Copyright
©The Author(s) 2024.
World J Exp Med. Mar 20, 2024; 14(1): 86898
Published online Mar 20, 2024. doi: 10.5493/wjem.v14.i1.86898
Published online Mar 20, 2024. doi: 10.5493/wjem.v14.i1.86898
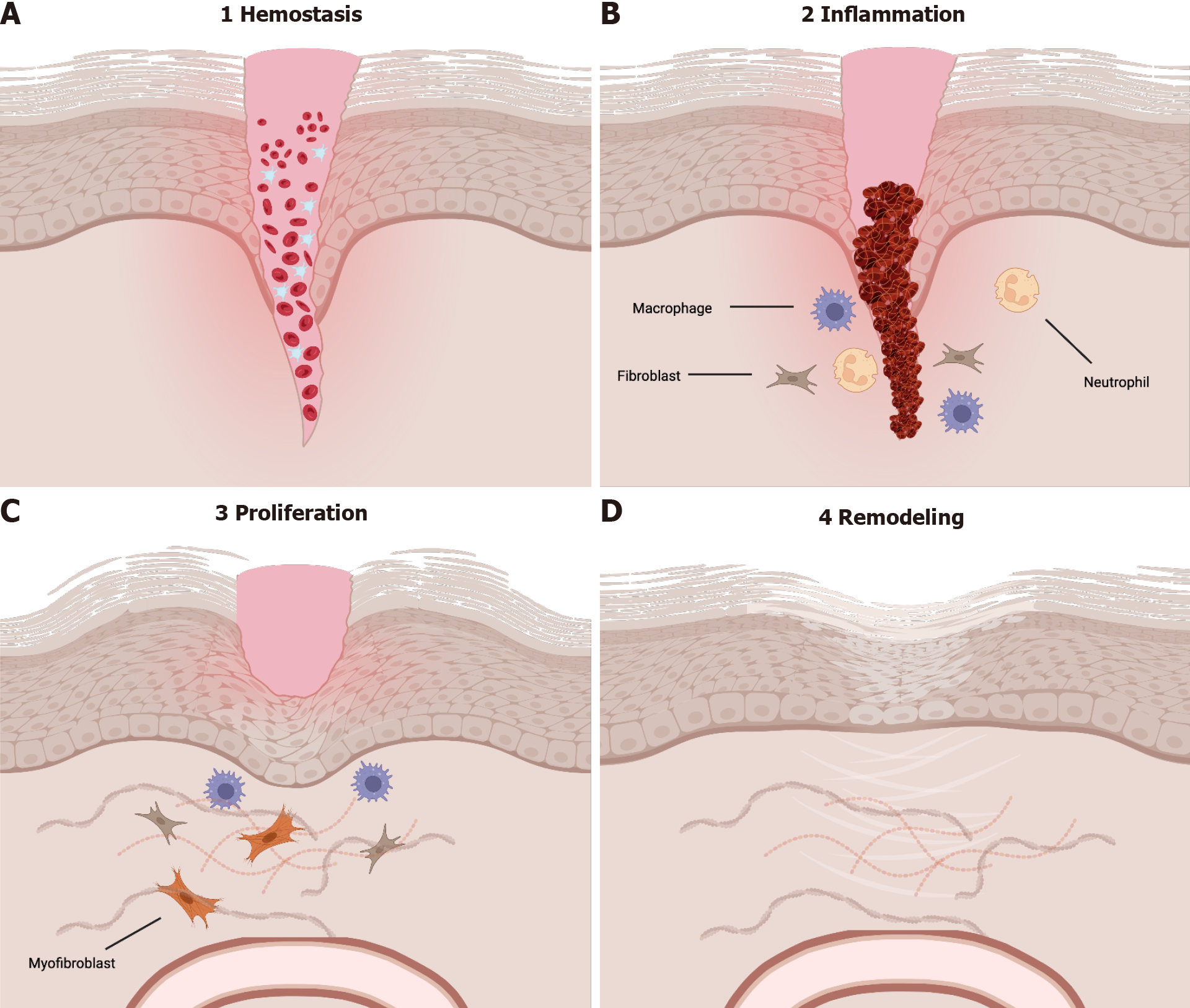
Figure 1 The four phases of wound healing.
Wound healing is divided into 4 distinct phases that have overlap. A: Hemostasis, B: Inflammation, C: Proliferation, D: Remodeling. Cell-to-cell interactions mediated by both cytokines and chemokines are imperative for the transitions between phases. During hemostasis, platelets and fibrin function to form a plug to stop bleeding. Hemostasis is followed by the inflammatory phase which is characterized by release of cytokines, most notably from macrophages, that are imperative for induction of the proliferative phase. During proliferation, the body is focused on neovascularization and re-epithelialization of the wound surface. The final phase, remodeling, takes place over months to years and is currently not well characterized. Produced using BioRender.com.
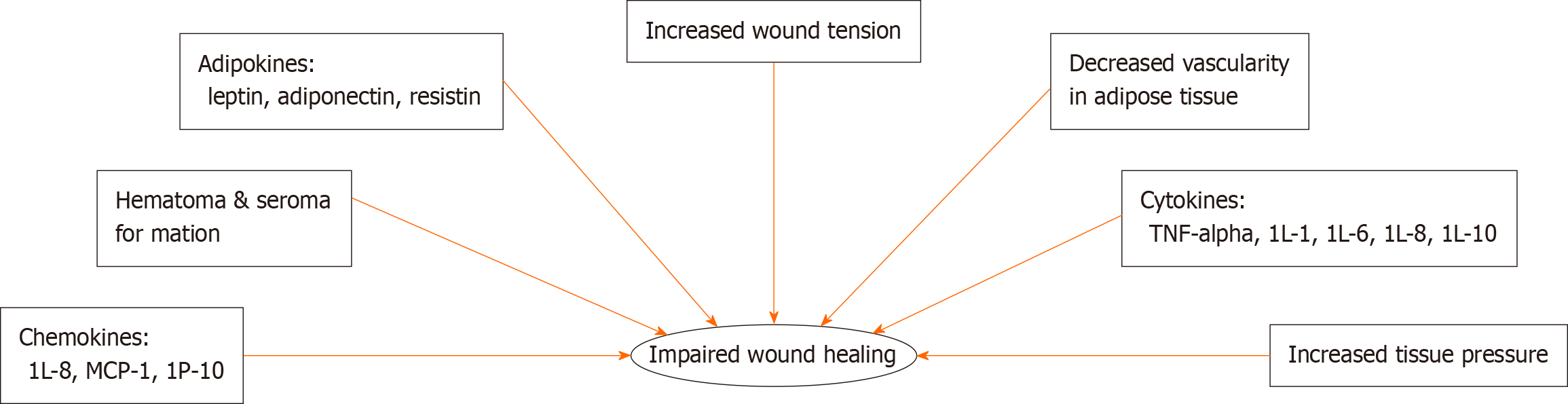
Figure 2 Factors related to wound healing impairment in obesity.
Obesity is characterized by a chronic inflammatory state that is associated with changes mediated by varying levels of adipokines, chemokines, and cytokines. In addition to these chemical signals, physiologic changes including increased tissue pressure and decreased vascularity of adipose tissue also contribute to poor wound healing outcomes. MCP-1: Monocyte chemoattractant protein-1; IP-10: Interferon-gamma-inducible protein 10; TNF-α: Tumor necrosis factor alpha; IL: Interleukin.
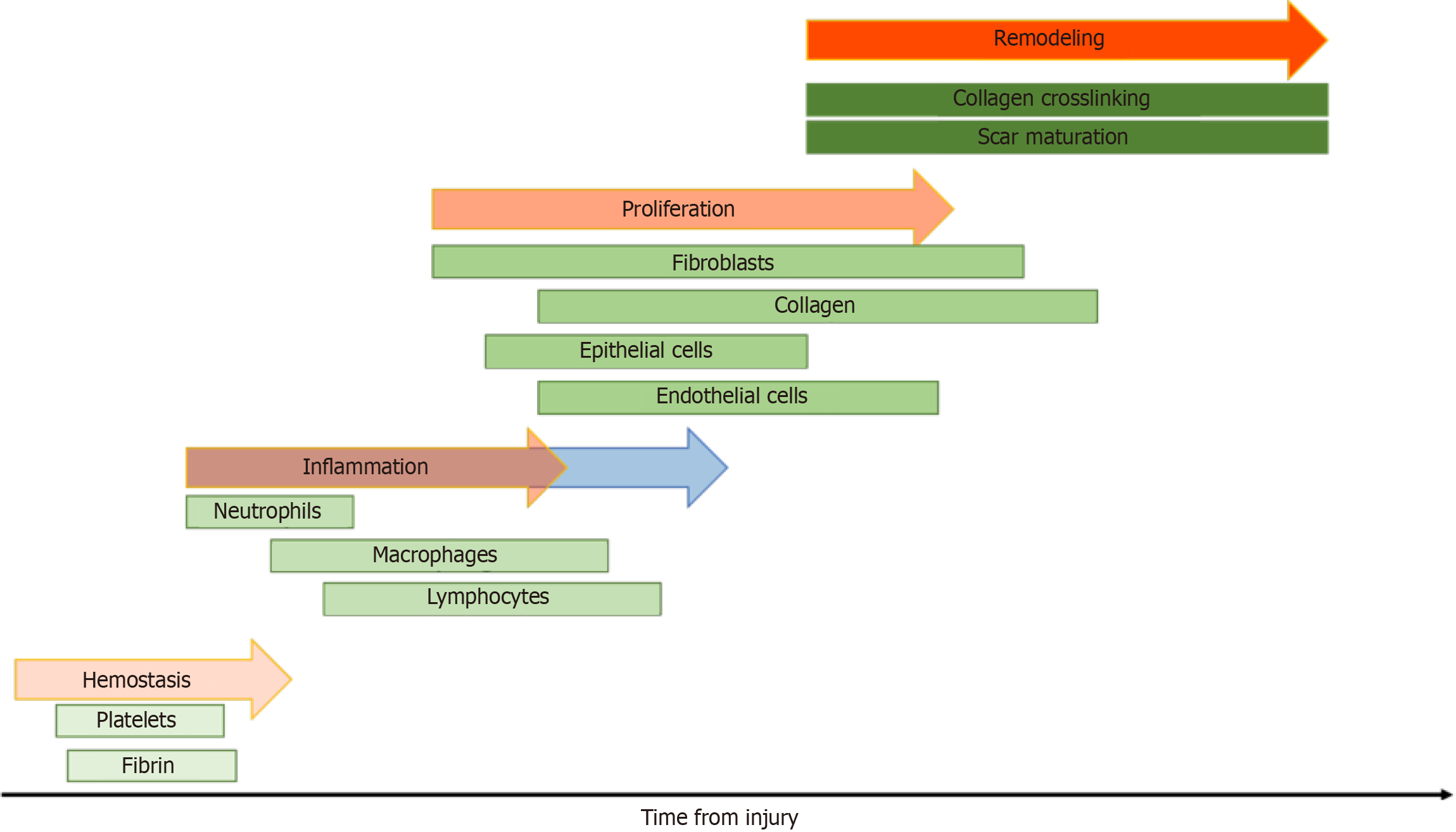
Figure 3 A timeline of the four phases of wound healing.
Each phase of wound healing is mediated by a distinct population of cells. While the phases have significant overlap, alterations in levels of cytokines or cell types in any phase may cause delayed wound healing. The inflammatory phase is notably extended in obese patients (blue arrow), this is thought to contribute to poor healing outcomes in this population.
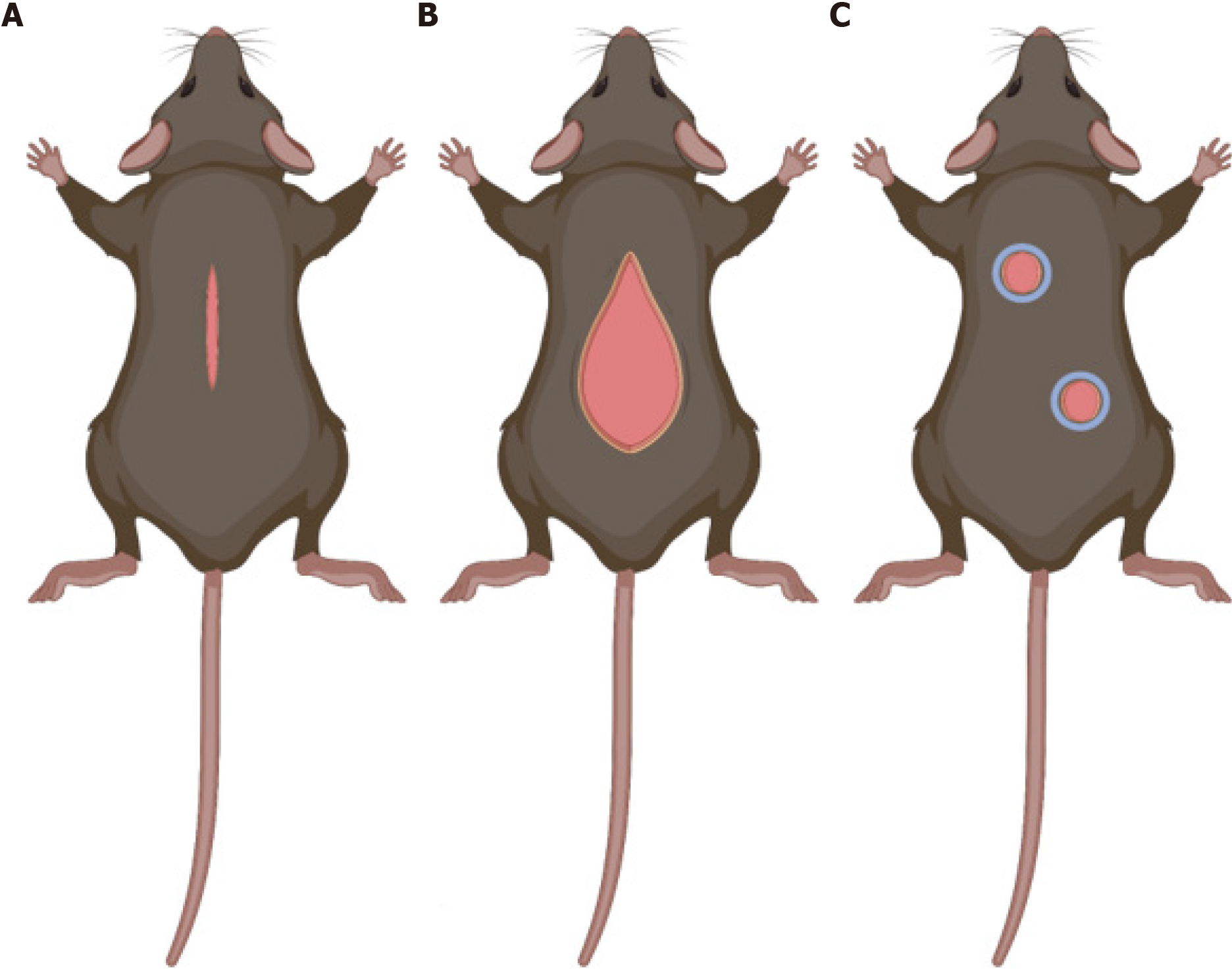
Figure 4 Schematic of three major models of wound healing.
A: Hypertrophic wound model. This model allows for use of a device to produce constant tension in the wound bed to produce healing with a hypertrophic scar similar to what is seen in areas of high tension on the body; B: Wound-induced hair follicle neogenesis model. This model is used to investigate regeneration in the setting of large full-thickness trauma; C: Excisional wound model. This model is the most commonly used model to study wound healing and is popular for its ability to investigate the role of various therapeutics to augment wound healing in a similar manner to what is seen in human skin. Produced using BioRender.com.
- Citation: Cotterell A, Griffin M, Downer MA, Parker JB, Wan D, Longaker MT. Understanding wound healing in obesity. World J Exp Med 2024; 14(1): 86898
- URL: https://www.wjgnet.com/2220-315x/full/v14/i1/86898.htm
- DOI: https://dx.doi.org/10.5493/wjem.v14.i1.86898