INTRODUCTION
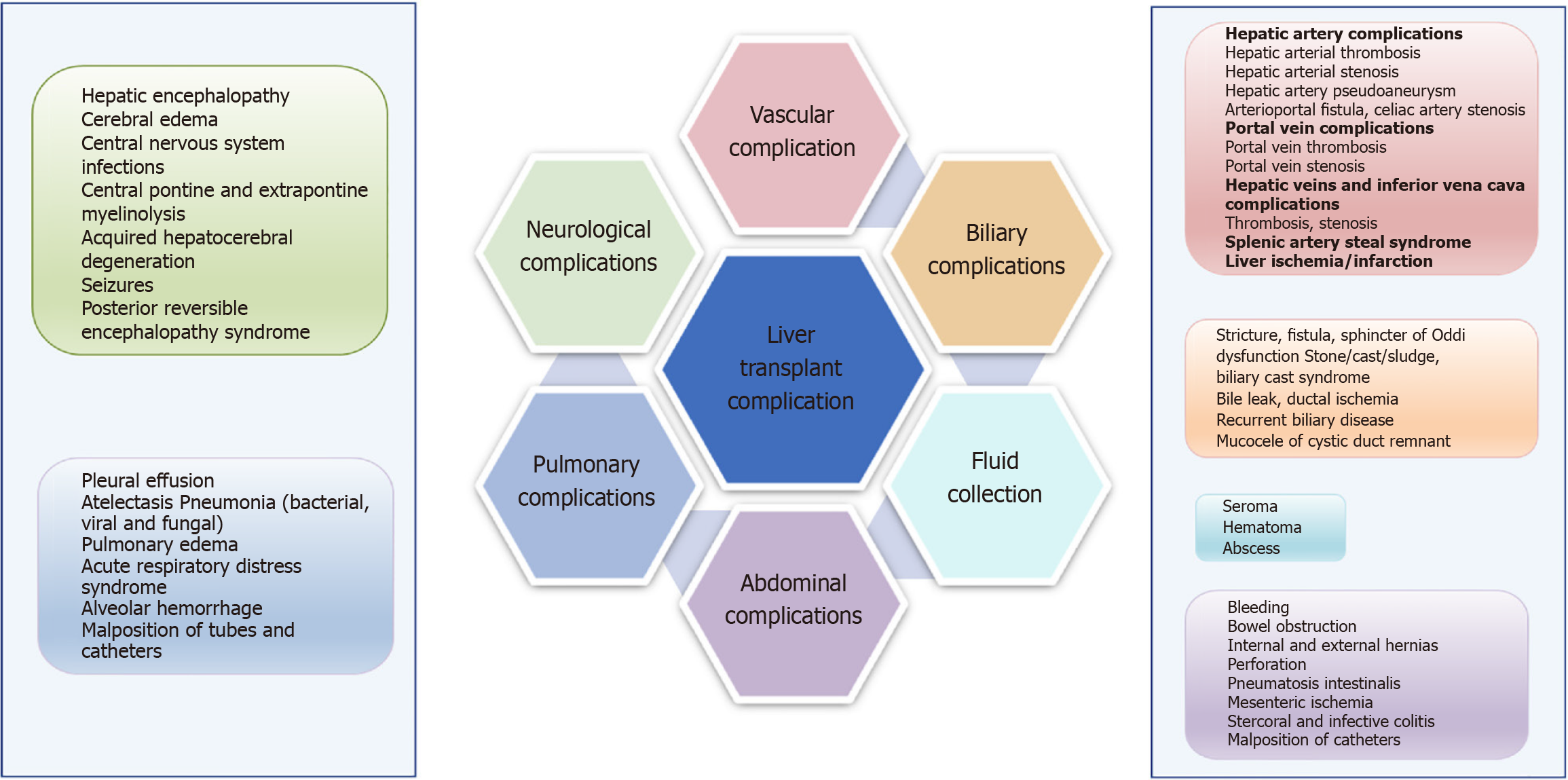
Orthotopic liver transplantation (OLT) is an essential and only curative therapy for patients with end stage liver disease. It is a globally accepted therapeutic option for liver tumors at primary stage and acute liver failure[1]. The first liver transplant surgery was performed by Starzl et al[2]in the year 1967, wherein whole donor liver from a deceased donor replaced the resected liver. Advancements in surgical techniques, improved anaesthesiological approaches and post-operative care have increased the one year survival rate to 80%-90%. Improved immunosuppressive regimens also give a better long term survival[3]. However, despite of these advancements in operative procedures and post-operative care, morbidity and mortality are very common post OLT[1]. Thus, liver transplant patients require a close medical care, both immediate post operative and long term care. Common medical complications in such patients include renal dysfunction, neurological complications, arterial hypertension and even psychiatric complications[4]. Biliary complications which affect approximately one fourth of liver recipients include anastomotic and non-anastomotic biliary strictures, bile duct stones, leaks etc. (Figure 1)[1]. In adult transplants, most common complications are stenosis and strictures after OLT[5]. Early morbidity and mortality in liver transplant patients also occur due to infectious or non-infectious pulmonary complications such as pleural effusion, pulmonary edema, atelectasis, pneumonia and respiratory distress syndrome (Figure 1)[6].
Figure 1 Schematic representation of various Postoperative complications after liver transplantation.
As the liver transplant surgery includes dissection and removal of native liver under deranged coagulation conditions, portal hypertension and diffusion of collateral venous flow, it is often associated with bleeding complications and side effects of blood transfusion[7]. However, with modern surgical devices and skills and treatment of coagulation abnormalities, blood losses are minimized. Compared to bleeding complications, thrombotic events are less frequent post OLT, however, special emphasis must be given to them as they pose a major risk to both, the patient and the graft survival. In fact, some liver recipients may pose substantial risk of thrombotic complications[8], hence it becomes utmost important to have a better and clear understanding of re-balanced haemostatic system.
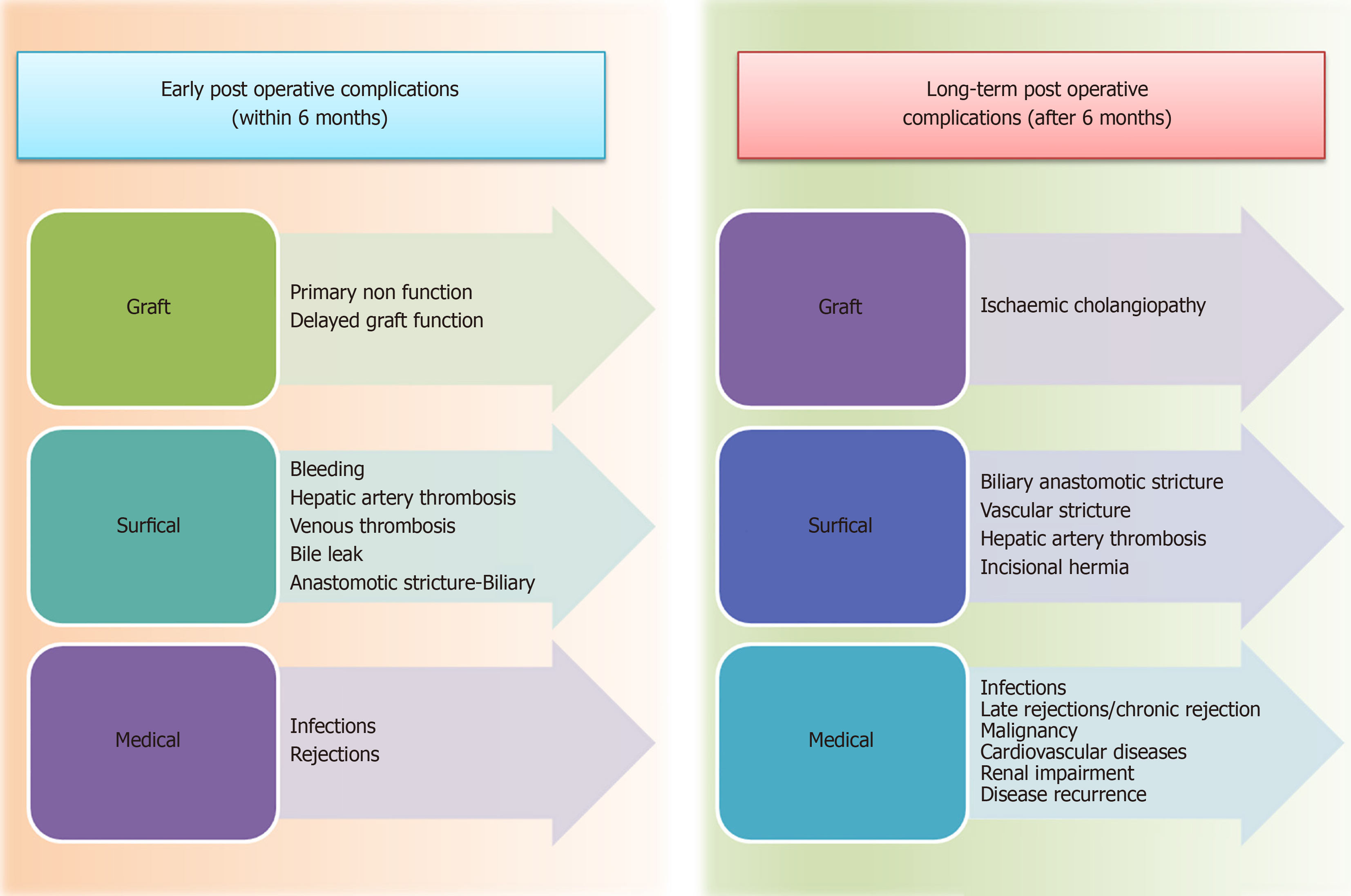
Post-transplant thrombosis may occur at an early stage or after several months of OLT procedure, however, in both cases, the complications are potentially life threatening and reduce the chances of graft and patient survival to a significant extent (Figure 2)[9]. Thrombotic studies are estimated to occur in approximately 26% of liver transplant surgeries, as estimated by cohort studies on pediatric and adult transplant data[10]. Incidences of vascular complications (VCs) is highly variable amongst the liver transplant patients, however these incidences result in higher rates of graft failure and mortality. VCs not only deteriorates graft but also significantly affects patient survival[11]. Clinical presentation of VCs depends on its type, thrombosis or stenosis and its timing of occurrence after transplantation. Prompt diagnosis is always beneficial in such cases[12,13]. Thus, all vascular problems, although occur seldom, need special attention as they might lead to dreadful complications. VCs are most commonly monitored using doppler ultrasonography and magnetic resonance imaging (MRI) angiography for the diagnosis of early postoperative arterial stenosis and thrombosis[7].
Figure 2 Medical complications during follow up period after liver transplantation.
Early diagnosis and advances in treatment of thrombosis can spare the re-transplantation. Other treatment options such as revascularization procedures are successful only if the thrombosis is diagnosed in initial stages, within few hours of development[14,15]. Possible outcome of post-operative thrombosis are more serious than postoperative hemorrhaging and include graft dysfunction and damage to other critical organs. It is extremely difficult to establish strict surveillance for every patient undergoing transplantation. Thus the awareness about risk factors for thrombosis and effective treatment strategies can guide clinicians for better management of patients post OLT. However, most of the institutions nowadays, follow strict and continuous point-of-care intraoperative and perioperative monitoring of haemostatic problems. This has actually helped in replacing traditional attempts to prophylactically reverse perioperative blood coagulation issues[7]. This article aims to review the various clinical forms of thrombotic complications which can occur after liver transplantation (LT) and risk factors associated with them.
EARLY AND LONG TERM POST OPERATIVE OLT COMPLICATIONS
Despite significant improvisation in surgical techniques, VCs with varying incidences in children and adult, leads to failure of LT. In serious cases, re-transplantation is the only option, however, it involves high risk of patient mortality and availability of graft is also a limiting factor is such cases[16]. Different imaging modalities play a significant role in monitoring post operative liver transplant patients to assess their early and late complications. Thrombotic events occurring in perioperative period include intracardiac thrombosis (ICT), portal vein thrombosis (PVT), deep vein thrombosis and pulmonary emboli[7]. Their prognosis is dependent upon early diagnosis and treatment. Thus, post OLT management is extremely important to increase graft and patients survival[17,18]. Clinical presentations of post OLT complications may show overlapping thus making it difficult to assure prompt treatment and graft survival[18,19]. In such cases, state of the art imaging techniques such as Doppler ultrasonography (USG) followed by computed tomography (CT) angiography, multidetector CT, MRI or procedures of cholangiography are used for accurate diagnosis. Various complications may occur within few hours after OLT mainly due to graft characteristics, intra-operative instability and pre-operative clinical status of recipient[20].
THROMBOTIC RISK POST LIVER TRANSPLANT
OLT is associated with several arterial and venous complications. There is a possible cohesion of intrinsic hypercoagulative state with transplant procedure, which may pose a life threat to the patient[7]. Majority of mortality and morbidity are due to arterial complications whereas venous complications are less frequent[21]. Onset of thromboembolism is unpredictable, which may be triggered by various factors acquired post transplant procedure such as inflammation, venous stasis, ischemia-reperfusion injury, vascular clamping along with inherited (genetic) risk factors such as increased activity of coagulation factors and deficiency of profibrinolytic activity[7]. Lowered fibrinolysis along with abnormal thrombin generation and activated platelet function may trigger a hypercoagulable state. Imbalance of pro-coagulants and anti-coagulants and various other factors inherent to the procedure of LT may promote a prothrombic milieu[8]. Thrombotic risks related to transplantation procedure include surgical damage, stasis of blood, activation of coagulation factors and release of activators from donor liver[7].
Uninterrupted and adequate inflow and outflow of blood is one of the most critical factors for a successful LT surgery. However, LT surgery is often affected by serious VCs such as PVT and hepatic artery thrombosis (HAT). This post transplant VCs increases mortality rates significantly[22,23]. Amongst the two, PVT is a rarer complication with incidence rate of approximately 3% to 7% in LT patients[24], however, it is more detrimental than HAT because it is difficult to establish alternative portal inflow[25]. HAT and PVT together contributes to approximately 16% of graft failure[26-28].
ARTERIAL COMPLICATIONS POST OLT
Arterial complications are one of the major causes of morbidity and mortality after OLT. Pivotal role is played by hepatic artery (HA) as it supplies blood or both the liver parenchyma and the biliary tree. Two most common arterial complications related to liver transplant are HAT and HA stricture (HAS), as these contribute to maximum morbidity and mortality in liver transplant patients[29].
HAT
HAT is an important cause for graft loss as well as ischemic biliary complications. HAT is basically occlusion of the HA that may occur within 30 days of liver transplant (early HAT) or after 30 days of liver transplant (late HAT)[30,31]. It is one of the most frequent of all arterial complications. HAT is most commonly associated with higher incidences (more than 50%) of liver transplant failure, resulting in high mortality rates in the absence of revascularization or re-transplantation. The incidences of HAT widely ranges from 0%-12%[22,32,33], however its true incidence rate post OLT is unknown.
HAT usually occurs due to surgical techniques such as kinking, stenotic anastomosis, however many studies have shown occurrence of eHAT because of non-surgical factors such as age of donor[32], sluggish flow through HA[34-36] and rejection. HA supplies blood to the bile ducts exclusively. In case of HAT, biliary ishemic lesions, necrosis along with biliary leakage is common, resulting in graft dysfunction. HAT also presents ischemic strictures(s) and ultimately multiorgan failure[31].
HAT needs an early detection and treatment before there is irreversible graft dysfunction. This can be done by routine monitoring of HA anastomoses with doppler USG. Thus appropriate therapeutic strategies other than re-transplantation can be employed[27]. Although re-transplantation remains the last hope for severe HAT patients, it is dependent upon the availability of graft. More therapeutic options include arterial reconstruction, radiologically guided thrombolysis and surgical thrombectomy[27].
Intraoperative HAT: Complication of acute HAT is more common in pediatric OLT cases than adults due to their narrower vessel diameters[37]. The development of Intraoperative HAT could be abrupt due to mechanical factors such as internal flaps, prolonged clamping of HA during the procedure, intra-arterial haematoma and knicking of long artery[37].
Early post operative HAT: Incidences of HAT are reportedly higher in children (15%-20%) compared to adults (2.56%)[37]. However, overall mortality rates are higher in adults (34.3%) compared to children (25%)[31]. Overall re-transplantation rate in case of early HAT has been reported as 53.1% which was 62% in Children compared to 50% in adults[31]. In most cases, the real causes of early post operative HAT (eHAT) remains unknown. Apart from surgical causes such as kinking, stenotic and anastomosis, several non-surgical causes have also been linked to eHAT[32]. Rejection and sluggish artery flow are some of the other reasons for eHAT[35,36].
HAS
HAS refers to narrowing of the transverse diameter of the HA resulting in graft ischemia. It is often asymptomatic and is indicated by abnormal liver function tests[38,39]. Incidences of HA occurs in occurs in 2% to 13% of transplants[38-40]. The chances of developing biliary complications are lesser during HAS compared to HAT. HA stenosis may progress to thrombosis if not treated on time and leads to additional biliary stricture and graft dysfunction.
HA pseudoaneurysm
HA dilates during HA flow after iatrogenic injury causing leakage of blood in the surrounding tissue outside the artery wall. The incidences of HA pseudoaneurysm (HAP) are rarely reported, approximately 0.27%-3%[41-44]. Clinical representation of HAP could range from asymptomatic to abdominal pain, fever, gastrointestinal bleeding through the abdominal drain and hemorrhagic shock[45]. HAP is reportedly associated with peritoneal infection, arterial anastomosis difficulties and biliary leak and occurs within few months of transplantation procedure[41,45,46]. Its contributing factors include local infection due to immunosuppression, biliary tract infections, biloma etc.[46,47]. Management of uncomplicated pseudoaneurysms is possible through various approaches including percutaneous approaches, however in most cases, HA pseudoaneurysms are unrecognized before rupture. Surgery is the option in such cases. Other successful endovascular treatment strategies include coil embolization, stent and stent-graft[48,49].
HA rupture
HA rupture (HAR) refers to severe hemorrhage from the trunk or from a main branch of the HA. Arterial blood supply is disrupted during HAR. It is a rare complication but has very high mortality rates[46,50]. HAR usually occurs as a result of pseudoaneurysm of the HA causing massive bleeding. Rupture may occur freely into the peritoneum, the gastrointestinal tract, or the biliary tract. It requires immediate surgery. Mortality rate due to HAR is as high as 78%[46,47]. Boleslawski et al[50] compared different management techniques for HA rupture and found that HA ligation results in better survival rates and hence it is a reasonably good option for initial management for HAR and also concluded that re-transplantation was not always necessary in such cases.
HA stenosis
This condition can predispose a person towards thrombosis after LT. It has an incidence rate of 5% to 11% in adults post OLT[29,51,52]. Though most of the patients do not show any symptoms, untreated HAS reportedly cause thrombosis in 65% of patients[53]. Several therapeutic options are available for treatment of HA stenosis (HAS), such as conservative anticoagulation treatment to more massive surgical revascularization and re-transplantation[38,54]. Endovascular interventions such as dilation with a balloon, angioplasty or stent are most commonly used for treatment of HAS[29]. Surgical revascularization or re-transplantation can be avoided using these endovascular treatment strategies.
VENOUS COMPLICATIONS POST OLT
Venous complications post LT are less frequent compared to overall arterial complications[55,56], however these can lead to serious complications leading to graft failure and mortality after OLT procedure, especially if the venous complication occurs at an early stage after the procedure[57,58]. Also, several studies have suggested that the incidences of venous thrombosis during OLT are more frequent in pediatric cases compare to adult transplants[59,60].
PVT
Incidence rate of PVT in LT recipients ranges from 4.9% to 10.6%, with highest rates reported in pediatric transplants[61,62]. Preoperative PVT is frequently associated with liver cirrhosis and liver cancer and this further increases risk of postoperative PVT. Portal hypertension, allograft loss, and mortality are the known complications of PVT[63]. Treatment of PVT after LT is complicated, as it is difficult to establish an alternative blood flow. Jensen and co-workers demonstrated that portal vein (PV) flow is restored in higher number of patients with early PVT (60%) compare to patients with late PVT which had lower white blood cells and platelet count and an elevated international normalized ratio (INR) as well as gastrointestinal bleeding[63].
PV stenosis
Occurrence of PV stenosis (PVS) might be associated with graft failure or the complication of portal hypertension[64]. Actual incidences of PVS are not reported. Signs of portal hypertension such as gastrointestinal tract bleeding may occur in patients with PVS, whereas majority of the patients are asymptomatic. Also, PVS is not always accompanied by abnormal liver function tests[58]. In most cases PVS occurs as a result of surgical errors[58]. In a recent study of postoperative PV complications after LT, it was found that PV complications occurred in 53 (9.3%) patients including 46 recipients with PVS and 7 with PVT[65]. Various methods of portal venography such as percutaneous transhepatic, transjugular intrahepatic or transfemoral venous approaches are reported for treatment of PV stenosis. Stent placement is also a widely accepted management strategy for treating venous obstructions after OLT.
Post liver transplant DVT and inferior vena cava thrombosis
Deep vein thrombosis (DVT) occurs rarely post OLT. Accurate detection of venous thrombosis is mostly done using doppler ultrasound. Major risk factors leading to DVT after transplant procedure include hypercoagulated state as a result of surgery, venous stasis occurring due to prolonged immobilization after surgery, pro-coagulant administration and prolonged indwelling femoral vein catheters[66]. Reported incidences of DVT post transplant ranges from 3.5% and 8.6% in literature[66,67]. Defects in anti-coagulation protein synthesis can be transmitted from donors to recipients through liver grafts. These include protein C (PROC) or protein S (PROS1) deficiency, inherited anti-thrombin and factor II G20210A mutation[68,69].
In high risk patients or those with upper and lower extremity DVT, low molecular weight heparin (LMWH) is prescribed followed by oral anti-coagulants in therapeutic doses.
ICT and pulmonary embolism
Both ICT and pulmonary embolism (PE) are serious complications that may result in mortality during adult LT procedure. The incidence rates of these complications are relatively low, ranging from 1.2% to 6.2%[70]. Out of nearly 3000 OLT procedures performed from 1982 till 2007, PE was reported in only 36 patients (0.37% incidence rate[71]), whereas Sakai et al[70] later showed incidence rate of PE was 4%. Actual incidence rates of PE and ICT could have been much higher with frequent use of intraoperative transoesophageal echocardiography, which could have helped in better identification of these sudden and serious haemodynamic changes[7].
Onset of PE and ICT may occur within few minutes after graft re-perfusion[72]. It has been reported that 30% of PE and ICT cases occur during pre-anhepatic phase whereas more than 30% cases occur during anhepatic and reperfusion phase of OLT procedure[73].
Hepatic vein thrombosis, also known as Budd-Chiari syndrome
Stenosis or thrombosis of the inferior vena cava or hepatic vein leads to hepatic vein thrombosis (HVT). Incidents of HVT are rare, however they can suddenly interrupt hepatic blood supply causing graft loss. Its therapeutic strategies mostly include surgical revascularization, percutaneous thrombolysis, percutaneous angioplasty or re-transplantation[21]. Its symptoms include abdominal swelling, intense pain and vomiting containing blood. Hepatic outflow obstruction is often treated by heparin when it is partial, however, surgical thrombectomy supported by extracorporeal circulation might be required to salvage the graft.
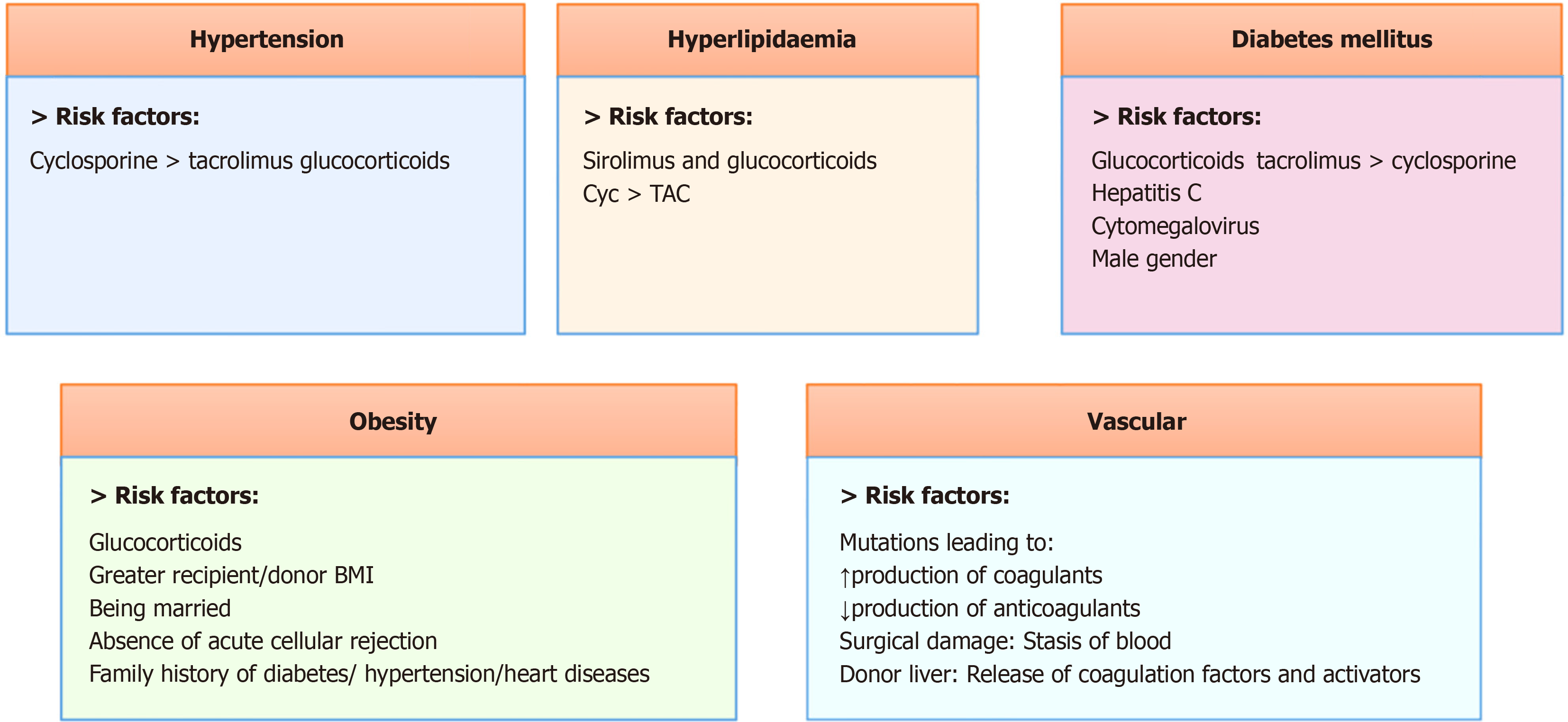
RISK FACTORS FOR CARDIO VCS POST LT
Cardiovascular complications are the leading causes of death post OLT, particularly in severely ill patients[74,75]. Cardiovascular diseases causes early mortality after LT in 40% cases followed by 28% due to infection and 12% due to graft failure, as demonstrated by large national cohort study of organ procurement and transplantation network database[76]. A number of patients undergo LT for non-alcoholic fatty liver disease and alcoholic liver disease[77]. Such patients are often associated with cardiovascular risk factors such as hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, prior cardiovascular disease etc. (Figure 3). These chronic complications might take several years to resurface.
Figure 3 Risk factors for Cardiovascular Complications after liver transplantation.
Cyc: Cyclophosphamide; TAC: Total antioxidant capacity; BMI: Body mass index.
Risk factors for post operative thrombosis has been well defined however, genetic risk factors for the same have not been elucidated[78]. Few genetic association studies have identified the role of genetic variants in increased risk for venous thromboembolism. Following OLT procedure, recipient may get inherited thrombotic risk factors from the donor. In such cases, recipient hypercoagulability with additional acquired risk factors from donor graft may increase the risk for thrombotic event post transplant[79,80]. Genetic association of single nucleotide polymorphisms in pro-thrombotic genes and coagulation factors such as factor V Leiden, factor II Leiden, fibrinogen gamma polypeptide, ABO, F11, Syntaxin Binding Protein 5, Stabilin-2, factor VIII Leiden as well as natural anti-coagulant genes such as PROC, PROC receptor, PROS1 etc. with increased risk of venous thromboembolism has been well established in literature[81-83]. These reports raise concern regarding genetic role in thrombotic incidences post OLT.
In a recent study by Li et al[84], genome wide association study was carried out in 775 donors for adult recipients and 310 donors for pediatric recipients along with meta-analysis of 1085 LTs to establish association between known donor thrombophilia gene variants and recipient post-transplant thrombosis. They identified 280 variants in 55 Loci at suggestive genetic significance threshold and plausible candidate genes such as adenylate kinase 4 (rs11208611-T) encoding a protein that regulates cellular adenosine triphosphate levels and G-protein signaling 5 (rs10917696-C) involved in vascular development, to be associated with increased risk of thrombosis post OLT[84]. This study provided common genetic variants in donors (not previously associated with thrombophilia) to be significantly associated with thrombotic risk post OLT. Due to lack of genome wide studies in OLT patients, true contribution of genetic risk factors in development of thrombotic complications after LT is unknown.
IMPACT OF THROMBOSIS AND ITS OUTCOME IN LIVER TRANSPLANT PATIENTS
Post operative complications of LT surgery include to contradictory states, including bleeding complications and thrombosis. Although, thrombotic events occur less frequently compared to bleeding complications, they pose significant risk to patients and graft survival. Etiology of thrombosis post OLT is complex and unpredictable. Serious complications like HAT and PVT are not uncommon after LT surgery and have detrimental effects. Pro-coagulant generation, thrombin production and platelet hyper-reactivity, post OLT leads to re-balanced hemostasis[85]. There are no specific guidelines which recommend thromboprophylaxis in LT. Factors which contribute to increased risk of thrombosis post LT include antiphospholipid syndrome, elevated serum homocysteine and acquired or congenital thrombophilia, however, in such cases also, prophylactic treatment is not recommended[86-88].
TIMELINE FOR THROMBOTIC EVENTS POST OLT
Thrombotic complications can occur during or after OLT. Thrombus formation is primarily associated with increased levels of platelet-adhesive protein von Willebrand factor and low levels of its regulatory factor ADAMTS13. Secondary causes of thrombus formation include increased potential to generate thrombin and reduced fibrinolysis[89]. Long term surveillance of LT patients suggests that peripheral thrombosis can cause complex haemostatic abnormalities leading to increased mortality and morbidity[88]. There are no specific guidelines for treatment of DVT during long term surveillance after OLT. LT recipients may have abnormal haemostatic function even after 1 year of transplant, which has been attributed to endothelial cell activation. Post transplantation thrombotic complications are often treated with LMWHs and oral anti-coagulants[89]. However, safety and efficacy of these drugs needs to be evaluated in future trials.
MANAGEMENT OF VCS POST OLT
Management of VCs is essential for maintaining normal liver functions. Due to the risk of bleeding, anti-thrombotic prophylaxis is not routinely prescribed during OLT post operative period. Furthermore, intra-operative release of tissue factor depends on surgical technique and other skills which is an important contributing factor for vascular thrombosis post OLT. Treatment strategies depend on clinical manifestations. Therapeutic options range from heparin based systemic anti-coagulation treatment to surgical thrombectomy, percutaneous transhepatic catheter-based thrombolysis, portosystemic shunts and even re-transplantation[90-92]. However, optimal treatment depends upon case to case basis. Anti-coagulation treatment option mostly includes LMWH initially, followed by vitamin K antagonists for long term treatment. More recently, interventional radiological techniques are being employed as alternatives to surgical thrombectomy or re-transplantation for thrombosis management post OLT, because of their reduced invasiveness and high success rates. Interventions for treatment of PV obstruction after pediatric LT include stent placement, mesorex bypass, percutaneous transluminal angioplasty and endovascular re-canalization[93]. Most frequently chosen options for management of thrombosis post OLT are interventional radiotherapy combined with systematic anticoagulation and transluminal angioplasty combined with thrombolysis and stent placement[93]. Patients under long term immunosuppressive therapy after LT are often treated with direct oral anti-coagulants (DOACs) such as rivaroxaban, apixaban and edoxaban. However, safety and efficacy of these DOACs is not well defined. In a recent study, mean immunosuppressive trough levels after DOACs treatment increased to 18.8% ± 29.6% in transplant patients compared to 3.0% ± 16.5% in matched controls without significant dose adjustments. Researchers further observed that there was no significant change in liver function and no transplant rejection in these patients[94]. Thus DOACs treatment for thrombosis post OLT is a safe option however, immunosuppressive trough levels should be monitored in such patients at regular intervals. Post operative use of anti-coagulants and anti-platelet therapy is restricted due to the risk of bleeding complications. Dose and duration of anti-coagulant treatment depends upon patient’s condition and risk of recurrent thrombosis[23]. Pre and post LT thrombotic management and choice of treatment strategy depends upon the phenotype of the liver disease and individual risk factors. Prospective studies with larger cohort should be conducted to formulate the guidelines for effective treatment strategies in this regard.
Advancements in the field of interventional radiology (IR) have enabled treatment of vascular and non VCs and also helps in improving graft and patient survival. Recent studies have demonstrated that IR treatment is effective for hepatic vein occlusion, PV stenosis, HAS, and anastomotic biliary stricture after LT procedure[95]. IR is a minimally invasive and safe treatment technique and hence IR team is an important part of multidisciplinary approach for care of LT patients[95].
IMPLICATIONS OF PRO-THROMBOTIC WORK UP PRE AND POST OLT
LT patients need a regular monitoring of their hemostatic status. Patients with provoking risk factors, previous or familial history of blood clots are at higher risk of developing thrombosis post surgery. Regular monitoring of various clotting biomarkers (thrombotic profile) reduces the likelihood of venous blood clots pre and post OLT. Standard indicators of patient’s coagulation status are coagulation tests. These include prothrombin time, activated partial thromboplastin time and INR. These tests provide a measure of measure of procoagulant factors, however, they do not provide any information on plasma levels of anti-coagulants[85]. Thus these tests alone cannot predict the risk of bleeding or thrombosis. Thrombin generation test (TGT) is a promising mechanism for investigating hemorrhagic coagulopathies, predicting the risk of recurrent VTE after a first event, and monitoring patients on oral anticoagulants[96]. TGT also measures the lag time, time to peak and also the endogenous thrombin potential[97]. Clinicians may take a call on the thromboprophylaxis option based on the assessment of prothrombotic status and patient’s individual risk factors.
CONCLUSION
Thrombotic complications post LT are frequent, which results in high rate of morbidity and mortality. Conventional coagulation tests do not provide accurate information about the blood clot dynamics. At present, no specific guidelines are available for management of thrombosis after LT. Thus, to minimize the risk of graft failure and mortality due to thrombosis, strict monitoring of patients post OLT is recommended. Clinicians should adopt rapid diagnostic techniques to predict VCs in patients post OLT.
ACKNOWLEDGEMENTS
Authors are extremely grateful to Director Defence Institute of Physiology and Allied Sciences, for his constant guidance and logistic support.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Transplantation
Country of origin: India
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Lindner C S-Editor: Luo ML L-Editor: A P-Editor: Zhao YQ