Copyright
©The Author(s) 2025.
World J Crit Care Med. Jun 9, 2025; 14(2): 101708
Published online Jun 9, 2025. doi: 10.5492/wjccm.v14.i2.101708
Published online Jun 9, 2025. doi: 10.5492/wjccm.v14.i2.101708
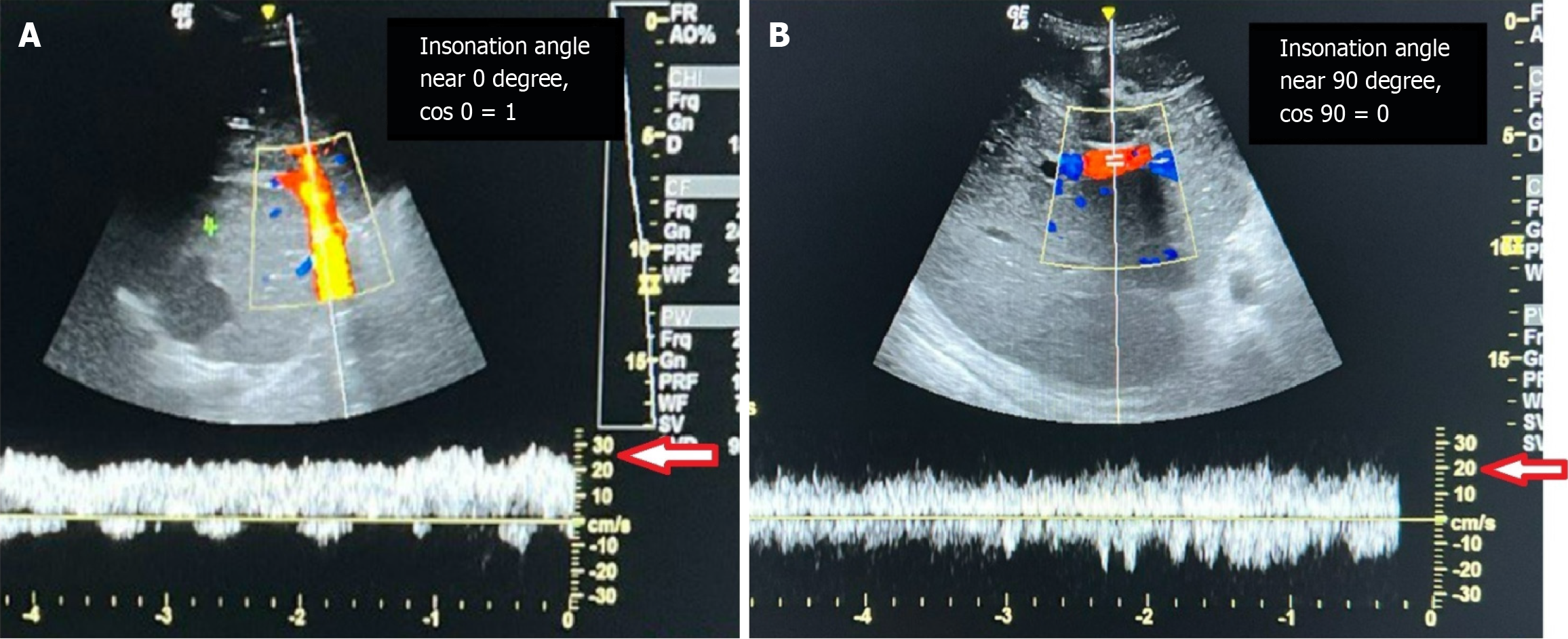
Figure 1 The influence of the insonation angle of the pulse wave spectral Doppler on the flow velocity measurement of the portal vein.
A: The left-hand side image showed an insonation angle of near 0 degrees; B: The right-hand side image showed an insonation angle of near 90 degrees for the portal vein of the same patient in the same setting. We underestimated the actual velocity of the portal vein blood flow from about 30 cm/s to roughly 20 cm/s when the insonation angle is near 90 degrees.
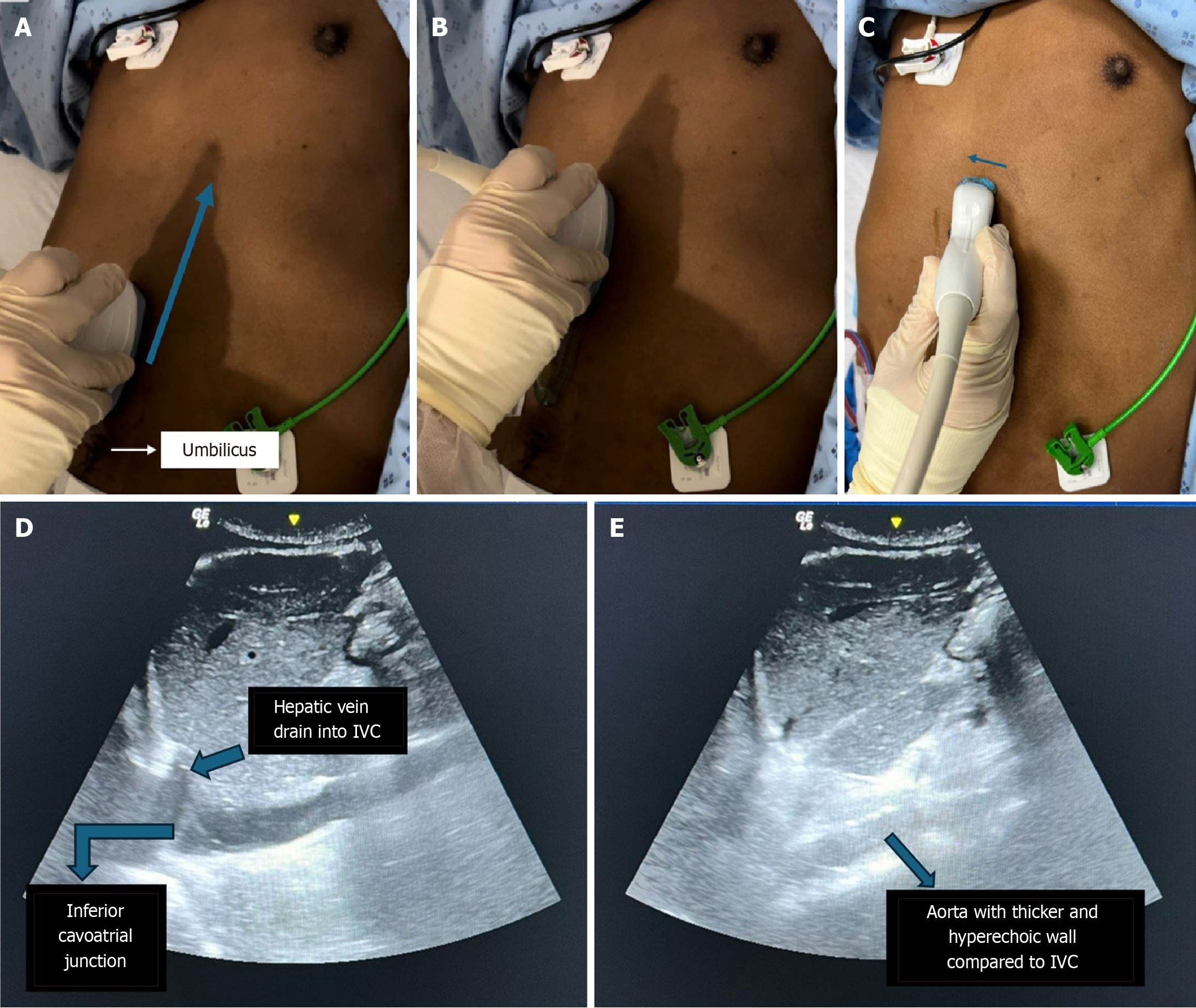
Figure 2 Measures for locating the inferior vena cava using a curvilinear probe.
A: Firstly, place the curvilinear probe near the umbilicus, then slide it cephalad, with the indicator pointing towards the patient's head; B: Once probe reaching subxiphoid area, you should be able to visualize the liver; C: Tilt the probe slightly towards the patient’s right, and the inferior vena cava (IVC) will be seen; D: Locate the anatomical landmarks of the inferior cavoatrial junction and the hepatic vein draining into the IVC to confirm the identification of the IVC; E: To check that the IVC is identified correctly, tilt the probe slightly to the patient’s left, and an aorta with a thicker and more hyperechoic wall will be seen.
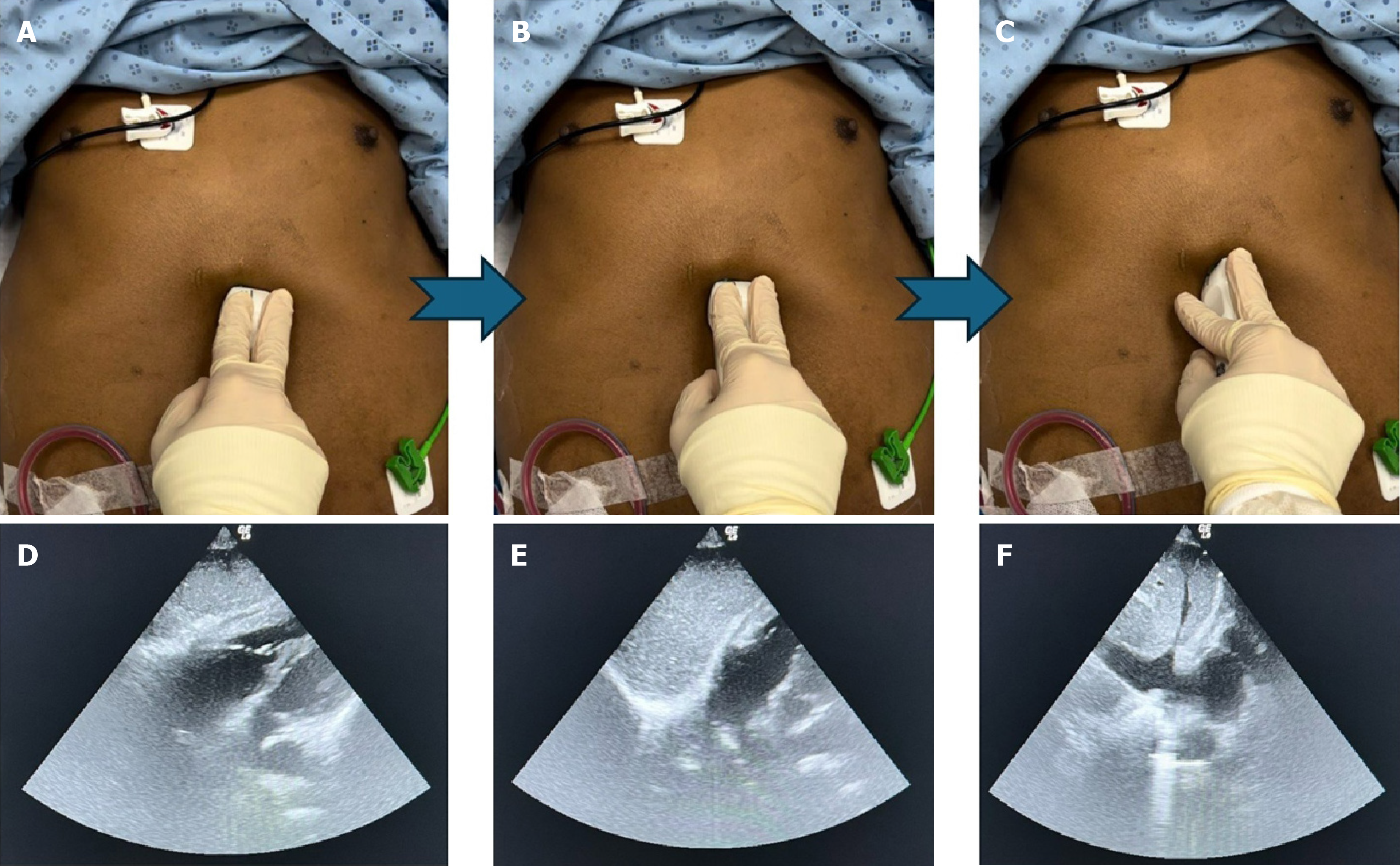
Figure 3 Measures for locating the inferior vena cava using a phased array probe.
A and D: Firstly, get an ideal subcostal four chambers echo view; B and E: Rock the probe towards the patient’s right, bringing the right atrium (RA) to the center of the screen; C and F: Once the RA is in the center, rotate the probe in an anticlockwise direction to open up the inferior vena cava.
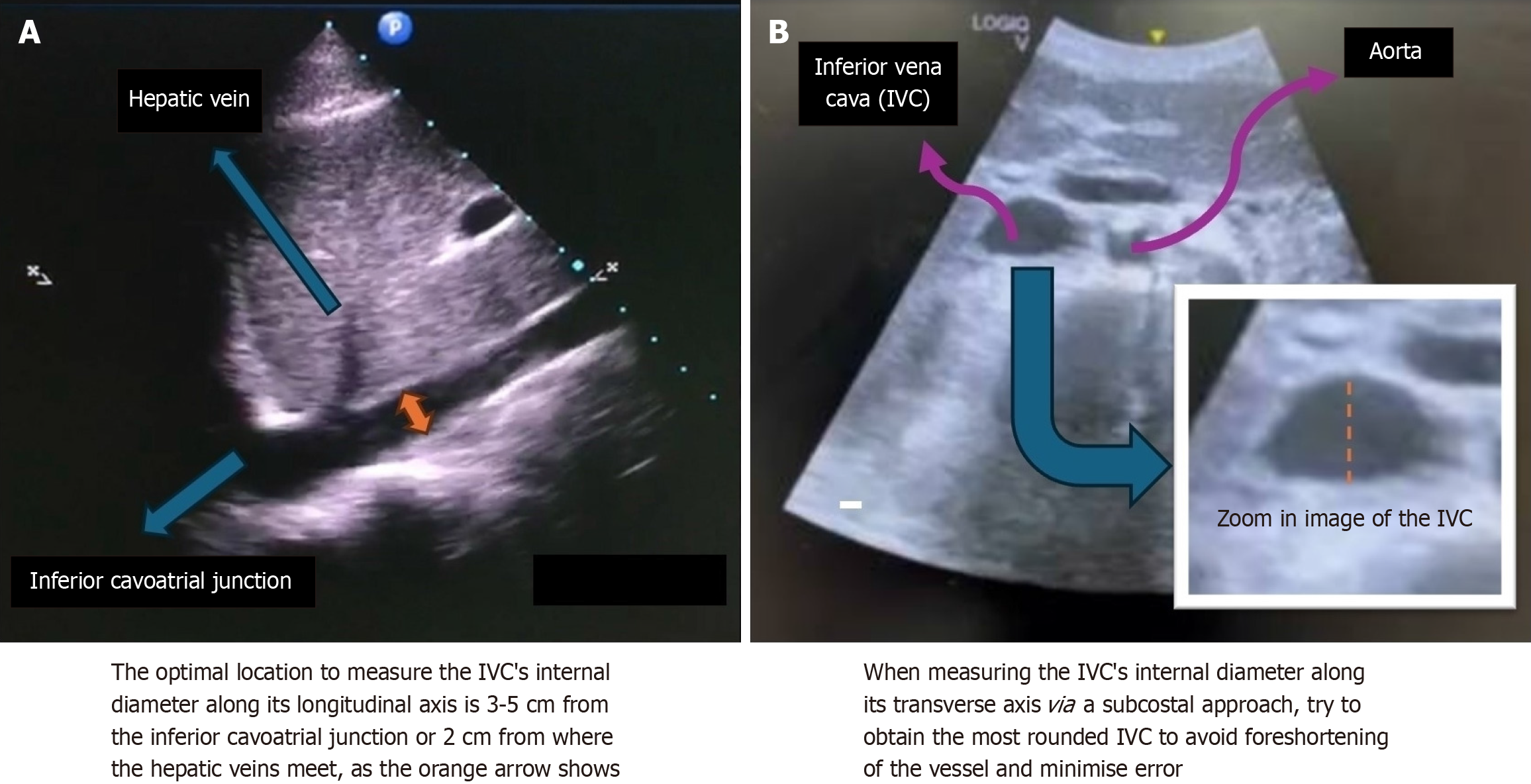
Figure 4 Inferior vena cava images obtained via the subcostal approach.
To guarantee the precision of the Inferior vena cava measurement, it was recommended to do the antero-posterior internal diameter measurement for both the longitudinal and transverse axis. A: Longitudinal axis; B: Transverse axis.
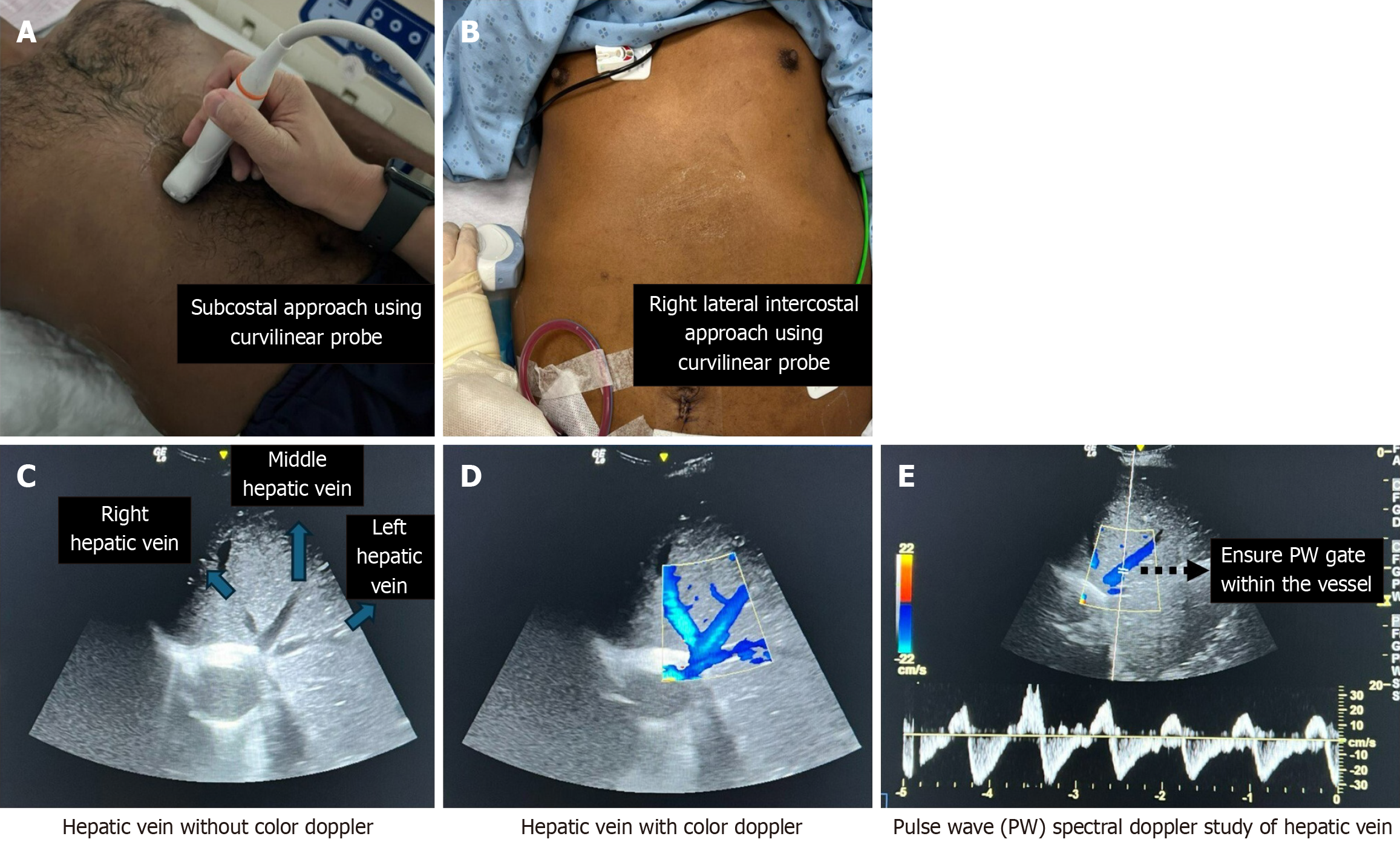
Figure 5 Measures for locating the hepatic vein using a curvilinear probe and performing a pulse wave spectral Doppler study on the hepatic vein.
Locating the hepatic vein using either the subcostal approach or the right lateral intercostal approach, with the pointer directed cephalad and towards the patient's right. A: Subcostal approach; B: Right lateral intercostal approach; C: Hepatic veins consist of right, middle, and left hepatic veins; any one of them can be analyzed for Venous Excess Ultrasound; D: Activating the color Doppler revealed the hepatic vein in blue; E: Once identified, place the pulse wave sample volume, also known as the PW gate, within the hepatic vein.
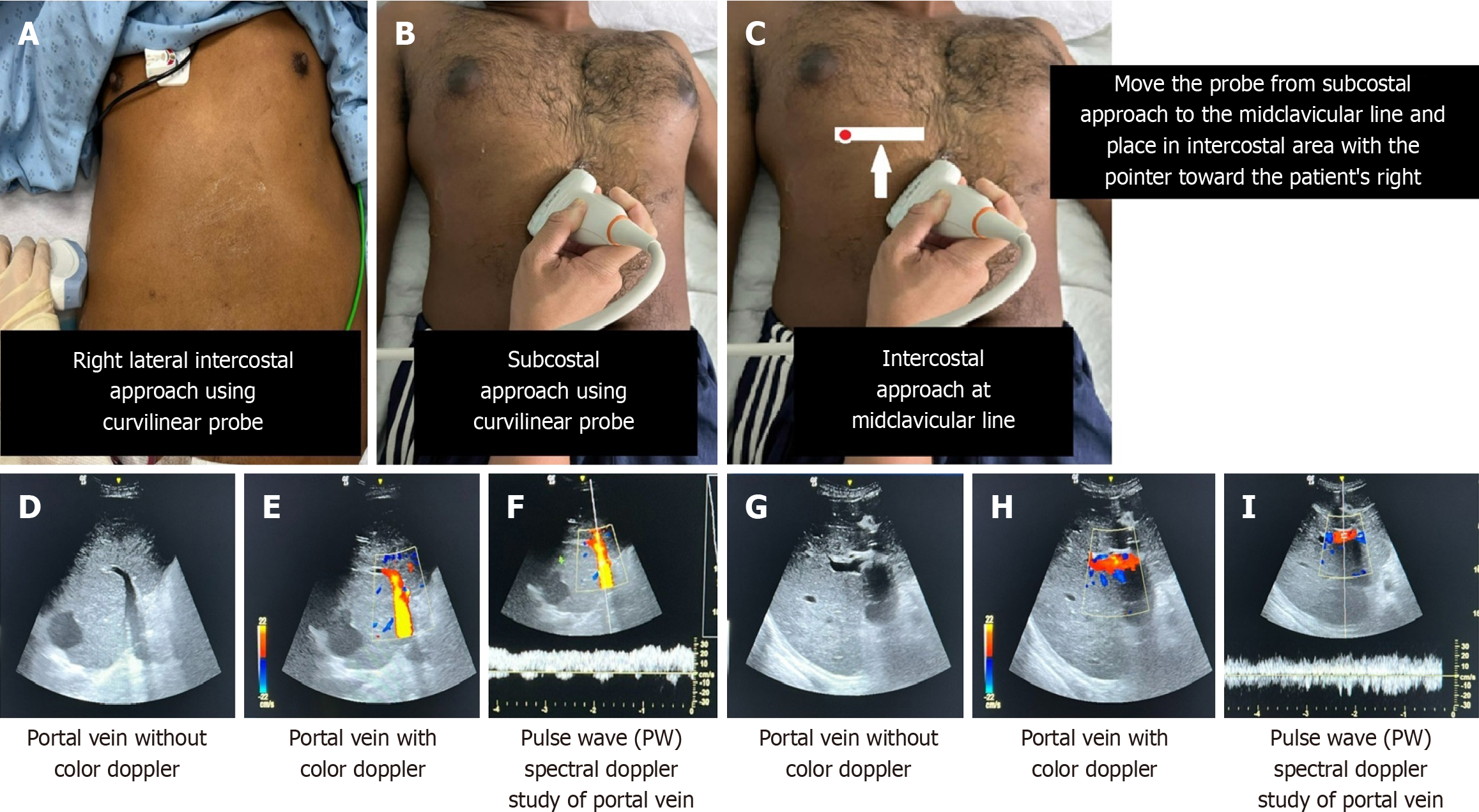
Figure 6 Measures for locating the portal vein using a curvilinear probe and performing a pulse wave spectral Doppler study on the portal vein.
On the left-hand side of the image, we locate the portal vein using the right lateral intercostal or subcostal approach. A: Right lateral intercostal approach; B: Subcostal approach. On the right-hand side of the image, we locate the portal vein using the intercostal approach at the midclavicular line; C: Intercostal approach at the midclavicular line. The portal vein images on each side exhibit slight differences, as do the insonation angles of the portal vein and the pulse wave gate; D-F: Right lateral intercostal or subcostal approach will give an insonation angle of near 0 degree; G-I: Intercostal approaches at the midclavicular line will give an insonation angle of near 90 degrees, which could underestimate the flow velocity measurement.
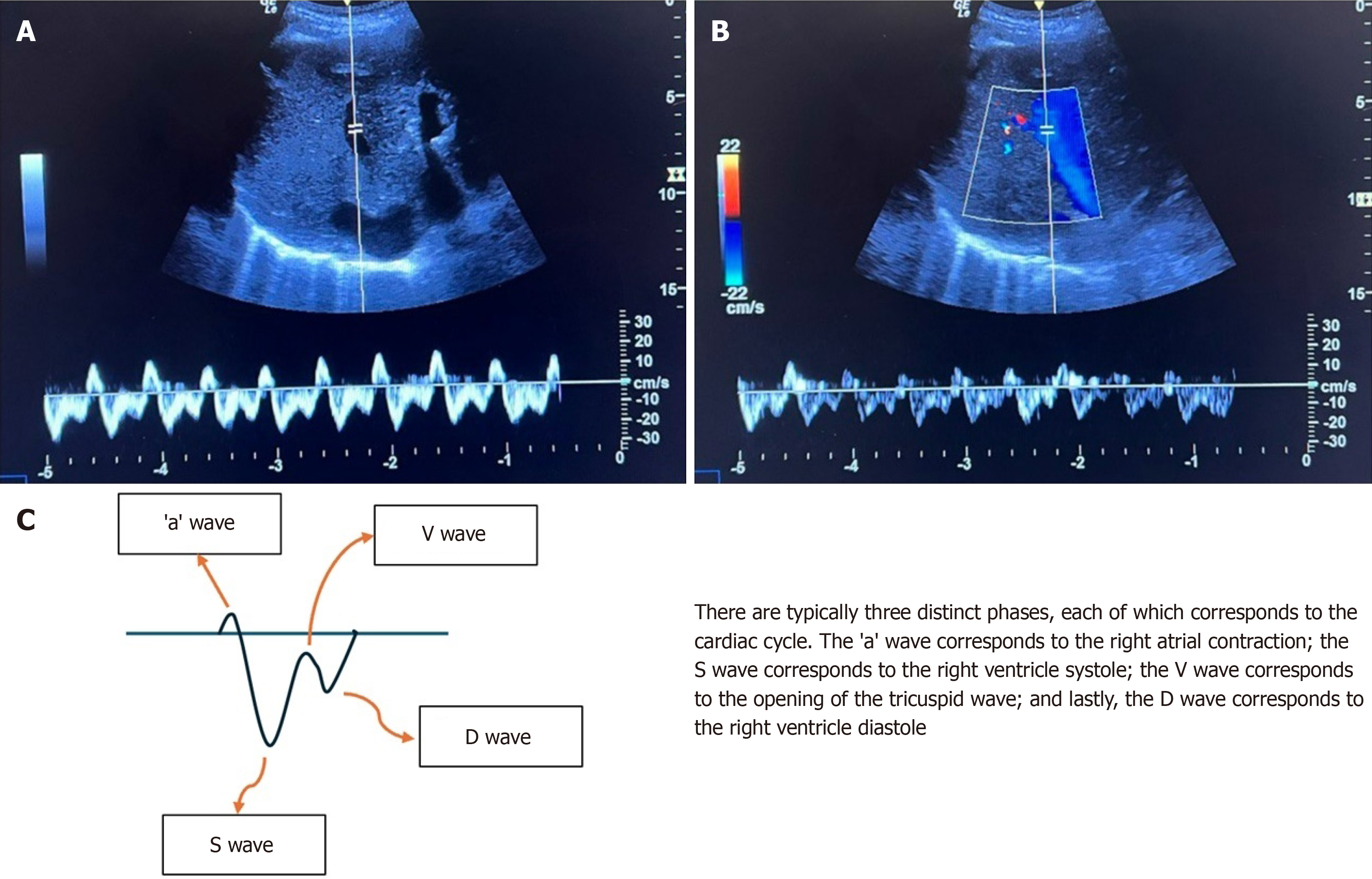
Figure 7 The morphology of the hepatic vein pulse-wave Doppler waveform in a normal condition.
A: Hepatic vein without color doppler; B: Hepatic with color doppler; C: Hepatic vein pulse-wave doppler waveform in a normal condition.
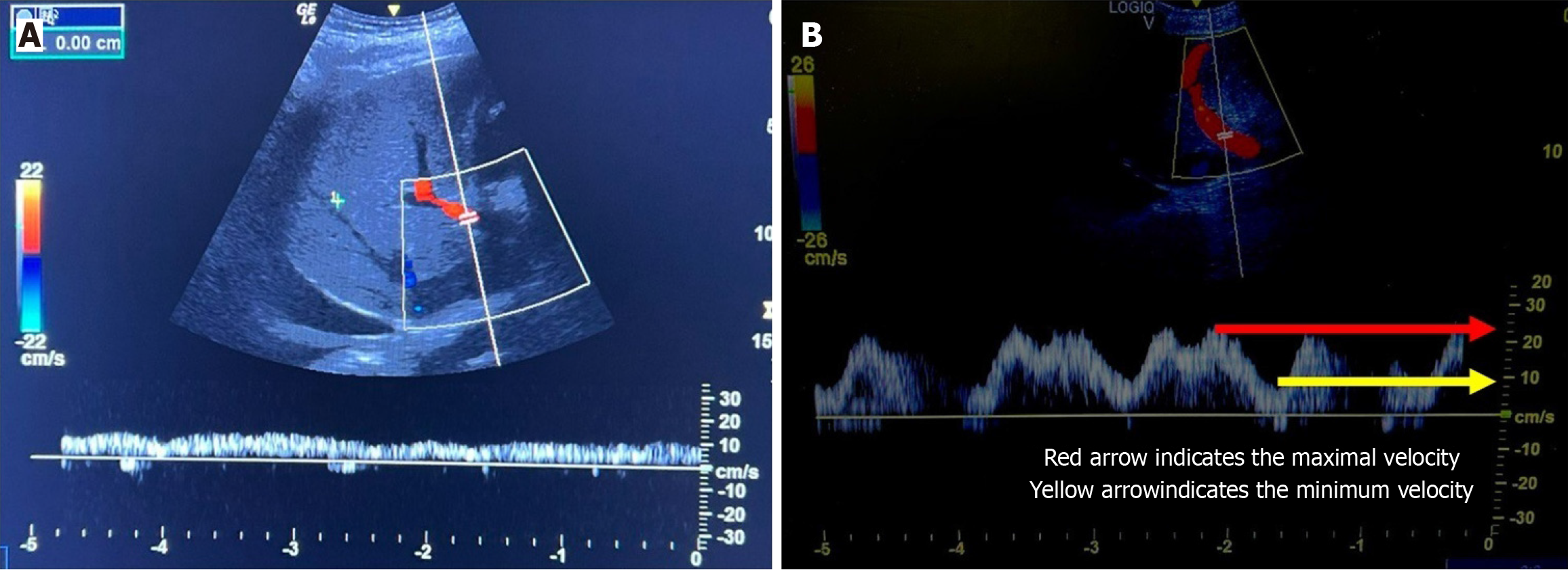
Figure 8 Examples of the portal vein Doppler waveform.
A: In normal condition, the portal vein Doppler waveform exhibit a monophasic flow; B: In a congested portal vein, the portal vein doppler waveform exhibit a pulsatility index > 50%.
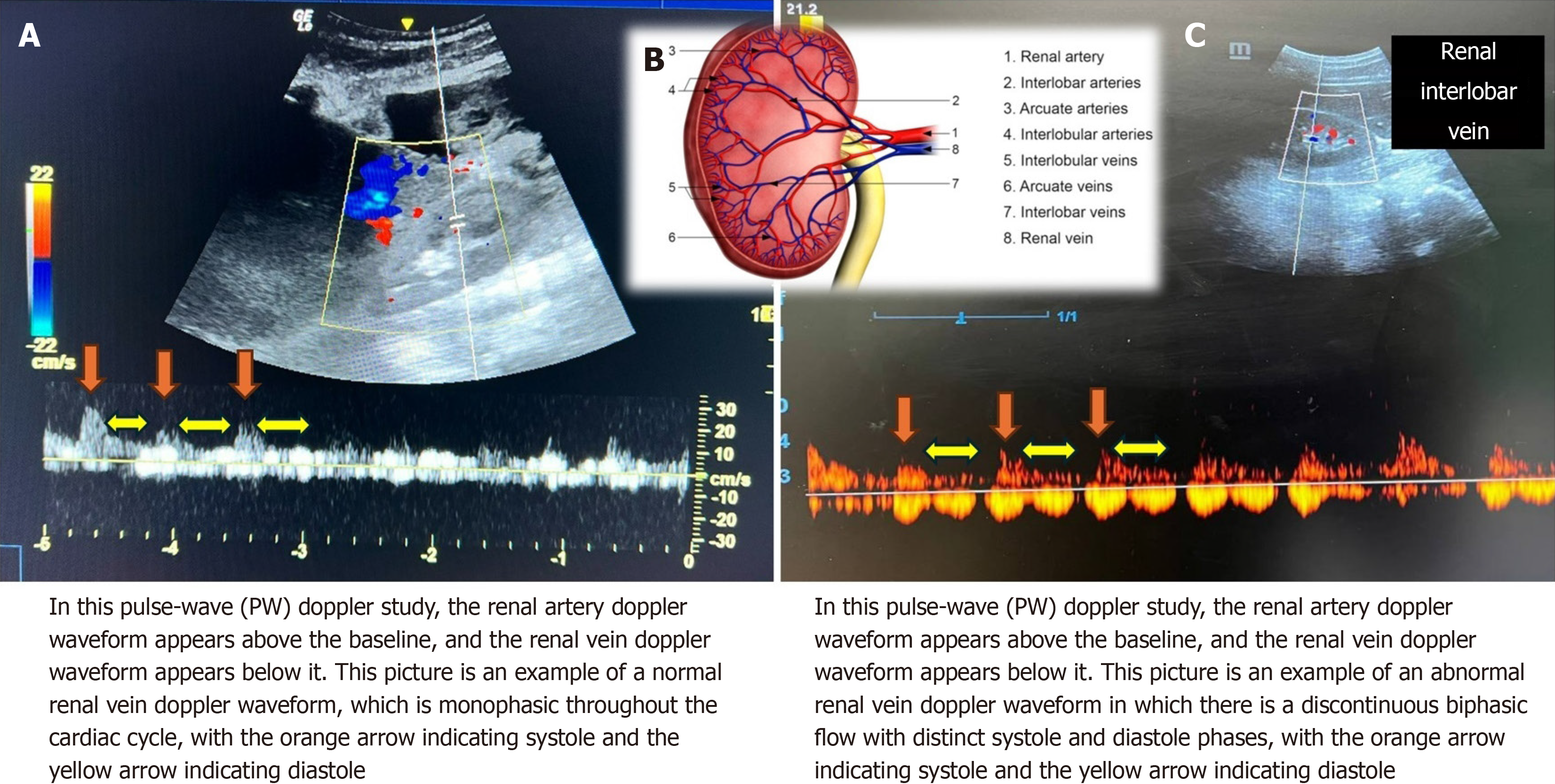
Figure 9 Examples of the renal vein Doppler waveform.
Renal interlobar or arcuate veins are the optimal Doppler sampling sites while performing Venous Excess Ultrasound grading assessments for renal veins. A: Normal renal vein doppler waveform which is monophasic throughout the cardiac cycle; B: Congested renal vein will exhibit a discontinuous biphasic flow with distinct systole and diastole phases; C: Renal interlobar vein.
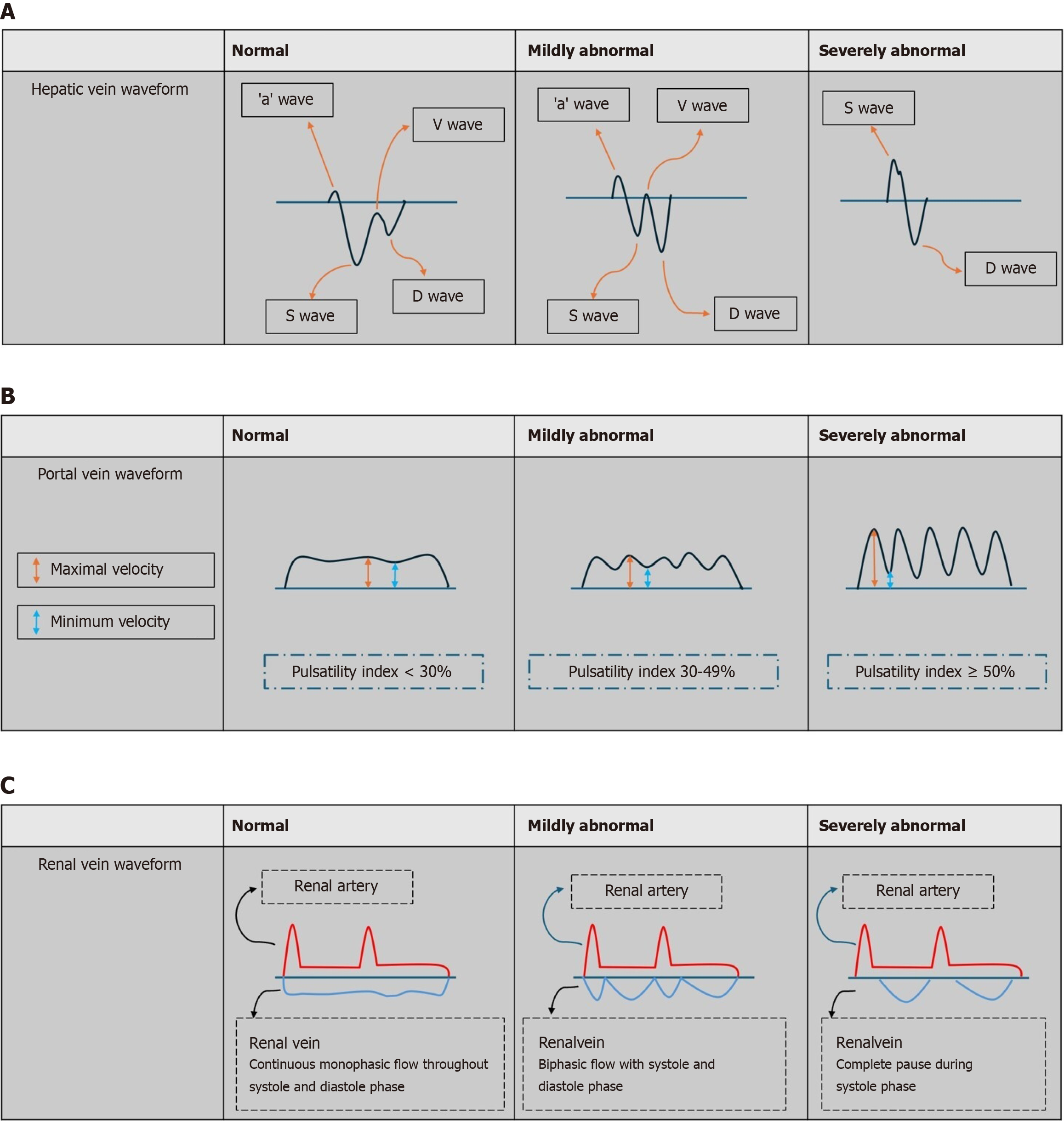
Figure 10 Graphic representation of the interpretation of the venous excess ultrasound grading system.
Grade 0: Inferior vena cava (IVC) < 2 cm signifying no congestion. A: Grade 1: IVC ≥ 2 cm and any combination of normal or mildly abnormal waveforms, reflects only mild congestion; B: Grade 2: IVC ≥ 2 cm with one severely abnormal waveform, indicating severe congestion in a single organ; C: Grade 3: IVC ≥ 2 cm with ≥ two severely abnormal waveforms, denotes severe congestion affecting at least two organ system.
- Citation: Chin WV, Ngai MMI, See KC. Venous excess ultrasound: A mini-review and practical guide for its application in critically ill patients. World J Crit Care Med 2025; 14(2): 101708
- URL: https://www.wjgnet.com/2220-3141/full/v14/i2/101708.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i2.101708