to patients to dispel their concerns;
(2) Psychological nursing: Through active communication, medical staff helped family members to face patients’ condition with a more optimistic attitude, thereby providing necessary family support for patients, inspiring their yearning for a new postoperative life, and helping them face surgery and illness more bravely. To allow patients and their families have a deeper understanding of the disease, surgery, and general anesthesia, nurses provided relevant knowledge, particularly possible adverse reactions caused by anesthesia, prepared patients for minor postoperative discomfort and reduced psychological and physiological stress reactions;
(3) Intraoperative thermal insulation: During the operation, nursing staff paid special attention to the patient’s thermal insulation and closely monitored vital signs. To ensure the stability of the patient’s body temperature, the fluids used for fluid replacement were preheated and kept at approximately 37 °C to prevent a sudden drop in the body temperature and local blood circulation caused by a large volume of low-temperature fluids entering the body quickly;
And (4) Postoperative care: After the operation, the patients were transferred to the postanesthesia care unit, where the nursing staff would choose a comfortable posture for them and regularly assisted them in adjusting their posture to ensure a smooth respiratory tract. Once changes in the patient’s vital signs were noted, the nursing staff immediately notified the doctor and took appropriate measures promptly. When patients gradually regained consciousness, nurses inquired about their feelings in time, and analgesic drugs were administered as prescribed for those with unbearable pain.
Surgical indicators: The surgical indicators of the two groups were recorded in detail and compared. These parameters include the operation time (OT), time to complete regain consciousness, and temperature (measured using an infrared tympanic thermometer) immediately after the procedure and upon recovery from anesthesia.
Negative emotions: Before and after nursing care, a comprehensive assessment of the patient’s psychological state was conducted using the specialized self-rating anxiety scale (SAS) and self-rating depression scale (SDS). An SAS score > 50 points and an SDS score > 53 points indicate anxiety and depression symptoms, respectively. Higher scores indicate greater anxiety or depression.
Pain severity: Pain levels before and after nursing were evaluated using the visual analog scale (VAS). The score is capped at a score of 10, and the resulting score is proportional to the level of pain felt, i.e., higher scores indicate more intense pain experienced by the patient.
Sleep quality: The Pittsburgh sleep quality index (PSQI) was used to evaluate the sleep quality of patients before and after receiving nursing care. The total scale score is 21 points, and the score is inversely proportional to sleep quality; that is, the higher the score, the less satisfactory the patient’s sleep quality.
Incidence of sleep disturbances: The incidence of sleep disorders in the two groups, such as difficulties in falling asleep for the first time, falling asleep after waking up frequently at night, falling asleep again after waking up early, and falling asleep all night, were observed and recorded.
Adverse events: The incidences of respiratory tract obstruction, catheter detachment, aspiration, and asphyxia were recorded.
The normality test for quantitative data was conducted using the Kolmogorov–Smirnov test. The quantitative data are expressed by as means ± SE. The independent sample t-test was used for intergroup comparisons, whereas paired t-tests were used for intragroup comparisons before and after treatment. Categorical data are presented as the number of cases (percentages), and χ2 tests were used for intergroup comparisons. All data analyses were performed using IBM SPSS Statistics for Windows version 22.0 (Armonk, NY, United States). Significance was indicated by a P value < 0.05.
The research and control groups did not differ significantly in terms of age, body mass index, sex, American Society of Anesthesiologists grading, surgical grading, and anesthesia mode (P > 0.05; Table 1).
| Indicators | Research group (n = 86) | Control group (n = 77) | χ2/t | P value |
| Age (years old) | 57.63 ± 7.39 | 58.44 ± 6.81 | 0.725 | 0.469 |
| Body mass index (kg/m2) | 21.31 ± 2.37 | 21.55 ± 2.24 | 0.662 | 0.509 |
| Sex | 1.086 | 0.297 | ||
| Male | 45 (52.33) | 34 (44.16) | ||
| Female | 41 (47.67) | 43 (55.84) | ||
| ASA grading | 0.034 | 0.983 | ||
| Grade I | 34 (39.53) | 30 (38.96) | ||
| Grade II | 29 (33.72) | 27 (35.06) | ||
| Grade III | 23 (26.74) | 20 (25.97) | ||
| Surgical grading | 0.237 | 0.972 | ||
| Grade I | 21 (24.42) | 18 (23.38) | ||
| Grade II | 25 (29.07) | 22 (28.57) | ||
| Grade III | 24 (27.91) | 24 (31.17) | ||
| Grade IV | 16 (18.60) | 13 (16.88) | ||
| Anesthesia mode | 0.547 | 0.908 | ||
| Epidural anesthesia | 27 (31.40) | 23 (29.87) | ||
| Subarachnoid block | 15 (17.44) | 11 (14.29) | ||
| Block anesthesia | 18 (20.93) | 19 (24.68) | ||
| Combined spinal-epidural anesthesia | 26 (30.23) | 24 (31.17) |
In the two groups, the surgical indicators observed were the OT, time to complete regain of consciousness, temperature immediately after the procedure, and temperature upon recovery from anesthesia before and after nursing. After nursing, the OT and time to complete regain of consciousness were significantly lower in the research group than in the control group, whereas the temperatures immediately after the procedure and upon recovery from anesthesia were significantly better (P < 0.05; Table 2).
| Groups | n | Operation time (minute) | Time to complete regain of consciousness (minute) | Temperature immediately after the procedure (°C) | Temperature upon recovery from anesthesia (°C) |
| Research group | 86 | 143.17 ± 13.31 | 27.90 ± 2.66 | 36.38 ± 1.04 | 36.85 ± 0.49 |
| Control group | 77 | 188.12 ± 19.26 | 43.09 ± 3.17 | 35.62 ± 0.82 | 36.09 ± 0.64 |
| t | - | 17.480 | 33.250 | 5.139 | 8.562 |
| P value | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
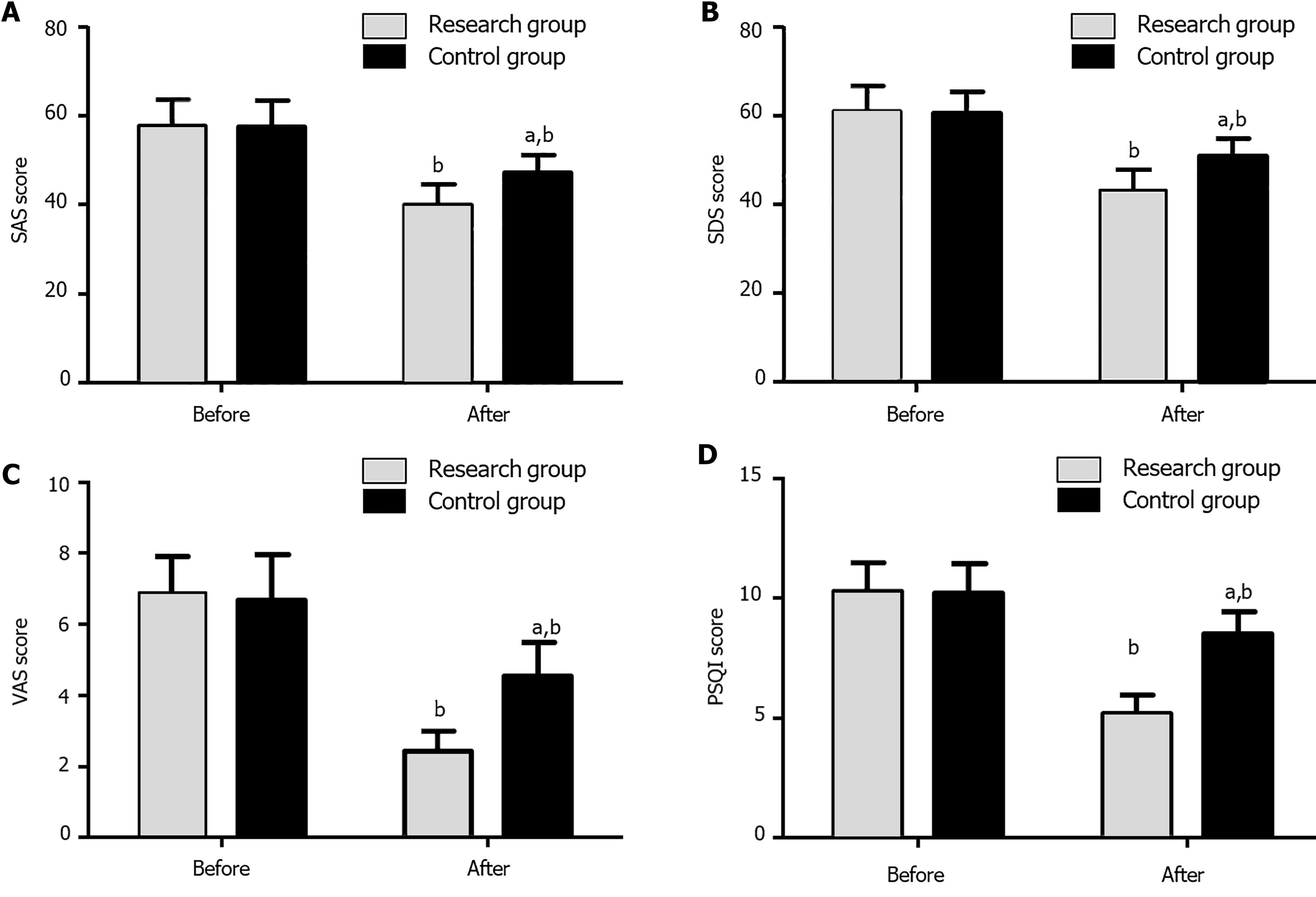
The psychological states of the patients in the two groups were evaluated by SAS and SDS. No significant intergroup differences were found in SAS and SDS scores before nursing care (P > 0.05). After nursing care, the SAS and SDS scores of both groups were significantly reduced, with a more notable decrease in the research group than in the control group (P < 0.05; Figure 1A and B).
A light difference in the VAS scores was noted between the two groups before nursing care (P > 0.05). An obvious decrease in VAS scores was observed in both groups after nursing care. Moreover, the research group had a more significant decrease in VAS scores than the control group (P < 0.05; Figure 1C).
The two groups had similar PSQI scores before nursing care (P > 0.05). PSQI scores were markedly reduced in both groups after nursing care. Moreover, the research group exhibited a more significant decrease in the PSQI score than the control group (P < 0.05; Figure 1D).
The number and percentage of difficulties in falling asleep for the first time, falling asleep again after waking up frequently at night, falling asleep again after waking up early, and falling asleep all night in the two groups were counted. The incidence of sleep disturbances was 8.14% in the research group, which was significantly lower than the 29.87% in the control group (P < 0.05; Table 3).
| Indicators | Research group (n = 86) | Control group (n = 77) | χ2 | P value |
| Difficulty in falling asleep for the first time | 3 (3.49) | 7 (9.09) | - | - |
| Difficulty in falling asleep again after waking up frequently at night | 2 (2.33) | 8 (10.39) | - | - |
| Difficulty in falling asleep again after waking up early | 2 (2.33) | 5 (6.49) | - | - |
| Difficulty in falling asleep all night | 0 (0.00) | 3 (3.90) | - | - |
| Total | 7 (8.14) | 23 (29.87) | 12.771 | < 0.001 |
By counting the number and percentage of cases of respiratory tract obstruction, catheter detachment, aspiration, and asphyxia, the adverse event rate in the research group (4.65%) was significantly lower than that in the control group (19.48%) (P < 0.05; Table 4).
| Indicators | Research group (n = 86) | Control group (n = 77) | χ2 | P value |
| Respiratory tract obstruction | 1 (1.16) | 4 (5.19) | - | - |
| Catheter detachment | 2 (2.33) | 4 (5.19) | - | - |
| Aspiration | 1 (1.16) | 5 (6.49) | - | - |
| Asphyxia | 0 (0.00) | 2 (2.60) | - | - |
| Total | 4 (4.65) | 15 (19.48) | 8.676 | 0.003 |
Surgery is undoubtedly a significant psychological and physiological stressor for older patients[13]. Typically, anxiety is evident in patients who are entering the operating room for major or minor surgeries, particularly those who are entering the operating room for the first time because they are often concerned about the possible detrimental effects of surgery on their health[14]. This intense sense of anxiety will not only affect the surgical process but may also adversely influence postoperative rehabilitation[15]. Many factors can cause perioperative anxiety in older patients, including the surgical procedure, anesthesia process, postoperative recovery, postoperative pain, and effect of surgery on physical function[16]. Therefore, to ensure a smooth recovery for patients after surgery, it is necessary to attach importance to and strengthen preoperative and postoperative nursing work[17].
In traditional preoperative visits, health education is often unilateral explanation by nurses without knowing whether patients understand and need these contents[18]. To improve this, a new comprehensive preoperative health education model was adopted[19]. The patient’s dedicated ward nurse will provide comprehensive and systematic preoperative education, including basic knowledge of surgery and anesthesia, and key points of perioperative care and postoperative recovery[20]. Unlike traditional methods, the current education approach encourages patients to take the initiative to raise questions, and professional health educators then provide detailed answers to ensure that the information is relevant to the actual needs of patients[21]. Preoperative patient education has been indicated to be the basic responsibility of any healthcare provider, and patients who receive detailed preoperative education have better extubation quality and improved quality of recovery from general anesthesia[22]. In the present study, the OT and time to complete regain of consciousness were significantly lower in the research group than in the control group after nursing, and the temperatures immediately after the procedure and upon recovery from anesthesia were significantly better. Thus, through comprehensive preoperative education, patients’ OT can be significantly shortened, they can regain pos
The application of preoperative comprehensive education for older patients who underwent surgery under general anesthesia can improve postoperative indicators, significantly reduce the occurrence of anxiety and depression, reduce postoperative pain, and improve the sleep quality of the patients.
| 1. | Lim BG, Lee IO. Anesthetic management of geriatric patients. Korean J Anesthesiol. 2020;73:8-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 2. | Bhushan S, Huang X, Duan Y, Xiao Z. The impact of regional versus general anesthesia on postoperative neurocognitive outcomes in elderly patients undergoing hip fracture surgery: A systematic review and meta-analysis. Int J Surg. 2022;105:106854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 48] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 3. | Ma J, Wang F, Wang J, Wang P, Dou X, Yao S, Lin Y. The Effect of Low-Dose Esketamine on Postoperative Neurocognitive Dysfunction in Elderly Patients Undergoing General Anesthesia for Gastrointestinal Tumors: A Randomized Controlled Trial. Drug Des Devel Ther. 2023;17:1945-1957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 32] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Li YW, Li HJ, Li HJ, Zhao BJ, Guo XY, Feng Y, Zuo MZ, Yu YP, Kong H, Zhao Y, Huang D, Deng CM, Hu XY, Liu PF, Li Y, An HY, Zhang HY, Wang MR, Wu YF, Wang DX, Sessler DI; Peking University Clinical Research Program Study Group. Delirium in Older Patients after Combined Epidural-General Anesthesia or General Anesthesia for Major Surgery: A Randomized Trial. Anesthesiology. 2021;135:218-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 5. | Xiao R, Zhao X, Qi Q, Zhang D, Zhang W, Wang G. Effect of Language Arousal Nursing Combined with Thermal Insulation Nursing on MAP, SPO2, NRS and Adverse Reactions in Elderly Patients Undergoing Spinal Fracture Surgery Under General Anesthesia. Altern Ther Health Med. 2023;29:764-769. [PubMed] |
| 6. | Phelps JR, Lizi H, Murphy BA. Anesthesia for Global General Thoracic Surgery. Thorac Surg Clin. 2022;32:307-315. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Chiu PL, Li H, Yap KY, Lam KC, Yip PR, Wong CL. Virtual Reality-Based Intervention to Reduce Preoperative Anxiety in Adults Undergoing Elective Surgery: A Randomized Clinical Trial. JAMA Netw Open. 2023;6:e2340588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 30] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 8. | Gao J, Zheng Q, Liu M, Bao J. Functional Magnetic Resonance Imaging of Brain Function and Emergence Agitation of Patients with Dexmedetomidine-Assisted General Anesthesia under Comfortable Nursing Intervention. Comput Intell Neurosci. 2022;2022:8527568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Soeters R, White PB, Murray-Weir M, Koltsov JCB, Alexiades MM, Ranawat AS; Hip and Knee Surgeons Writing Committee. Preoperative Physical Therapy Education Reduces Time to Meet Functional Milestones After Total Joint Arthroplasty. Clin Orthop Relat Res. 2018;476:40-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 10. | Tadesse B, Kumar P, Girma N, Anteneh S, Yimam W, Girma M. Preoperative Patient Education Practices and Predictors Among Nurses Working in East Amhara Comprehensive Specialized Hospitals, Ethiopia, 2022. J Multidiscip Healthc. 2023;16:237-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Zganjar A, Glavin K, Mann K, Dahlgren A, Thompson J, Wulff-Burchfield E, Winright S, Heim A, Wyre H, Lee E, Taylor J, Holzbeierlein J, Mirza M. Intensive preoperative ostomy education for the radical cystectomy patient. Urol Oncol. 2022;40:481-486. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Bang YJ, Kim S, Kim JK, Kim H, Kim S, Chung CS, Yoo SY, Jeong H, Park B, Lee SH. Effect of preoperative patient education and simulated mouth breathing training on opioid requirements in the post-anesthesia care unit after nasal surgery: a randomized controlled study. BMC Anesthesiol. 2023;23:348. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Lin HS, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16:157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 790] [Cited by in RCA: 720] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 14. | Celik F, Edipoglu IS. Evaluation of preoperative anxiety and fear of anesthesia using APAIS score. Eur J Med Res. 2018;23:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 113] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 15. | Richards SJG, Frizelle FA, Geddes JA, Eglinton TW, Hampton MB. Frailty in surgical patients. Int J Colorectal Dis. 2018;33:1657-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 16. | Adams PD, Ritz J, Kather R, Patton P, Jordan J, Mooney R, Horst HM, Rubinfeld I. The differential effects of surgical harm in elderly populations. Does the adage: "they tolerate the operation, but not the complications" hold true? Am J Surg. 2014;208:656-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Jones TS, Moore JT, Robinson TN. Perioperative Care Strategy for Older Adults. Med Clin North Am. 2020;104:895-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Bailes BK. Perioperative care of the elderly surgical patient. AORN J. 2000;72:186-207; quiz 218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | St-Louis E, Sudarshan M, Al-Habboubi M, El-Husseini Hassan M, Deckelbaum DL, Razek TS, Feldman LS, Khwaja K. The outcomes of the elderly in acute care general surgery. Eur J Trauma Emerg Surg. 2016;42:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 20. | Jurys T, Kupilas A, Rajwa P, Bryniarski P, Burzyński B. Role of preoperative patient education among prostate cancer patients treated by radical prostatectomy. Cent European J Urol. 2022;75:272-276. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Ko FC. Preoperative Frailty Evaluation: A Promising Risk-stratification Tool in Older Adults Undergoing General Surgery. Clin Ther. 2019;41:387-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 115] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 22. | Sameen Z, Talib K, Wani SQ, Ashraf M, Nengroo SH. Preoperative education improves the preparedness for extubation at emergence from general anaesthesia! J Perioper Pract. 2022;32:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Jovanovic K, Kalezic N, Sipetic Grujicic S, Zivaljevic V, Jovanovic M, Savic M, Trailovic R, Vjestica Mrdak M, Novovic M, Marinkovic J, Kukic B, Dimkic Tomic T, Cvetkovic S, Davidovic L. Patients' Fears and Perceptions Associated with Anesthesia. Medicina (Kaunas). 2022;58:1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Peng F, Peng T, Yang Q, Liu M, Chen G, Wang M. Preoperative communication with anesthetists via anesthesia service platform (ASP) helps alleviate patients' preoperative anxiety. Sci Rep. 2020;10:18708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Oshodi TO. The impact of preoperative education on postoperative pain. Part 2. Br J Nurs. 2007;16:790-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Sibley D, Sellers D, Randall I, Englesakis M, Culos-Reed SN, Singh M, Mina DS. Evaluating the effect of preoperative interventions on sleep health in the perioperative period: a systematic review. J Sleep Res. 2024;33:e14124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 27. | Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, Heim M, Houle T, Kurth T, Latronico N, Lee J, Meyer MJ, Peponis T, Talmor D, Velmahos GC, Waak K, Walz JM, Zafonte R, Eikermann M; International Early SOMS-guided Mobilization Research Initiative. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388:1377-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 473] [Article Influence: 52.6] [Reference Citation Analysis (0)] |