Published online May 20, 2015. doi: 10.5321/wjs.v4.i2.39
Peer-review started: February 22, 2015
First decision: March 20, 2015
Revised: April 10, 2015
Accepted: April 28, 2015
Article in press: May 4, 2015
Published online: May 20, 2015
Processing time: 96 Days and 22.2 Hours
The aim of this article is to review the outcomes of platelet preparations in dentistry. A structured electronic search discovered 348 articles, which described the use of autologous platelet concentrates with a relevance to clinical dentistry. Among these articles, 220 articles investigated platelet rich plasma, 99 investigated platelet rich fibrin, 22 investigated plasma rich in growth factors and 7 investigated the use of concentrated growth factors. Several studies reported beneficial treament outcomes in terms of enhanced bone and soft tissue regeneration.
Core tip: Autologous platelet concentrates (platelet-rich plasma, platelet rich fibrin, plasma rich in growth factors, concentrated growth factor), are blood derivatives, prepared from patient's own blood, reach in platelets, growth factors and cytokines, which can be used to promote guided tissue regeneration in dentistry and oral surgery.
- Citation: Rodella LF, Bonazza V. Platelet preparations in dentistry: How? Why? Where? When? World J Stomatol 2015; 4(2): 39-55
- URL: https://www.wjgnet.com/2218-6263/full/v4/i2/39.htm
- DOI: https://dx.doi.org/10.5321/wjs.v4.i2.39
Bone and soft tissue regeneration is frequently required in dentistry, mainly but not exclusively for implantology and periodontology. Tissue regeneration is a complex process of healing and tissue growth, which involves different biological elements and strategies. These include the use of bone grafts[1,2], biomaterials and growth factors[3], natural or synthetic scaffolds and more recently the use of stem cells[4,5]. Nowadays, a whole range of modern surgical procedures and a variety of dental materials are available. These are performed to reconstruct bony defects of the upper and lower jaw and for augmentation of lost structures of the residual alveolar ridge. Autologous platelet concentrates are a promising and innovative therapeutic approach in various medical fields, including dentistry[6-10]. Platelets play a crucial role not only in hemostasis, but also in the wound healing process, as they are reservoirs of growth factors and cytokines, which in turn are key promoters for bone and soft tissues regeneration. After platelets are activated, they become trapped within a fibrin matrix and release growth factors. Together the fibrin can form a scaffold and the growth factors can stimulate tissue healing and regeneration repair responses. An improved understanding of the physiologic properties of platelets in wound healing over the last two decades, has led to more successful therapeutic applications, especially in oral surgery.
Platelet concentrates are blood derivatives[11,12], prepared from the patient’s own blood and containing autologous platelets, growth factors and cytokines involved in the key processes of tissue regeneration, including cell proliferation and differentiation, extracellular matrix synthesis, chemotaxis and angiogenesis. Platelets are packed with secretory granules, which are necessary to fulfill their functions. There are three types of secretory granules, α granules are the most abundant and have a high protein content. The granules contain cytokines and growth factors, such as vascular endothelial growth factor, epidermal growth factor, platelet-derived growth factor, fibroblast growth factor, hepatocyte growth factor and the insulin-like growth factor as well as several others. The release of these growth factors from activated platelets can promote healing in both soft and hard tissues.
Most platelet concentrate preparations used in guided tissue regeneration surgery are termed Platelet-Rich Plasma (PRP), even if they differ slightly according to their preparation from a patients peripheral blood. These variations include differences in centrifugation speeds and times, differences in adding chemicals, and differences in the selection of supernatants and precipitates. These variations can cause differences in fibrin network structures and in platelets, leucocyte and growth factors content. Therefore the term PRP alone can be non-specific, because it does not define the actual preparation protocol. Depending on the leukocyte content and fibrin architecture, five main categories of PRPs can be defined: (1) Pure Platelet-Rich Plasma, such as cell separator PRP, Vivostat platelet rich fibrin (PRF)[13] or Anitua’s PRGF[14,15]; (2) Leukocyte and Platelet-Rich Plasma; (3) Pure Plaletet-Rich Fibrin, such as Fibrinet; (4) Leukocyte- and Platelet-Rich Fibrin, such as Choukroun’s PRF; and (5) Concentrated growth factors (CGF). In the following paragraphs, the use of PRP, PRF, plasma rich in growth factors (PRGF) and CGF in dentistry and oral surgery will be reviewed.
PRP is blood plasma that has been enriched with platelets and it was the first generation of platelet concentrates to be used in clinical practice by Marx in 1998[16]. PRP has a platelet concentration of 1000 × 109/L in 5 mL of plasma, which is 3-5 times higher compared to the normal whole blood platelet count (150-400 × 109/L). PRP contains (and releases through platelet degranulation) several growth factors and cytokines that can stimulate bone and soft tissue healing[17-19]. PRP is prepared by drawing peripheral venous blood from a patient’s arm. The fresh blood is immediately mixed with an anti-coagulant to prevent clotting and then the platelets are concentrated using a two-step gradient centrifugation method[20]. In this method, the first spin (called the hard spin) separates the red blood cells (RBCs) from the plasma containing platelets, leukocytes and clotting factors, the second spin (called the soft spin) is used to delicately separate the platelets and leukocytes, from the plasma. The soft spin produces PRP and separates it from the platelet-poor plasma (PPP), free from the interference associated with large number of red blood cells. Commonly, with commercially available systems, a one-step method is used to separate the RBCs, buffy coat and plasma into three distinct layers. The buffy coat contains platelets and leukocytes and is often collected as PRP. The top plasma layer is often called PPP, which is discarded, leaving the PRP to be injected into surgical sites to accomplish guided tissue regeneration.
PRF consists of an intimate assembly of cytokines, glycanic chains, structural glycoproteins enmeshed within a fibrin network, and is considered to be the second generation of platelet concentrates[21-23]. The cytokines, glycanic chains, structural glycoproteins can have synergetic effects on tissue healing processes. The PRF pioneers were Choukroun et al[24,25], who used it to promote the osseointegration of dental implants. Several studies have demonstrated the clinical effectiveness of autologous PRF to regenerate defects in hard and soft tissues. The preparation of PRF is similar to PRP and consists in collecting peripheral venous blood from the patient's arm. Except that no anti-coagulant is used during blood harvesting. After the blood is collected it is immediately centrifuged for 10 min to activate the platelets, leading to the initiation of a coagulation cascade. After centrifugation, the blood is separated into three different layers: acellular PPP (platelet poor plasma) on top, a PRF clot in the middle and RBCs at the bottom of the test tube. The PRF clot obtained after centrifugation is collected, 2 mm below the lower dividing line and the other layers are discarded. The clinical success of the PRF protocol is dependent on a quick collection of blood and its transfer to the centrifuge. Because no anti-coagulant is used, the blood sample begins to coagulate almost immediately, and a failure to accomplish the quick preparation of PRF could cause a diffuse polymerization of fibrin, which is not ideal for tissue healing.
PRGF is prepared from peripheral venous blood drawn from a patient’s arm. PRGF is prepared using a modified PRP protocol developed by Anitua[26-28]. The difference between PRGF and PRP is that PRGF is optimized to deliver a more sustained release of growth factors. PRGF can create a three-dimensional fibrin scaffold which can be injected into a tissue defect, to maintain the regenerative space and can be used as a scaffold for cells to accomplish tissue regeneration. The Leukocyte content of PRGF is eliminated to prevent the pro-inflammatory effects of the proteases and acid hydrolases contained within these cells. PRGF is prepared from a small volume of patient’s peripheral venous blood and is collected by a one-step centrifugation using sodium citrate as the anti-coagulant (Endoret System, Biotechnology Institut, Minano, Alava, Spain). After activation, PRGF progressively releases a pool of proteins and growth factors, which accelerate soft tissue healing as well as bone regeneration. Different formulations of PRGF with therapeutic potential can be obtained from a patient’s blood depending on the degree of coagulation and activation of the samples. PRGF supernatant can be used as conventional eye-drop solution and cell culture media solution; liquid PRGF can be used to coat dental implant surfaces to promote osseointegration; the fibrillar and cellular scaffold-like PRGF can be used to fill tissue defects as part of ulcer treatment, sealing tooth sockets after tooth extraction, and promoting the epithelialization of soft tissues.
CGF, first developed by Sacco, in 2006, is an autologous fibrin network, rich in leukocytes and platelets[29,30]. CGF also contains autologous osteo-inductive growth factors derived from platelets and an osteo-inductive fibrin matrix. Similar to PRF, CGF is created using a one-step centrifugation method, but it requires a special programmed centrifuge (Medifuge MF200, Silfradent srl, Forli, Italy), which uses plastic tubes, coated with silica particles, and without the addition of exogenous substances. The final blood product is separated into three layers, two are discarded, and the CGF is collected from the buffy coat layer, which consists of a dense fibrin matrix that is rich in growth factors.
A structured electronic search of scientific papers up to January 2015, was conducted using two medical databases (PubMed and the Cochrane Library) and specific keywords: “platelet concentrates in dentistry”, “PRF”“Platelet rich fibrin Choukroun”, “platelets in dentistry and maxillofacial surgery”, “PRP”, “CGF”, “PRGF”, “periodontal regeneration”. For each of these platelet concentrate categories, their therapeutic potential in dentistry was evaluated according to the following inclusion criteria: (1) clinical trials; (2) animal studies; (3) in vitro studies; (4) case reports; and (5) technical reports. Subsequently, the articles for each type of platelet concentrate (PRP, PRF, PRGF and CGF) were classified according to these inclusion criteria and study type.
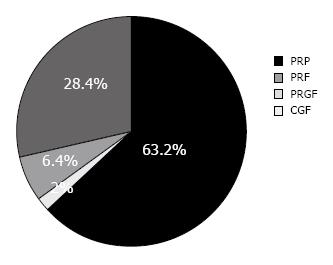
A total of 563 articles were identified as meeting the inclusion criteria of investigating the clinical use of autologous platelet concentrates in dentistry. However, after all the studies not relevant to dentistry, or containing no data were excluded, 348 articles were included in this review. Of the 348 articles, 220 articles (63.2%) were about PRP, 99 articles (28.4%) investigated PRF, 22 articles (6.4%) investigated PRGF and 7 articles (2%) were about CGF (Figure 1).
The articles were classified according to the type of platelet preparations in dentistry and the type of research performed in the article, which are briefly described below and summarized in Table 1: (1) PRP: from 220 articles, 116 were human clinical trials, 46 regarded animal studies, 20 were about in vitro investigations, 3 were technical reports and 35 were case reports; (2) PRF: from 99 articles, 50 were human clinical trials, 13 regarded animal studies, 17 were about in vitro experiments, 1 was a technical report about PRF general properties and 18 were case reports; (3) PRGF: from 22 articles, 13 were human clinical trials, 5 regarded animal studies, 2 were about in vitro experiments and 2 were case reports; and (4) CGF: from 7 articles, 1 was a human clinical study, 1 regarded an animal study, 1 was about an in vitro study, 2 were technical reports about CGF properties and its application in dental implantology and 2 were case reports.
| Platelets concentrates | ||||
| Study type | PRP | PRF | PRGF | CGF |
| Clinical trials | 116 | 50 | 13 | 1 |
| Animal studies | 46 | 13 | 5 | 1 |
| In vitro studies | 20 | 17 | 2 | 1 |
| Technical report | 3 | 1 | 0 | 2 |
| Case report | 35 | 18 | 2 | 2 |
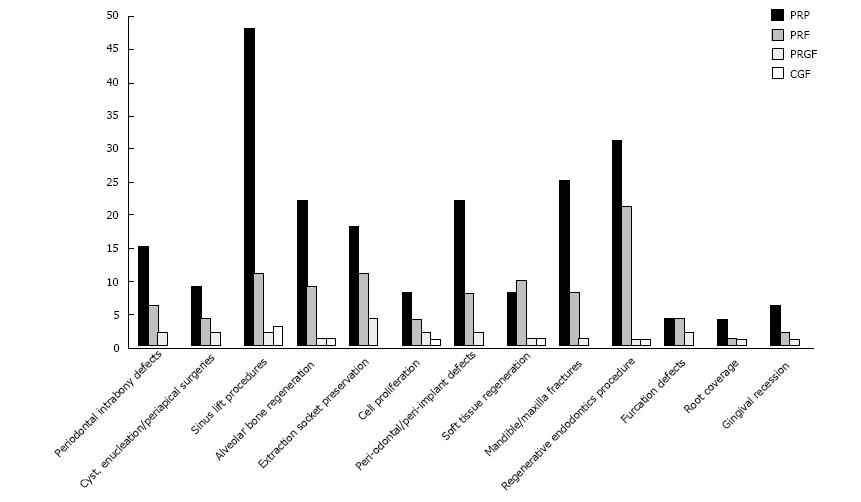
PRP was used to treat periodontal intrabony defects in fifteen studies[31-45]. Nine studies described the use of PRP in cyst enucleations/periapical surgeries[46-54]. Forty-eight studies investigated PRP in sinus floor elevation treatments[55-101]. Twenty-two studies reported the use of PRP for the treatment of periodontal and periimplant defects[102-123]. Four studies used PRP for covering the roots of teeth[124-127]. Six studies investigated the efficacy of PRP for the treatment of gingival recession[128-133]. Four studies evaluated the benefits of using PRP to repair furcation defects[134-137]. Twenty-five studies investigated PRP for the repair of mandible/maxilla fractures[138-160]. Thirty-one studies investigated the use of PRP in endodontic surgery[161-188]. Eighteen studies investigated the use of PRP for dental extraction socket preservation before implant placement[189-206]. Twenty-two studies investigated the stimulating effect of PRP on alveolar bone regeneration and reconstruction[207-224]. Eight studies investigated the use of PRP to improve the healing and regeneration of soft tissues[225-231], mostly for periodontal ligament repair, and reducing the incidence of complications. Eight studies investigated PRP using in vitro protocols to enhance the migration and proliferation of human dental stem cells and gingival fibroblasts[232-237] (Figure 2).
PRF was used in six studies to treat periodontal intrabony defects[238-243]. Four studies used PRF to regenerate tissue following cyst enucleations, and periapical surgeries[244-246]. Eleven studies investigated the ability of PRF to regenerate tissues following sinus floor elevation[247-256]. Eight studies investigated the use of PRF to treat periodontal and periimplant defects[257-263]. One study tested PRF as a potential root coverage repair treatment[264]. Two studies investigated the efficacy of PRF in gingival recession treatment[265,266]. Four studies investigated PRF to treat furcation defects[267-269]. Eight studies applied PRF to heal mandible or maxilla fractures[270-276]. Twenty one studies investigated the usefulness of PRF as part of endodontic surgery to repair periapical tissues[277-293] . Eleven studies investigated the ability of PRF to preserve tooth sockets after tooth extraction in preparation for dental implant placement[294-302]. Nine studies investigated the ability of PRF to stimulate alveolar bone regeneration and reconstruction[303-309]. Ten studies investigated the ability of PRF to improve the healing and regeneration of soft tissues, especially periodontal ligament, reducing complications[310-319]. Four studies investigated the in vitro effects of PRF to enhance the migration and proliferation of human dental stem cells and gingival fibroblasts[320-323] (Figure 2).
PRGF was investigated in two studies to treat periodontal bone defects[324,325]. PRGF was investigated in two studies to regenerate tissues following cyst enucleations and periapical surgeries[326,327]. The potential of PRGF to heal tissues following sinus floor elevation treatment[328,329] was reported in two studies. Two studies reported that PRGF had a positive effect on the healing of periodontal and periimplant defects[330,331]. One study investigated the use of PRF to cover the roots of teeth[332]. One study investigated the efficacy of PRGF to heal tissues following gingival recession treatment[333]. Two studies investigated the benefits of PRGF for the treatment of furcation defects[334,335]. One study investigated the effectiveness of PRGF to heal mandible/maxilla fractures[336]. One study investigated the effectiveness of PRGF to heal periapical soft tissues following endodontic surgery[337]. Four studies investigated the clinical potential of PRGF to preserve tissue in tooth extraction sockets prior to dental implant placement[338-340]. One study investigated the stimulating effect of PRGF on alveolar bone regeneration and reconstruction[341]. One study investigated the ability of PRGF to improve the healing and regeneration of soft tissues, especially the periodontal ligament[342]. Two studies investigated the in vitro effect of PRGF to enhance the migration and proliferation of human dental stem cells and gingival fibroblasts[343,344] (Figure 2).
Compared to the other platelet articles, only a few had investigated the use of CGFs as part of dental treatment. A reason for the lack of CGF articles may be because it is newest of the platelet protocols and there has not been enough time for many articles to be published. Three studies were found which investigated CGF for tissue regeneration following sinus floor elevation[345-347]. One study investigated the in vitro effectiveness of CGF to enhance the migration and proliferation of human dental stem cells and gingival fibroblasts[348]. One study investigated the healing effects of CGF for tissue repair following endodontic surgery[349]. Two studies investigated soft tissue and periodontal ligament healing after using CGF to accomplish guided tissue regeneration[350,351] (Figure 2).
Dentists have different types of biomimetic biomaterials to help guided bone and soft tissue regeneration. All these biomaterials have advantages and limitations and no single type of biomaterial has all the properties needed to be the universal dental regeneration biomaterial. A natural scaffold regeneration material is the blood clot, and several protocols have been developed to improve the scaffold and growth factor properties of the blood clot (PRP, PRF, PRGF and CGF). These platelet rich preparations have been shown to improve healing, quicken tissue regeneration, improve the quality of tissues that are regenerated, and to reduce the incidence of complications. Alternatively, there are also many studies, which have shown that platelet rich preparations had little or no effect on tissue healing in comparison to biomimetic scaffolds. This explains the need to carefully investigate the uses of platelet concentrates as part of dental treatments.
After the careful analysis of the literature, the follow questions could be asked: (1) How is platelet rich fractions of blood prepared? (2) Why use platelet concentrates in dentistry? (3) Where to use platelet concentrates in dentistry? and (4) When to use platelet concentrates in dentistry?
The answer to the first question about how platelet rich fractions of blood are prepared, was answered in the previous paragraphs. All the techniques involve the centrifugation of the patient’s peripheral venous blood and the use of fractions containing fibrin, platelets, leukocytes and growth factors. Red blood cells are discarded.
The answer to the second question about why platelet concentrates are used in dentistry is because they are cheap natural scaffolds and source of growth factors to stimulate tissue regeneration. Platelet concentrates are biocompatible and can sometimes offer potential benefits including rapid wound healing and bone regeneration. A controversial advantage is a reduction of postoperative pain and an unequivocal advantage is the lack of risk of infectious disease transmission. Sometimes platelet concentrates cannot be used where a patient does not want to donate their own blood, or when a special-needs patient or child refuses to cooperate with the collection of their blood.
The answer to the third question about why autologous platelet concentrates are used in oral and maxillofacial surgery and periodontal regenerative therapy is because of some promising results for tissue regeneration following sinus floor elevation (especially with PRP and CGF)[55-101,345-347], bone filling of periodontal intrabony defects[102-123,238-243,324,325], regeneration of alveolar ridges[207-224,303-311,343], dental extraction socket preservation[189-206,294-302,338-340], gingival recession treatment[128-133,265,266], mandibular and maxilla fractures[138-160,270-276,333]. Platelet concentrates have been used to manage bisphosphonate-related osteonecrosis of the jaw to enhance wound healing and bone maturation[271,272,352].
The answer to the fourth question about when to use platelet concentrates is the most difficult to reach for most dentists. A general rule of guidance is to use platelet concentrates, scaffolds, or biomaterials, in surgical situations where the prognosis for tissue repair is poor in the absence of a tissue regeneration scaffold and addition of growth factors[225-231,310-319].
In conclusion, platelets concentrates represents innovative tools in dentistry. The results, demonstrate that these concentrates are effective at improving bone and soft tissues healing. Moreover, well-enhanced bone regeneration can be obtained when PRP, PRF and CGF are used together with autogenous bone, with recombinant human growth factors such as recombinant BMP and also with other biomaterials (as for example Bio-Oss- Geistlich-Switzerland and Hydroxyapatite)[95-96]. However, the definition and validation of accurate protocols is a key issue for the long-term development of these techniques. So for further research is required to establish a standardized protocol for the use of these concentrates in the treatment of tissue regeneration.
Dott Robert Coates for English language revision.
P- Reviewer: Galiatsatos AA, Gorseta K, Lopez-Jornet P S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Buffoli B, Boninsegna R, Rezzani R, Poli PP, Santoro F, Rodella LF. Histomorphometrical evaluation of fresh frozen bone allografts for alveolar bone reconstruction: preliminary cases comparing femoral head with iliac crest grafts. Clin Implant Dent Relat Res. 2013;15:791-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Rodella LF, Favero G, Boninsegna R, Borgonovo A, Rezzani R, Santoro F. TGF-beta1 and VEGF after fresh frozen bone allograft insertion in oral-maxillo-facial surgery. Histol Histopathol. 2010;25:463-471. [PubMed] |
| 3. | Rodella LF, Favero G, Labanca M. Biomaterials in maxillofacial surgery: membranes and grafts. Int J Biomed Sci. 2011;7:81-88. [PubMed] |
| 4. | Lane SW, Williams DA, Watt FM. Modulating the stem cell niche for tissue regeneration. Nat Biotechnol. 2014;32:795-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 425] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 5. | Brown PT, Handorf AM, Jeon WB, Li WJ. Stem cell-based tissue engineering approaches for musculoskeletal regeneration. Curr Pharm Des. 2013;19:3429-3445. [PubMed] |
| 6. | Anitua E, Pelacho B, Prado R, Aguirre JJ, Sánchez M, Padilla S, Aranguren XL, Abizanda G, Collantes M, Hernandez M. Infiltration of plasma rich in growth factors enhances in vivo angiogenesis and improves reperfusion and tissue remodeling after severe hind limb ischemia. J Control Release. 2015;202:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Bettega G, Schir E. [Contribution of platelet concentrates to oral and maxillo-facial surgery]. Rev Stomatol Chir Maxillofac. 2012;113:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Del Corso M, Vervelle A, Simonpieri A, Jimbo R, Inchingolo F, Sammartino G, Dohan Ehrenfest DM. Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: Periodontal and dentoalveolar surgery. Curr Pharm Biotechnol. 2012;13:1207-1230. [PubMed] |
| 9. | Lynch SE, Wisner-Lynch L, Nevins M, Nevins ML. A new era in periodontal and periimplant regeneration: use of growth-factor enhanced matrices incorporating rhPDGF. Compend Contin Educ Dent. 2006;27:672-678; quiz 679-680. [PubMed] |
| 10. | Rozman P, Bolta Z. Use of platelet growth factors in treating wounds and soft-tissue injuries. Acta Dermatovenerol Alp Pannonica Adriat. 2007;16:156-165. [PubMed] |
| 11. | Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91:4-15. [PubMed] |
| 12. | Prakash S, Thakur A. Platelet concentrates: past, present and future. J Maxillofac Oral Surg. 2011;10:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Agren MS, Rasmussen K, Pakkenberg B, Jørgensen B. Growth factor and proteinase profile of Vivostat® platelet-rich fibrin linked to tissue repair. Vox Sang. 2014;107:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Anitua E, Sánchez M, Orive G, Andía I. The potential impact of the preparation rich in growth factors (PRGF) in different medical fields. Biomaterials. 2007;28:4551-4560. [PubMed] |
| 15. | Anitua E. The use of plasma-rich growth factors (PRGF) in oral surgery. Pract Proced Aesthet Dent. 2001;13:487-493; quiz 487-493. [PubMed] |
| 16. | Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001;10:225-228. [PubMed] |
| 17. | Leitner GC, Gruber R, Neumüller J, Wagner A, Kloimstein P, Höcker P, Körmöczi GF, Buchta C. Platelet content and growth factor release in platelet-rich plasma: a comparison of four different systems. Vox Sang. 2006;91:135-139. [PubMed] |
| 18. | Cavallo C, Filardo G, Mariani E, Kon E, Marcacci M, Pereira Ruiz MT, Facchini A, Grigolo B. Comparison of platelet-rich plasma formulations for cartilage healing: an in vitro study. J Bone Joint Surg Am. 2014;96:423-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 19. | Malhotra A, Pelletier MH, Yu Y, Walsh WR. Can platelet-rich plasma (PRP) improve bone healing? A comparison between the theory and experimental outcomes. Arch Orthop Trauma Surg. 2013;133:153-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 20. | Ogundipe OK, Ugboko VI, Owotade FJ, Paul-Odo B, Afariogun AB. Preparation of platelet-rich plasma from small volume of whole blood - a simplified approach. Niger Postgrad Med J. 2012;19:133-136. [PubMed] |
| 21. | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37-e44. [PubMed] |
| 22. | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-e50. [PubMed] |
| 23. | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e51-e55. [PubMed] |
| 24. | Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299-303. [PubMed] |
| 25. | Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56-e60. [PubMed] |
| 26. | Anitua E, Zalduendo MM, Prado R, Alkhraisat MH, Orive G. Morphogen and proinflammatory cytokine release kinetics from PRGF-Endoret fibrin scaffolds: evaluation of the effect of leukocyte inclusion. J Biomed Mater Res A. 2015;103:1011-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 27. | Anitua E, Sánchez M, Orive G. The importance of understanding what is platelet-rich growth factor (PRGF) and what is not. J Shoulder Elbow Surg. 2011;20:e23-e24; author reply e24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14:529-535. [PubMed] |
| 29. | Honda H, Tamai N, Naka N, Yoshikawa H, Myoui A. Bone tissue engineering with bone marrow-derived stromal cells integrated with concentrated growth factor in Rattus norvegicus calvaria defect model. J Artif Organs. 2013;16:305-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Rodella LF, Favero G, Boninsegna R, Buffoli B, Labanca M, Scarì G, Sacco L, Batani T, Rezzani R. Growth factors, CD34 positive cells, and fibrin network analysis in concentrated growth factors fraction. Microsc Res Tech. 2011;74:772-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 207] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 31. | Agarwal A, Gupta ND. Platelet-rich plasma combined with decalcified freeze-dried bone allograft for the treatment of noncontained human intrabony periodontal defects: a randomized controlled split-mouth study. Int J Periodontics Restorative Dent. 2014;34:705-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Pinipe J, Mandalapu NB, Manchala SR, Mannem S, Gottumukkala NV, Koneru S. Comparative evaluation of clinical efficacy of β-tri calcium phosphate (Septodont-RTR)™ alone and in combination with platelet rich plasma for treatment of intrabony defects in chronic periodontitis. J Indian Soc Periodontol. 2014;18:346-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Döri F, Arweiler N, Húszár T, Gera I, Miron RJ, Sculean A. Five-year results evaluating the effects of platelet-rich plasma on the healing of intrabony defects treated with enamel matrix derivative and natural bone mineral. J Periodontol. 2013;84:1546-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 34. | Menezes LM, Rao J. Long-term clinical evaluation of platelet-rich plasma in the treatment of human periodontal intraosseous defects: A comparative clinical trial. Quintessence Int. 2012;43:571-582. [PubMed] |
| 35. | Ozdemir B, Okte E. Treatment of intrabony defects with beta-tricalciumphosphate alone and in combination with platelet-rich plasma. J Biomed Mater Res B Appl Biomater. 2012;100:976-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Rodrigues SV, Acharya AB, Thakur SL. An evaluation of platelet-rich plasma without thrombin activation with or without anorganic bone mineral in the treatment of human periodontal intrabony defects. Platelets. 2011;22:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Saini N, Sikri P, Gupta H. Evaluation of the relative efficacy of autologous platelet-rich plasma in combination with β-tricalcium phosphate alloplast versus an alloplast alone in the treatment of human periodontal infrabony defects: a clinical and radiological study. Indian J Dent Res. 2011;22:107-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Yilmaz S, Kabadayi C, Ipci SD, Cakar G, Kuru B. Treatment of intrabony periodontal defects with platelet-rich plasma versus platelet-poor plasma combined with a bovine-derived xenograft: a controlled clinical trial. J Periodontol. 2011;82:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 39. | Kaushick BT, Jayakumar ND, Padmalatha O, Varghese S. Treatment of human periodontal infrabony defects with hydroxyapatite + β tricalcium phosphate bone graft alone and in combination with platelet rich plasma: a randomized clinical trial. Indian J Dent Res. 2011;22:505-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 40. | Carvalho MD, Suaid FF, Santamaria MP, Casati MZ, Nociti FH, Sallum AW, Sallum EA. Platelet-rich plasma plus bioactive glass in the treatment of intra-bony defects: a study in dogs. J Appl Oral Sci. 2011;19:82-89. [PubMed] |
| 41. | Kang J, Sha YQ, Ou-yang XY. [Combination therapy of periodontal intrabony defects with demineralized freeze-dried bone powder and platelet-rich plasma]. Beijing Daxue Xuebao. 2010;42:24-27. [PubMed] |
| 42. | Kotsovilis S, Markou N, Pepelassi E, Nikolidakis D. The adjunctive use of platelet-rich plasma in the therapy of periodontal intraosseous defects: a systematic review. J Periodontal Res. 2010;45:428-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 43. | Yilmaz S, Cakar G, Kuru B, Dirikan S, Yildirim B. Platelet-rich plasma in combination with bovine derived xenograft in the treatment of deep intrabony periodontal defects: a report of 20 consecutively treated patients. Platelets. 2009;20:432-440. [PubMed] |
| 44. | Döri F, Kovács V, Arweiler NB, Huszár T, Gera I, Nikolidakis D, Sculean A. Effect of platelet-rich plasma on the healing of intrabony defects treated with an anorganic bovine bone mineral: a pilot study. J Periodontol. 2009;80:1599-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 45. | Ouyang XY, Qiao J. Effect of platelet-rich plasma in the treatment of periodontal intrabony defects in humans. Chin Med J (Engl). 2006;119:1511-1521. [PubMed] |
| 46. | Güven Polat G, Yıldırım C, Akgün OM, Altun C, Dinçer D, Ozkan CK. The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report. Restor Dent Endod. 2014;39:230-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 47. | Ramanathan A, Cariappa KM. Effect of platelet-rich plasma on bone regeneration after removal of cysts and benign tumours of the jaws. Oral Maxillofac Surg. 2014;18:445-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 48. | Pappalardo S, Guarnieri R. Efficacy of Platelet-Rich-Plasma (PRP) and Highly Purified Bovine Xenograft (Laddec(®)) Combination in Bone Regeneration after Cyst Enucleation: Radiological and Histological Evaluation. J Oral Maxillofac Res. 2013;4:e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 49. | Subramaniam P, Kumar K, Ramakrishna T, Bhadranna A. Bone regeneration with plasma-rich-protein following enucleation of traumatic bone cyst. Eur J Dent. 2013;7:377-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 50. | Del Fabbro M, Ceresoli V, Lolato A, Taschieri S. Effect of platelet concentrate on quality of life after periradicular surgery: a randomized clinical study. J Endod. 2012;38:733-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 51. | Parikh B, Navin S, Vaishali P. A comparative evaluation of healing with a computed tomography scan of bilateral periapical lesions treated with and without the use of platelet-rich plasma. Indian J Dent Res. 2011;22:497-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Nagaveni NB, Praveen RB, Umashankar KV, Pranav B, Sreedevi R, Radhika NB. Efficacy of platelet-rich-plasma (PRP) in bone regeneration after cyst enucleation in pediatric patients--a clinical study. J Clin Pediatr Dent. 2010;35:81-87. [PubMed] |
| 53. | Hiremath H, Gada N, Kini Y, Kulkarni S, Yakub SS, Metgud S. Single-step apical barrier placement in immature teeth using mineral trioxide aggregate and management of periapical inflammatory lesion using platelet-rich plasma and hydroxyapatite. J Endod. 2008;34:1020-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 54. | Demiralp B, Keçeli HG, Muhtaroğullar M, Serper A, Demiralp B, Eratalay K. Treatment of periapical inflammatory lesion with the combination of platelet-rich plasma and tricalcium phosphate: a case report. J Endod. 2004;30:796-800. [PubMed] |
| 55. | Khairy NM, Shendy EE, Askar NA, El-Rouby DH. Effect of platelet rich plasma on bone regeneration in maxillary sinus augmentation (randomized clinical trial). Int J Oral Maxillofac Surg. 2013;42:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 56. | Yilmaz S, Karaca EO, Ipci SD, Cakar G, Kuru BE, Kullu S, Horwitz J. Radiographic and histologic evaluation of platelet-rich plasma and bovine-derived xenograft combination in bilateral sinus augmentation procedure. Platelets. 2013;24:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 57. | Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Inchingolo AD, Dipalma G, Flace P, Girolamo F, Tarullo A, Laino L. Regenerative surgery performed with platelet-rich plasma used in sinus lift elevation before dental implant surgery: an useful aid in healing and regeneration of bone tissue. Eur Rev Med Pharmacol Sci. 2012;16:1222-1226. [PubMed] |
| 58. | Poeschl PW, Ziya-Ghazvini F, Schicho K, Buchta C, Moser D, Seemann R, Ewers R, Schopper C. Application of platelet-rich plasma for enhanced bone regeneration in grafted sinus. J Oral Maxillofac Surg. 2012;70:657-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 59. | Bae JH, Kim YK, Myung SK. Effects of platelet-rich plasma on sinus bone graft: meta-analysis. J Periodontol. 2011;82:660-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 60. | Cabbar F, Güler N, Kürkcü M, Işeri U, Sençift K. The effect of bovine bone graft with or without platelet-rich plasma on maxillary sinus floor augmentation. J Oral Maxillofac Surg. 2011;69:2537-2547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 61. | Arora NS, Ramanayake T, Ren YF, Romanos GE. Platelet-rich plasma in sinus augmentation procedures: a systematic literature review: Part II. Implant Dent. 2010;19:145-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 62. | Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, Worthington H, Coulthard P. Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review. Eur J Oral Implantol. 2010;3:7-26. [PubMed] |
| 63. | Riaz R, Ravindran C. Efficacy of platelet rich plasma in sinus lift augmentation. J Maxillofac Oral Surg. 2010;9:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 64. | Taglialatela Scafati C, Taglialatela Scafati S, Aveta A, Cassese M, Vitale C. Chronic frontal sinus disease: combined use of platelet-rich plasma and calvarial bone grafts for sinus obliteration in aggressive and secondary cases. Rev Stomatol Chir Maxillofac. 2010;111:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 65. | Trindade-Suedam IK, de Morais JA, Faeda RS, Leite FR, Tosoni GM, Neto CB, Marcantonio E, Scaf G. Bioglass associated with leukocyte-poor platelet-rich plasma in the rabbit maxillary sinus: histomorphometric, densitometric, and fractal analysis. J Oral Implantol. 2010;36:333-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 66. | Bettega G, Brun JP, Boutonnat J, Cracowski JL, Quesada JL, Hegelhofer H, Drillat P, Richard MJ. Autologous platelet concentrates for bone graft enhancement in sinus lift procedure. Transfusion. 2009;49:779-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 67. | Lee CY, Rohrer MD, Prasad HS, Stover JD, Suzuki JB. Sinus grafting with a natural fluorohydroxyapatite for immediate load: a study with histologic analysis and histomorphometry. J Oral Implantol. 2009;35:164-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 68. | Smith AE, Prasad HS, Rohrer MD. Bone regeneration with autologous biomaterial; rapid induction of vital new bone in maxillary sinus floor by platelet concentrate alone at 23x baseline (PRP23x): a case report. Implant Dent. 2009;18:210-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 69. | Torres J, Tamimi F, Martinez PP, Alkhraisat MH, Linares R, Hernández G, Torres-Macho J, López-Cabarcos E. Effect of platelet-rich plasma on sinus lifting: a randomized-controlled clinical trial. J Clin Periodontol. 2009;36:677-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 70. | Aimetti M, Romano F, Dellavia C, De Paoli S. Sinus grafting using autogenous bone and platelet-rich plasma: histologic outcomes in humans. Int J Periodontics Restorative Dent. 2008;28:585-591. [PubMed] |
| 71. | Antoun H, Bouk H, Ameur G. Bilateral sinus graft with either bovine hydroxyapatite or beta tricalcium phosphate, in combination with platelet-rich plasma: a case report. Implant Dent. 2008;17:350-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 72. | Lee CY, Rohrer MD, Prasad HS. Immediate loading of the grafted maxillary sinus using platelet rich plasma and autogenous bone: a preliminary study with histologic and histomorphometric analysis. Implant Dent. 2008;17:59-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 73. | Nikolidakis D, Meijer GJ, Jansen JA. Sinus floor elevation using platelet-rich plasma and beta-tricalcium phosphate: case report and histological evaluation. Dent Today. 2008;27:66, 68, 70; quiz 71. [PubMed] |
| 74. | Pieri F, Lucarelli E, Corinaldesi G, Iezzi G, Piattelli A, Giardino R, Bassi M, Donati D, Marchetti C. Mesenchymal stem cells and platelet-rich plasma enhance bone formation in sinus grafting: a histomorphometric study in minipigs. J Clin Periodontol. 2008;35:539-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 75. | Roldán JC, Knueppel H, Schmidt C, Jepsen S, Zimmermann C, Terheyden H. Single-stage sinus augmentation with cancellous iliac bone and anorganic bovine bone in the presence of platelet-rich plasma in the miniature pig. Clin Oral Implants Res. 2008;19:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 76. | Schaaf H, Streckbein P, Lendeckel S, Heidinger KS, Rehmann P, Boedeker RH, Howaldt HP. Sinus lift augmentation using autogenous bone grafts and platelet-rich plasma: radiographic results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:673-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 77. | Schaaf H, Streckbein P, Lendeckel S, Heidinger K, Görtz B, Bein G, Boedeker RH, Schlegel KA, Howaldt HP. Topical use of platelet-rich plasma to influence bone volume in maxillary augmentation: a prospective randomized trial. Vox Sang. 2008;94:64-69. [PubMed] |
| 78. | DePoi R, John V, Paez de Mendoza CY, Gossweiler MK. Development of an oro-antral fistula following sinus elevation surgery: a case report on management using platelet-rich plasma. J Indiana Dent Assoc 2007-. 2008;86:10-16. [PubMed] |
| 79. | Consolo U, Zaffe D, Bertoldi C, Ceccherelli G. Platelet-rich plasma activity on maxillary sinus floor augmentation by autologous bone. Clin Oral Implants Res. 2007;18:252-262. [PubMed] |
| 80. | Lee HJ, Choi BH, Jung JH, Zhu SJ, Lee SH, Huh JY, You TM, Li J. Maxillary sinus floor augmentation using autogenous bone grafts and platelet-enriched fibrin glue with simultaneous implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:329-333. [PubMed] |
| 81. | Schlegel KA, Zimmermann R, Thorwarth M, Neukam FW, Klongnoi B, Nkenke E, Felszeghy E. Sinus floor elevation using autogenous bone or bone substitute combined with platelet-rich plasma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e15-e25. [PubMed] |
| 82. | Boyapati L, Wang HL. The role of platelet-rich plasma in sinus augmentation: a critical review. Implant Dent. 2006;15:160-170. [PubMed] |
| 83. | Klongnoi B, Rupprecht S, Kessler P, Thorwarth M, Wiltfang J, Schlegel KA. Influence of platelet-rich plasma on a bioglass and autogenous bone in sinus augmentation. An explorative study. Clin Oral Implants Res. 2006;17:312-320. [PubMed] |
| 84. | Trisi P, Rebaudi A, Calvari F, Lazzara RJ. Sinus graft with biogran, autogenous bone, and PRP: a report of three cases with histology and micro-CT. Int J Periodontics Restorative Dent. 2006;26:113-125. [PubMed] |
| 85. | Butterfield KJ, Bennett J, Gronowicz G, Adams D. Effect of platelet-rich plasma with autogenous bone graft for maxillary sinus augmentation in a rabbit model. J Oral Maxillofac Surg. 2005;63:370-376. [PubMed] |
| 86. | Grageda E, Lozada JL, Boyne PJ, Caplanis N, McMillan PJ. Bone formation in the maxillary sinus by using platelet-rich plasma: an experimental study in sheep. J Oral Implantol. 2005;31:2-17. [PubMed] |
| 87. | Graziani F, Ducci F, Tonelli M, El Askary AS, Monier M, Gabriele M. Maxillary sinus augmentation with platelet-rich plasma and fibrinogen cryoprecipitate: a tomographic pilot study. Implant Dent. 2005;14:63-69. [PubMed] |
| 88. | Ohya M, Yamada Y, Ozawa R, Ito K, Takahashi M, Ueda M. Sinus floor elevation applied tissue-engineered bone. Comparative study between mesenchymal stem cells/platelet-rich plasma (PRP) and autogenous bone with PRP complexes in rabbits. Clin Oral Implants Res. 2005;16:622-629. [PubMed] |
| 89. | Philippart P, Daubie V, Pochet R. Sinus grafting using recombinant human tissue factor, platelet-rich plasma gel, autologous bone, and anorganic bovine bone mineral xenograft: histologic analysis and case reports. Int J Oral Maxillofac Implants. 2005;20:274-281. [PubMed] |
| 90. | Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL, van der Wal JE, Vissink A. Does platelet-rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? Clin Oral Implants Res. 2005;16:349-356. [PubMed] |
| 91. | Steigmann M, Garg AK. A comparative study of bilateral sinus lifts performed with platelet-rich plasma alone versus alloplastic graft material reconstituted with blood. Implant Dent. 2005;14:261-266. [PubMed] |
| 92. | Mazor Z, Peleg M, Garg AK, Luboshitz J. Platelet-rich plasma for bone graft enhancement in sinus floor augmentation with simultaneous implant placement: patient series study. Implant Dent. 2004;13:65-72. [PubMed] |
| 93. | Roldán JC, Jepsen S, Schmidt C, Knüppel H, Rueger DC, Açil Y, Terheyden H. Sinus floor augmentation with simultaneous placement of dental implants in the presence of platelet-rich plasma or recombinant human bone morphogenetic protein-7. Clin Oral Implants Res. 2004;15:716-723. [PubMed] |
| 94. | Fürst G, Gruber R, Tangl S, Zechner W, Haas R, Mailath G, Sanroman F, Watzek G. Sinus grafting with autogenous platelet-rich plasma and bovine hydroxyapatite. A histomorphometric study in minipigs. Clin Oral Implants Res. 2003;14:500-508. [PubMed] |
| 95. | Maiorana C, Sommariva L, Brivio P, Sigurtà D, Santoro F. Maxillary sinus augmentation with anorganic bovine bone (Bio-Oss) and autologous platelet-rich plasma: preliminary clinical and histologic evaluations. Int J Periodontics Restorative Dent. 2003;23:227-235. [PubMed] |
| 96. | Moro G, Casini V, Bastieri A. [Use of platelet-rich plasma in major maxillary sinus augmentation]. Minerva Stomatol. 2003;52:267-271. [PubMed] |
| 97. | Jakse N, Tangl S, Gilli R, Berghold A, Lorenzoni M, Eskici A, Haas R, Pertl C. Influence of PRP on autogenous sinus grafts. An experimental study on sheep. Clin Oral Implants Res. 2003;14:578-583. [PubMed] |
| 98. | Pacifici L, Casella F, Ripari M. [Lifting of the maxillary sinus: complementary use of platelet rich plasma, autologous bone deproteinised bovine bone. Case report]. Minerva Stomatol. 2003;52:471-478. [PubMed] |
| 99. | Danesh-Meyer MJ, Filstein MR, Shanaman R. Histological evaluation of sinus augmentation using platelet rich plasma (PRP): a case series. J Int Acad Periodontol. 2001;3:48-56. [PubMed] |
| 100. | Lozada JL, Caplanis N, Proussaefs P, Willardsen J, Kammeyer G. Platelet-rich plasma application in sinus graft surgery: Part I--Background and processing techniques. J Oral Implantol. 2001;27:38-42. [PubMed] |
| 101. | Rosenberg ES, Torosian J. Sinus grafting using platelet-rich plasma--initial case presentation. Pract Periodontics Aesthet Dent. 2000;12:843-850; quiz 852. [PubMed] |
| 102. | Sonnleitner D, Huemer P, Sullivan DY. A simplified technique for producing platelet-rich plasma and platelet concentrate for intraoral bone grafting techniques: a technical note. Int J Oral Maxillofac Implants. 2000;15:879-882. [PubMed] |
| 103. | Keskiner I, Alkan A, Acikgoz G, Arpak N, Kaplan S, Arslan H. Platelet-rich plasma and autogenous bone graft combined with guided tissue regeneration in periodontal fenestration defects in dogs. Int J Periodontics Restorative Dent. 2014;34:e112-e120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 104. | Nagata MJ, de Campos N, Messora MR, Pola NM, Santinoni CS, Bomfim SR, Fucini SE, Ervolino E, de Almeida JM, Theodoro LH. Platelet-rich plasma, low-level laser therapy, or their combination promotes periodontal regeneration in fenestration defects: a preliminary in vivo study. J Periodontol. 2014;85:770-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 105. | Jeong KI, Kim SG, Oh JS, Lee SY, Cho YS, Yang SS, Park SC, You JS, Lim SC, Jeong MA. Effect of platelet-rich plasma and platelet-rich fibrin on peri-implant bone defects in dogs. J Biomed Nanotechnol. 2013;9:535-537. [PubMed] |
| 106. | Tobita M, Uysal CA, Guo X, Hyakusoku H, Mizuno H. Periodontal tissue regeneration by combined implantation of adipose tissue-derived stem cells and platelet-rich plasma in a canine model. Cytotherapy. 2013;15:1517-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 107. | Moghe S, Saini N, Moghe A. Platelet-rich plasma in periodontal defect treatment after extraction of impacted mandibular third molars. Natl J Maxillofac Surg. 2012;3:139-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 108. | Del Fabbro M, Bortolin M, Taschieri S, Weinstein R. Is platelet concentrate advantageous for the surgical treatment of periodontal diseases? A systematic review and meta-analysis. J Periodontol. 2011;82:1100-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 109. | Goyal B, Tewari S, Duhan J, Sehgal PK. Comparative evaluation of platelet-rich plasma and guided tissue regeneration membrane in the healing of apicomarginal defects: a clinical study. J Endod. 2011;37:773-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 110. | Garcia RV, Gabrielli MA, Hochuli-Vieira E, Spolidorio LC, Filho JG, Neto FA, de Cardoso LA, Shibli JA. Effect of platelet-rich plasma on peri-implant bone repair: a histologic study in dogs. J Oral Implantol. 2010;36:281-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 111. | Markou N, Pepelassi E, Kotsovilis S, Vrotsos I, Vavouraki H, Stamatakis HC. The use of platelet-rich plasma combined with demineralized freeze-dried bone allograft in the treatment of periodontal endosseous defects: a report of two clinical cases. J Am Dent Assoc. 2010;141:967-978. [PubMed] |
| 112. | Harnack L, Boedeker RH, Kurtulus I, Boehm S, Gonzales J, Meyle J. Use of platelet-rich plasma in periodontal surgery--a prospective randomised double blind clinical trial. Clin Oral Investig. 2009;13:179-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 113. | Holly D, Mracna J. The use of platelet rich plasma with guided tissue regeneration in defects caused by periodontal diseases. Bratisl Lek Listy. 2009;110:669-671. [PubMed] |
| 114. | Markou N, Pepelassi E, Vavouraki H, Stamatakis HC, Nikolopoulos G, Vrotsos I, Tsiklakis K. Treatment of periodontal endosseous defects with platelet-rich plasma alone or in combination with demineralized freeze-dried bone allograft: a comparative clinical trial. J Periodontol. 2009;80:1911-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 115. | Sammartino G, Tia M, Gentile E, Marenzi G, Claudio PP. Platelet-rich plasma and resorbable membrane for prevention of periodontal defects after deeply impacted lower third molar extraction. J Oral Maxillofac Surg. 2009;67:2369-2373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 116. | Zhao W, Wang QX, Liu WX. [Repairing of peri-implant bone defect with platelet-rich plasma and platelet-rich plasma/ osteoinduction active material composite: an experimental study in dogs]. Shanghai Kouqiang Yixue. 2009;18:307-312. [PubMed] |
| 117. | Yamamiya K, Okuda K, Kawase T, Hata K, Wolff LF, Yoshie H. Tissue-engineered cultured periosteum used with platelet-rich plasma and hydroxyapatite in treating human osseous defects. J Periodontol. 2008;79:811-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 118. | Tözüm TF, Keçeli HG. Treatment of peri-implant defect with modified sandwich bone augmentation. Case report and follow-up. N Y State Dent J. 2008;74:52-57. [PubMed] |
| 119. | Belli E, Longo B, Balestra FM. Autogenous platelet-rich plasma in combination with bovine-derived hydroxyapatite xenograft for treatment of a cystic lesion of the jaw. J Craniofac Surg. 2005;16:978-980. [PubMed] |
| 120. | Sammartino G, Tia M, Marenzi G, di Lauro AE, D’Agostino E, Claudio PP. Use of autologous platelet-rich plasma (PRP) in periodontal defect treatment after extraction of impacted mandibular third molars. J Oral Maxillofac Surg. 2005;63:766-770. [PubMed] |
| 121. | Sánchez AR, Sheridan PJ, Eckert SE, Weaver AL. Regenerative potential of platelet-rich plasma added to xenogenic bone grafts in peri-implant defects: a histomorphometric analysis in dogs. J Periodontol. 2005;76:1637-1644. [PubMed] |
| 122. | Sánchez AR, Sheridan PJ, Eckert SE, Weaver AL. Influence of platelet-rich plasma added to xenogeneic bone grafts in periimplant defects: a vital fluorescence study in dogs. Clin Implant Dent Relat Res. 2005;7:61-69. [PubMed] |
| 123. | Zhang Y, Lin Y, Qiu LX, Wang X. [Using platelet-rich plasma (PRP) to improve bone regeneration in implant bone defect]. Zhonghua Kouqiang Yixue Zazhi. 2004;39:269-272. [PubMed] |
| 124. | Shepherd N, Greenwell H, Hill M, Vidal R, Scheetz JP. Root coverage using acellular dermal matrix and comparing a coronally positioned tunnel with and without platelet-rich plasma: a pilot study in humans. J Periodontol. 2009;80:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 125. | Bashutski JD, Wang HL. Role of platelet-rich plasma in soft tissue root-coverage procedures: a review. Quintessence Int. 2008;39:473-483. [PubMed] |
| 126. | Keceli HG, Sengun D, Berberoğlu A, Karabulut E. Use of platelet gel with connective tissue grafts for root coverage: a randomized-controlled trial. J Clin Periodontol. 2008;35:255-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 127. | Huang LH, Neiva RE, Soehren SE, Giannobile WV, Wang HL. The effect of platelet-rich plasma on the coronally advanced flap root coverage procedure: a pilot human trial. J Periodontol. 2005;76:1768-1777. [PubMed] |
| 128. | Naik AR, Ramesh AV, Dwarkanath CD, Naik MS, Chinnappa AB. Use of autologous platelet rich plasma to treat gingival recession in esthetic periodontal surgery. J Indian Soc Periodontol. 2013;17:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 129. | Jovicić B, Lazić Z, Nedić M, Matijević S, Gostović-Spadijer A. Therapeutic efficacy of connective tissue autotransplants with periosteum and platelet rich plasma in the menagement of gingival recession. Vojnosanit Pregl. 2013;70:664-669. [PubMed] |
| 130. | Kumar A, Triveni MG, Mehta DS. Subepithelial connective tissue graft used with platelet-rich plasma in treatment of gingival recession. Dent Update. 2012;39:218-220. [PubMed] |
| 131. | Aleksić Z, Janković S, Dimitrijević B, Pucar A, Lazić V, Leković V. [Clinical impact of platelet rich plasma in treatment of gingival recessions]. Srp Arh Celok Lek. 2008;136:95-103. [PubMed] |
| 132. | Kontovazainitis G, Griffin TJ, Cheung WS. Treatment of gingival recession using platelet concentrate with a bioabsorbable membrane and coronally advanced flap: a report of two cases. Int J Periodontics Restorative Dent. 2008;28:301-307. [PubMed] |
| 133. | Suaid FF, Carvalho MD, Santamaria MP, Casati MZ, Nociti FH, Sallum AW, Sallum EA. Platelet-rich plasma and connective tissue grafts in the treatment of gingival recessions: a histometric study in dogs. J Periodontol. 2008;79:888-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 134. | Bajaj P, Pradeep AR, Agarwal E, Rao NS, Naik SB, Priyanka N, Kalra N. Comparative evaluation of autologous platelet-rich fibrin and platelet-rich plasma in the treatment of mandibular degree II furcation defects: a randomized controlled clinical trial. J Periodontal Res. 2013;48:573-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 135. | Suaid FF, Carvalho MD, Ambrosano GM, Nociti FH, Casati MZ, Sallum EA. Platelet-rich plasma in the treatment of Class II furcation defects: a histometrical study in dogs. J Appl Oral Sci. 2012;20:162-169. [PubMed] |
| 136. | Pradeep AR, Pai S, Garg G, Devi P, Shetty SK. A randomized clinical trial of autologous platelet-rich plasma in the treatment of mandibular degree II furcation defects. J Clin Periodontol. 2009;36:581-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 137. | Lekovic V, Camargo PM, Weinlaender M, Vasilic N, Aleksic Z, Kenney EB. Effectiveness of a combination of platelet-rich plasma, bovine porous bone mineral and guided tissue regeneration in the treatment of mandibular grade II molar furcations in humans. J Clin Periodontol. 2003;30:746-751. [PubMed] |
| 138. | Sarkarat F, Kalantar Motamedi MH, Jahanbani J, Sepehri D, Kahali R, Nematollahi Z. Platelet-Rich Plasma in Treatment of Zoledronic Acid-Induced Bisphosphonate-related Osteonecrosis of the Jaws. Trauma Mon. 2014;19:e17196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 139. | Bou Assi T, Rahme M, Saghieh S, Bou Raad Azoury N, Abdallah Hajj Hussein I, Leone A, Jurjus A. Effect of autologous platelet-rich plasma on distraction osteogenesis in the mandible of rabbits: a morphologic and morphometric approach. J Biol Regul Homeost Agents. 2013;27:177-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 140. | Dasmah A, Thor A, Ekestubbe A, Sennerby L, Rasmusson L. Marginal bone-level alterations at implants installed in block versus particulate onlay bone grafts mixed with platelet-rich plasma in atrophic maxilla. a prospective 5-year follow-up study of 15 patients. Clin Implant Dent Relat Res. 2013;15:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 141. | Messora MR, Nagata MJ, Fucini SE, Pola NM, Campos N, Oliveira GC, Bosco AF, Garcia VG, Furlaneto FA. Effect of platelet-rich plasma on the healing of mandibular defects treated with bone allograft. A radiographic study in dogs. J Oral Implantol. 2012;Sep 26; Epub ahead of print. [PubMed] |
| 142. | Korpi JT, Kainulainen VT, Sándor GK, Oikarinen KS. Long-term follow-up of severely resorbed mandibles reconstructed using tent pole technique without platelet-rich plasma. J Oral Maxillofac Surg. 2012;70:2543-2548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 143. | Brugnami F, Corsi A, Riminucci M, Caiazzo A. A case report of bilateral mandibular vertical guided bone regeneration with and without bovine thrombin/calcium chloride activated platelet-rich plasma. J Oral Implantol. 2011;37:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 144. | Arenaz-Búa J, Luaces-Rey R, Sironvalle-Soliva S, Otero-Rico A, Charro-Huerga E, Patiño-Seijas B, García-Rozado A, Ferreras-Granados J, Vázquez-Mahía I, Lorenzo-Franco F. A comparative study of platelet-rich plasma, hydroxyapatite, demineralized bone matrix and autologous bone to promote bone regeneration after mandibular impacted third molar extraction. Med Oral Patol Oral Cir Bucal. 2010;15:e483-e489. [PubMed] |
| 145. | Badr M, Coulthard P, Alissa R, Oliver R. The efficacy of platelet-rich plasma in grafted maxillae. A randomised clinical trial. Eur J Oral Implantol. 2010;3:233-244. [PubMed] |
| 146. | Gentile P, Bottini DJ, Spallone D, Curcio BC, Cervelli V. Application of platelet-rich plasma in maxillofacial surgery: clinical evaluation. J Craniofac Surg. 2010;21:900-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 147. | Schuckert KH, Jopp S, Osadnik M. Modern bone regeneration instead of bone transplantation: a combination of recombinant human bone morphogenetic protein-2 and platelet-rich plasma for the vertical augmentation of the maxillary bone-a single case report. Tissue Eng Part C Methods. 2010;16:1335-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 148. | Schuckert KH, Jopp S, Teoh SH. Mandibular defect reconstruction using three-dimensional polycaprolactone scaffold in combination with platelet-rich plasma and recombinant human bone morphogenetic protein-2: de novo synthesis of bone in a single case. Tissue Eng Part A. 2009;15:493-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 149. | Robiony M, Zorzan E, Polini F, Sembronio S, Toro C, Politi M. Osteogenesis distraction and platelet-rich plasma: combined use in restoration of severe atrophic mandible. Long-term results. Clin Oral Implants Res. 2008;19:1202-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 150. | Adornato MC, Morcos I, Rozanski J. The treatment of bisphosphonate-associated osteonecrosis of the jaws with bone resection and autologous platelet-derived growth factors. J Am Dent Assoc. 2007;138:971-977. [PubMed] |
| 151. | Curi MM, Cossolin GS, Koga DH, Araújo SR, Feher O, dos Santos MO, Zardetto C. Treatment of avascular osteonecrosis of the mandible in cancer patients with a history of bisphosphonate therapy by combining bone resection and autologous platelet-rich plasma: Report of 3 cases. J Oral Maxillofac Surg. 2007;65:349-355. [PubMed] |
| 152. | Gerard D, Carlson ER, Gotcher JE, Jacobs M. Effects of platelet-rich plasma at the cellular level on healing of autologous bone-grafted mandibular defects in dogs. J Oral Maxillofac Surg. 2007;65:721-727. [PubMed] |
| 153. | Lindeboom JA, Mathura KR, Aartman IH, Kroon FH, Milstein DM, Ince C. Influence of the application of platelet-enriched plasma in oral mucosal wound healing. Clin Oral Implants Res. 2007;18:133-139. [PubMed] |
| 154. | Rai B, Ho KH, Lei Y, Si-Hoe KM, Jeremy Teo CM, Yacob KB, Chen F, Ng FC, Teoh SH. Polycaprolactone-20% tricalcium phosphate scaffolds in combination with platelet-rich plasma for the treatment of critical-sized defects of the mandible: a pilot study. J Oral Maxillofac Surg. 2007;65:2195-2205. [PubMed] |
| 155. | Gerard D, Carlson ER, Gotcher JE, Jacobs M. Effects of platelet-rich plasma on the healing of autologous bone grafted mandibular defects in dogs. J Oral Maxillofac Surg. 2006;64:443-451. [PubMed] |
| 156. | Mannai C. Early implant loading in severely resorbed maxilla using xenograft, autograft, and platelet-rich plasma in 97 patients. J Oral Maxillofac Surg. 2006;64:1420-1426. [PubMed] |
| 157. | Thor A, Wannfors K, Sennerby L, Rasmusson L. Reconstruction of the severely resorbed maxilla with autogenous bone, platelet-rich plasma, and implants: 1-year results of a controlled prospective 5-year study. Clin Implant Dent Relat Res. 2005;7:209-220. [PubMed] |
| 158. | Fennis JP, Stoelinga PJ, Jansen JA. Mandibular reconstruction: a histological and histomorphometric study on the use of autogenous scaffolds, particulate cortico-cancellous bone grafts and platelet rich plasma in goats. Int J Oral Maxillofac Surg. 2004;33:48-55. [PubMed] |
| 159. | Merkx MA, Fennis JP, Verhagen CM, Stoelinga PJ. Reconstruction of the mandible using preshaped 2.3 mm titanium plates, autogenous particulate cortico-cancellous bone grafts and platelet rich plasma: a report on eight patients. Int J Oral Maxillofac Surg. 2004;33:733-739. [PubMed] |
| 160. | Fennis JP, Stoelinga PJ, Jansen JA. Mandibular reconstruction: a clinical and radiographic animal study on the use of autogenous scaffolds and platelet-rich plasma. Int J Oral Maxillofac Surg. 2002;31:281-286. [PubMed] |
| 161. | Bezgin T, Yilmaz AD, Celik BN, Kolsuz ME, Sonmez H. Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. J Endod. 2015;41:36-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 162. | Albanese A, Licata ME, Polizzi B, Campisi G. Platelet-rich plasma (PRP) in dental and oral surgery: from the wound healing to bone regeneration. Immun Ageing. 2013;10:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 163. | Georgakopoulos I, Tsantis S, Georgakopoulos P, Korfiatis P, Fanti E, Martelli M, Costaridou L, Petsas T, Panayiotakis G, Martelli FS. The impact of Platelet Rich Plasma (PRP) in osseointegration of oral implants in dental panoramic radiography: texture based evaluation. Clin Cases Miner Bone Metab. 2014;11:59-66. [PubMed] |
| 164. | Hiremath H, Motiwala T, Jain P, Kulkarni S. Use of second-generation platelet concentrate (platelet-rich fibrin) and hydroxyapatite in the management of large periapical inflammatory lesion: a computed tomography scan analysis. Indian J Dent Res. 2014;25:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 165. | Jadhav GR, Shah N, Logani A. Platelet-rich plasma supplemented revascularization of an immature tooth associated with a periapical lesion in a 40-year-old man. Case Rep Dent. 2014;2014:479584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 166. | Kundu R, Rathee M. Effect of Platelet-Rich-Plasma (PRP) and Implant Surface Topography on Implant Stability and Bone. J Clin Diagn Res. 2014;8:ZC26-ZC30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 167. | Ortolani E, Guerriero M, Coli A, Di Giannuario A, Minniti G, Polimeni A. Effect of PDGF, IGF-1 and PRP on the implant osseointegration. An histological and immunohistochemical study in rabbits. Ann Stomatol (Roma). 2014;5:66-68. [PubMed] |
| 168. | Sachdeva GS, Sachdeva LT, Goel M, Bala S. Regenerative endodontic treatment of an immature tooth with a necrotic pulp and apical periodontitis using platelet-rich plasma (PRP) and mineral trioxide aggregate (MTA): a case report. Int Endod J. 2014;Nov 4; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 169. | Streckbein P, Kleis W, Buch RS, Hansen T, Weibrich G. Bone healing with or without platelet-rich plasma around four different dental implant surfaces in beagle dogs. Clin Implant Dent Relat Res. 2014;16:479-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 170. | Zhang DD, Chen X, Bao ZF, Chen M, Ding ZJ, Zhong M. Histologic comparison between platelet-rich plasma and blood clot in regenerative endodontic treatment: an animal study. J Endod. 2014;40:1388-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 171. | Martin G, Ricucci D, Gibbs JL, Lin LM. Histological findings of revascularized/revitalized immature permanent molar with apical periodontitis using platelet-rich plasma. J Endod. 2013;39:138-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 192] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 172. | Zhu W, Zhu X, Huang GT, Cheung GS, Dissanayaka WL, Zhang C. Regeneration of dental pulp tissue in immature teeth with apical periodontitis using platelet-rich plasma and dental pulp cells. Int Endod J. 2013;46:962-970. [PubMed] |
| 173. | Torabinejad M, Faras H. A clinical and histological report of a tooth with an open apex treated with regenerative endodontics using platelet-rich plasma. J Endod. 2012;38:864-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 174. | Johns DA, Vidyanath S. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: a case report. J Endod. 2011;37:743; author reply 743-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 175. | Torabinejad M, Turman M. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: a case report. J Endod. 2011;37:265-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 181] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 176. | Vaishnavi C, Mohan B, Narayanan LL. Treatment of endodontically induced periapical lesions using hydroxyapatite, platelet-rich plasma, and a combination of both: An in vivo study. J Conserv Dent. 2011;14:140-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 177. | Singh S. Management of an endo perio lesion in a maxillary canine using platelet-rich plasma concentrate and an alloplastic bone substitute. J Indian Soc Periodontol. 2009;13:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 178. | Leventis MD, Eleftheriadis E, Oikonomopoulou P, Vavouraki H, Khaldi L, Tosios KI, Vardas E, Valavanis KD, Dontas I. Experimental study of the effect of autologous platelet-rich plasma on the early phases of osteoinduction by allogenic demineralized bone matrix. Implant Dent. 2012;21:399-405. [PubMed] |
| 179. | Malik A, Shaari R, Rahman SA, Aljuboori MJ. Influence of platelet-rich plasma on dental implants. Osseointegration in well-controlled diabetic patients. Dent Implantol Update. 2012;23:89-96. [PubMed] |
| 180. | Baeyens W, Glineur R, Evrard L. [The use of platelet concentrates: platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in bone reconstruction prior to dental implant surgery]. Rev Med Brux. 2010;31:521-527. [PubMed] |
| 181. | Duka M, Lazić Z, Bubalo M. [Effect of local administration of platelet-rich plasma and guided tissue regeneration on the level of bone resorption in early dental implant insertion]. Vojnosanit Pregl. 2008;65:462-468. [PubMed] |
| 182. | Nikolidakis D, van den Dolder J, Wolke JG, Jansen JA. Effect of platelet-rich plasma on the early bone formation around Ca-P-coated and non-coated oral implants in cortical bone. Clin Oral Implants Res. 2008;19:207-213. [PubMed] |
| 183. | Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Implants Res. 2008;19:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 172] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 184. | Schwartz-Arad D, Levin L, Aba M. [The use of platelet rich plasma (PRP) and platelet rich fibrin (PRP) extracts in dental implantology and oral surgery]. Refuat Hapeh Vehashinayim. 2007;24:51-55, 84. [PubMed] |
| 185. | You TM, Choi BH, Li J, Jung JH, Lee HJ, Lee SH, Jeong SM. The effect of platelet-rich plasma on bone healing around implants placed in bone defects treated with Bio-Oss: a pilot study in the dog tibia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e8-12. [PubMed] |
| 186. | Ito K, Yamada Y, Naiki T, Ueda M. Simultaneous implant placement and bone regeneration around dental implants using tissue-engineered bone with fibrin glue, mesenchymal stem cells and platelet-rich plasma. Clin Oral Implants Res. 2006;17:579-586. [PubMed] |
| 187. | John V, Gossweiler M. Implant treatment and the role of platelet rich plasma. J Indiana Dent Assoc. 2003;82:8-13. [PubMed] |
| 188. | Thor A. Reconstruction of the anterior maxilla with platelet gel, autogenous bone, and titanium mesh: a case report. Clin Implant Dent Relat Res. 2002;4:150-155. [PubMed] |
| 189. | Barona-Dorado C, González-Regueiro I, Martín-Ares M, Arias-Irimia O, Martínez-González JM. Efficacy of platelet-rich plasma applied to post-extraction retained lower third molar alveoli. A systematic review. Med Oral Patol Oral Cir Bucal. 2014;19:e142-e148. [PubMed] |
| 190. | Cheah CW, Vaithilingam RD, Siar CH, Swaminathan D, Hornbuckle GC. Histologic, histomorphometric, and cone-beam computerized tomography analyses of calcium sulfate and platelet-rich plasma in socket preservation: a pilot study. Implant Dent. 2014;23:593-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 191. | Geurs N, Ntounis A, Vassilopoulos P, Van der Velden U, Loos BG, Reddy M. Using growth factors in human extraction sockets: a histologic and histomorphometric evaluation of short-term healing. Int J Oral Maxillofac Implants. 2014;29:485-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 192. | Hatakeyama I, Marukawa E, Takahashi Y, Omura K. Effects of platelet-poor plasma, platelet-rich plasma, and platelet-rich fibrin on healing of extraction sockets with buccal dehiscence in dogs. Tissue Eng Part A. 2014;20:874-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 193. | Mozzati M, Gallesio G, di Romana S, Bergamasco L, Pol R. Efficacy of plasma-rich growth factor in the healing of postextraction sockets in patients affected by insulin-dependent diabetes mellitus. J Oral Maxillofac Surg. 2014;72:456-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 194. | Kaur P, Maria A. Efficacy of platelet rich plasma and hydroxyapatite crystals in bone regeneration after surgical removal of mandibular third molars. J Maxillofac Oral Surg. 2013;12:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 195. | Kutkut A, Andreana S, Monaco E. Clinical and radiographic evaluation of single-tooth dental implants placed in grafted extraction sites: a one-year report. J Int Acad Periodontol. 2013;15:113-124. [PubMed] |
| 196. | Kutkut A, Andreana S, Kim HL, Monaco E. Extraction socket preservation graft before implant placement with calcium sulfate hemihydrate and platelet-rich plasma: a clinical and histomorphometric study in humans. J Periodontol. 2012;83:401-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 197. | Del Fabbro M, Bortolin M, Taschieri S. Is autologous platelet concentrate beneficial for post-extraction socket healing? A systematic review. Int J Oral Maxillofac Surg. 2011;40:891-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 198. | Reichert da Silva Assunção L, Colenci R, Ferreira do-Amaral CC, Sonoda CK, Mogami Bomfim SR, Okamoto R, de Assis Golim M, Deffune E, Percinoto C, Penha de Oliveira SH. Periodontal tissue engineering after tooth replantation. J Periodontol. 2011;82:758-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 199. | Alissa R, Esposito M, Horner K, Oliver R. The influence of platelet-rich plasma on the healing of extraction sockets: an explorative randomised clinical trial. Eur J Oral Implantol. 2010;3:121-134. [PubMed] |
| 200. | Rutkowski JL, Johnson DA, Radio NM, Fennell JW. Platelet rich plasma to facilitate wound healing following tooth extraction. J Oral Implantol. 2010;36:11-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 201. | Camarini ET, Zanoni JN, Leite PC, Boos FB. Use of biomaterials with or without platelet-rich plasma in postextraction sites: a microscopic study in dogs. Int J Oral Maxillofac Implants. 2009;24:432-438. [PubMed] |
| 202. | Pessoa RS, Oliveira SR, Menezes HH, de Magalhaes D. Effects of platelet-rich plasma on healing of alveolar socket: split-mouth histological and histometric evaluation in Cebus apella monkeys. Indian J Dent Res. 2009;20:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 203. | Vivek GK, Sripathi Rao BH. Potential for osseous regeneration of platelet rich plasma: a comparitive study in mandibular third molar sockets. J Maxillofac Oral Surg. 2009;8:308-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 204. | Gürbüzer B, Pikdöken L, Urhan M, Süer BT, Narin Y. Scintigraphic evaluation of early osteoblastic activity in extraction sockets treated with platelet-rich plasma. J Oral Maxillofac Surg. 2008;66:2454-2460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 205. | Rutkowski JL, Fennell JW, Kern JC, Madison DE, Johnson DA. Inhibition of alveolar osteitis in mandibular tooth extraction sites using platelet-rich plasma. J Oral Implantol. 2007;33:116-121. [PubMed] |
| 206. | Antonello Gde M, Torres do Couto R, Giongo CC, Corrêa MB, Chagas Júnior OL, Lemes CH. Evaluation of the effects of the use of platelet-rich plasma (PRP) on alveolar bone repair following extraction of impacted third molars: prospective study. J Craniomaxillofac Surg. 2013;41:e70-e75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 207. | Findik Y, Baykul T. Secondary closure of alveolar clefts with mandibular symphyseal bone grafts and with platelet-rich fibrin under local anesthesia: three case reports. J Contemp Dent Pract. 2013;14:751-753. [PubMed] |
| 208. | Kim JS, Jeong MH, Jo JH, Kim SG, Oh JS. Clinical application of platelet-rich fibrin by the application of the Double J technique during implant placement in alveolar bone defect areas: case reports. Implant Dent. 2013;22:244-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 209. | Sclar AG, Best SP. The combined use of rhBMP-2/ACS, autogenous bone graft, a bovine bone mineral biomaterial, platelet-rich plasma, and guided bone regeneration at nonsubmerged implant placement for supracrestal bone augmentation. A case report. Int J Oral Maxillofac Implants. 2013;28:e272-e276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 210. | Célio-Mariano R, de Melo WM, Carneiro-Avelino C. Comparative radiographic evaluation of alveolar bone healing associated with autologous platelet-rich plasma after impacted mandibular third molar surgery. J Oral Maxillofac Surg. 2012;70:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 211. | Marukawa E, Oshina H, Iino G, Morita K, Omura K. Reduction of bone resorption by the application of platelet-rich plasma (PRP) in bone grafting of the alveolar cleft. J Craniomaxillofac Surg. 2011;39:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 212. | Luaces-Rey R, Arenaz-Búa J, Lopez-Cedrún-Cembranos JL, Herrero-Patiño S, Sironvalle-Soliva S, Iglesias-Candal E, Pombo-Castro M. Is PRP useful in alveolar cleft reconstruction? Platelet-rich plasma in secondary alveoloplasty. Med Oral Patol Oral Cir Bucal. 2010;15:e619-e623. [PubMed] |
| 213. | Torres J, Tamimi F, Alkhraisat MH, Manchón A, Linares R, Prados-Frutos JC, Hernández G, López Cabarcos E. Platelet-rich plasma may prevent titanium-mesh exposure in alveolar ridge augmentation with anorganic bovine bone. J Clin Periodontol. 2010;37:943-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 214. | Lee C, Nishihara K, Okawachi T, Iwashita Y, Majima HJ, Nakamura N. A quantitative radiological assessment of outcomes of autogenous bone graft combined with platelet-rich plasma in the alveolar cleft. Int J Oral Maxillofac Surg. 2009;38:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 215. | Pieri F, Lucarelli E, Corinaldesi G, Fini M, Aldini NN, Giardino R, Donati D, Marchetti C. Effect of mesenchymal stem cells and platelet-rich plasma on the healing of standardized bone defects in the alveolar ridge: a comparative histomorphometric study in minipigs. J Oral Maxillofac Surg. 2009;67:265-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 216. | Rullo R, Festa VM, Guida L, Laino G. Bone grafting with platelet-rich plasma in alveolar cleft. Case report. Minerva Stomatol. 2007;56:63-71. [PubMed] |
| 217. | Shi B, Zhou Y, Wang YN, Cheng XR. Alveolar ridge preservation prior to implant placement with surgical-grade calcium sulfate and platelet-rich plasma: a pilot study in a canine model. Int J Oral Maxillofac Implants. 2007;22:656-665. [PubMed] |
| 218. | Méndez R, López-Cedrún JL, Patiño B, Vázquez I, Martín-Sastre R, Tellado MG, Vela D. [Platelet-rich plasma (platelet gel) in secondary alveoloplasty in cleft patients]. Cir Pediatr. 2006;19:23-26. [PubMed] |
| 219. | Simon Z, Friedlich J. The use of autogenous bone grafting with platelet-rich plasma for alveolar ridge reconstruction: a clinical report. J Calif Dent Assoc. 2006;34:895-899. [PubMed] |
| 220. | Oyama T, Nishimoto S, Takeda M. Alveolar bone regeneration utilizing b-TCP and platelet-rich plasma (PRP) derived from bone marrow aspirate. Ann Plast Surg. 2005;54:222-223. [PubMed] |
| 221. | Oyama T, Nishimoto S, Tsugawa T, Shimizu F. Efficacy of platelet-rich plasma in alveolar bone grafting. J Oral Maxillofac Surg. 2004;62:555-558. [PubMed] |
| 222. | Wojtowicz A, Chaberek S, Kryst L, Urbanowska E, Ciechowicz K, Ostrowski K. Fourier and fractal analysis of maxillary alveolar ridge repair using platelet rich plasma (PRP) and inorganic bovine bone. Int J Oral Maxillofac Surg. 2003;32:84-86. [PubMed] |
| 223. | Kassolis JD, Rosen PS, Reynolds MA. Alveolar ridge and sinus augmentation utilizing platelet-rich plasma in combination with freeze-dried bone allograft: case series. J Periodontol. 2000;71:1654-1661. [PubMed] |
| 224. | Choi BH, Zhu SJ, Kim BY, Huh JY, Lee SH, Jung JH. Effect of platelet-rich plasma (PRP) concentration on the viability and proliferation of alveolar bone cells: an in vitro study. Int J Oral Maxillofac Surg. 2005;34:420-424. [PubMed] |
| 225. | Halper J. Advances in the use of growth factors for treatment of disorders of soft tissues. Adv Exp Med Biol. 2014;802:59-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 226. | Horimizu M, Kawase T, Nakajima Y, Okuda K, Nagata M, Wolff LF, Yoshie H. An improved freeze-dried PRP-coated biodegradable material suitable for connective tissue regenerative therapy. Cryobiology. 2013;66:223-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 227. | Roffi A, Filardo G, Kon E, Marcacci M. Does PRP enhance bone integration with grafts, graft substitutes, or implants? A systematic review. BMC Musculoskelet Disord. 2013;14:330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 228. | Pantou AL, Markopoulou CE, Dereka XE, Vavouraki H, Mamalis A, Vrotsos IA. The effect of platelet-rich plasma (PRP) combined with a bone allograft on human periodontal ligament (PDL) cells. Cell Tissue Bank. 2012;13:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 229. | Yamada Y, Ueda M, Hibi H, Baba S. A novel approach to periodontal tissue regeneration with mesenchymal stem cells and platelet-rich plasma using tissue engineering technology: A clinical case report. Int J Periodontics Restorative Dent. 2006;26:363-369. [PubMed] |
| 230. | Dugrillon A, Eichler H, Kern S, Klüter H. Autologous concentrated platelet-rich plasma (cPRP) for local application in bone regeneration. Int J Oral Maxillofac Surg. 2002;31:615-619. [PubMed] |
| 231. | Petrungaro PS. Using platelet-rich plasma to accelerate soft tissue maturation in esthetic periodontal surgery. Compend Contin Educ Dent. 2001;22:729-732, 734, 736 passim; quiz 746. [PubMed] |
| 232. | Suchánková Kleplová T, Soukup T, Řeháček V, Suchánek J. Human Plasma and Human Platelet-rich Plasma as a Substitute for Fetal Calf Serum during Long-term Cultivation of Mesenchymal Dental Pulp Stem Cells. Acta Medica (Hradec Kralove). 2015;57:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 233. | Lee UL, Jeon SH, Park JY, Choung PH. Effect of platelet-rich plasma on dental stem cells derived from human impacted third molars. Regen Med. 2011;6:67-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 234. | Creeper F, Lichanska AM, Marshall RI, Seymour GJ, Ivanovski S. The effect of platelet-rich plasma on osteoblast and periodontal ligament cell migration, proliferation and differentiation. J Periodontal Res. 2009;44:258-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 235. | Pepelassi EA, Markopoulou CE, Dereka XE, Mamalis AA, Vrotsos IA, Koutsilieris M. Platelet-rich plasma effect on periodontally affected human gingival fibroblasts: an in vitro study. J Int Acad Periodontol. 2009;11:160-168. [PubMed] |
| 236. | Chang T, Liu Q, Marino V, Bartold PM. Attachment of periodontal fibroblasts to barrier membranes coated with platelet-rich plasma. Aust Dent J. 2007;52:227-233. [PubMed] |
| 237. | Oliva A, Passaro I, Di Pasquale R, Di Feo A, Criscuolo M, Zappia V, Della Ragione F, D’Amato S, Annunziata M, Guida L. Ex vivo expansion of bone marrow stromal cells by platelet-rich plasma: a promising strategy in maxillo-facial surgery. Int J Immunopathol Pharmacol. 2005;18:47-53. [PubMed] |
| 238. | Gupta SJ, Jhingran R, Gupta V, Bains VK, Madan R, Rizvi I. Efficacy of platelet-rich fibrin vs. enamel matrix derivative in the treatment of periodontal intrabony defects: a clinical and cone beam computed tomography study. J Int Acad Periodontol. 2014;16:86-96. [PubMed] |
| 239. | Panda S, Jayakumar ND, Sankari M, Varghese SS, Kumar DS. Platelet rich fibrin and xenograft in treatment of intrabony defect. Contemp Clin Dent. 2014;5:550-554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 240. | Panda S, Doraiswamy J, Malaiappan S, Varghese SS, Del Fabbro M. Additive effect of autologous platelet concentrates in treatment of intrabony defects: a systematic review and meta-analysis. J Investig Clin Dent. 2014;Jul 22; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 241. | Panda S, Ramamoorthi S, Jayakumar ND, Sankari M, Varghese SS. Platelet rich fibrin and alloplast in the treatment of intrabony defect. J Pharm Bioallied Sci. 2014;6:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 242. | Bansal C, Bharti V. Evaluation of efficacy of autologous platelet-rich fibrin with demineralized-freeze dried bone allograft in the treatment of periodontal intrabony defects. J Indian Soc Periodontol. 2013;17:361-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 243. | Lekovic V, Milinkovic I, Aleksic Z, Jankovic S, Stankovic P, Kenney EB, Camargo PM. Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J Periodontal Res. 2012;47:409-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 244. | Shivashankar VY, Johns DA, Vidyanath S, Sam G. Combination of platelet rich fibrin, hydroxyapatite and PRF membrane in the management of large inflammatory periapical lesion. J Conserv Dent. 2013;16:261-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 245. | Bambal D, Manwar NU, Chandak M, Rudagi K. A comparative evaluation of the healing ability of bilateral periapical lesions treated with and without the use of platelet-rich fibrin. Todays FDA. 2012;24:54-57. [PubMed] |
| 246. | Jayalakshmi KB, Agarwal S, Singh MP, Vishwanath BT, Krishna A, Agrawal R. Platelet-Rich Fibrin with β-Tricalcium Phosphate-A Noval Approach for Bone Augmentation in Chronic Periapical Lesion: A Case Report. Case Rep Dent. 2012;2012:902858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 247. | Ali S, Bakry SA, Abd-Elhakam H, Choi BH. Platelet rich fibrin in maxillary sinus augmentation: A systematic review. J Oral Implantol. 2014;Dec 23; Epub ahead of print. [PubMed] |
| 248. | Xuan F, Lee CU, Son JS, Jeong SM, Choi BH. A comparative study of the regenerative effect of sinus bone grafting with platelet-rich fibrin-mixed Bio-Oss® and commercial fibrin-mixed Bio-Oss®: an experimental study. J Craniomaxillofac Surg. 2014;42:e47-e50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 249. | Bölükbaşı N, Ersanlı S, Keklikoğlu N, Başeğmez C, Ozdemir T. Sinus augmentation with platelet-rich fibrin in combination with bovine bone graft versus bovine bone graft in combination with collagen membrane. J Oral Implantol. 2013;Sep 16; Epub ahead of print. [PubMed] |
| 250. | Tajima N, Ohba S, Sawase T, Asahina I. Evaluation of sinus floor augmentation with simultaneous implant placement using platelet-rich fibrin as sole grafting material. Int J Oral Maxillofac Implants. 2013;28:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 251. | Toffler M, Toscano N, Holtzclaw D. Osteotome-mediated sinus floor elevation using only platelet-rich fibrin: an early report on 110 patients. Implant Dent. 2010;19:447-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 252. | Kim BJ, Kwon TK, Baek HS, Hwang DS, Kim CH, Chung IK, Jeong JS, Shin SH. A comparative study of the effectiveness of sinus bone grafting with recombinant human bone morphogenetic protein 2-coated tricalcium phosphate and platelet-rich fibrin-mixed tricalcium phosphate in rabbits. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:583-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 253. | Zhang Y, Tangl S, Huber CD, Lin Y, Qiu L, Rausch-Fan X. Effects of Choukroun’s platelet-rich fibrin on bone regeneration in combination with deproteinized bovine bone mineral in maxillary sinus augmentation: a histological and histomorphometric study. J Craniomaxillofac Surg. 2012;40:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 254. | Simonpieri A, Choukroun J, Del Corso M, Sammartino G, Dohan Ehrenfest DM. Simultaneous sinus-lift and implantation using microthreaded implants and leukocyte- and platelet-rich fibrin as sole grafting material: a six-year experience. Implant Dent. 2011;20:2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 255. | Mazor Z, Horowitz RA, Del Corso M, Prasad HS, Rohrer MD, Dohan Ehrenfest DM. Sinus floor augmentation with simultaneous implant placement using Choukroun’s platelet-rich fibrin as the sole grafting material: a radiologic and histologic study at 6 months. J Periodontol. 2009;80:2056-2064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 178] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 256. | Diss A, Dohan DM, Mouhyi J, Mahler P. Osteotome sinus floor elevation using Choukroun’s platelet-rich fibrin as grafting material: a 1-year prospective pilot study with microthreaded implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:572-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 257. | P A, Patil P, Kumar R V, Kripal K. Role and Efficacy of L-PRFmatrix in the Regeneration of Periodontal Defect: A New Perspective. J Clin Diagn Res. 2014;8:ZD03-ZD05. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 258. | Ranganathan AT, Chandran CR. Platelet-rich fibrin in the treatment of periodontal bone defects. J Contemp Dent Pract. 2014;15:372-375. [PubMed] |
| 259. | Desarda HM, Gurav AN, Gaikwad SP, Inamdar SP. Platelet rich fibrin: a new hope for regeneration in aggressive periodontitis patients: report of two cases. Indian J Dent Res. 2013;24:627-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 260. | Lee JW, Kim SG, Kim JY, Lee YC, Choi JY, Dragos R, Rotaru H. Restoration of a peri-implant defect by platelet-rich fibrin. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 261. | Ruga E, Gallesio C, Boffano P. Platelet-rich fibrin and piezoelectric surgery: a safe technique for the prevention of periodontal complications in third molar surgery. J Craniofac Surg. 2011;22:1951-1955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 262. | Jang ES, Park JW, Kweon H, Lee KG, Kang SW, Baek DH, Choi JY, Kim SG. Restoration of peri-implant defects in immediate implant installations by Choukroun platelet-rich fibrin and silk fibroin powder combination graft. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:831-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 263. | Hao PJ, Wang ZG, Xu QC, Xu S, Li ZR, Yang PS, Liu ZH. Effect of umbilical cord mesenchymal stem cell in peri-implant bone defect after immediate implant: an experiment study in beagle dogs. Int J Clin Exp Med. 2014;7:4131-4138. [PubMed] |
| 264. | Agarwal K, Chandra C, Agarwal K, Kumar N. Lateral sliding bridge flap technique along with platelet rich fibrin and guided tissue regeneration for root coverage. J Indian Soc Periodontol. 2013;17:801-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 265. | Eren G, Atilla G. Platelet-rich fibrin in the treatment of localized gingival recessions: a split-mouth randomized clinical trial. Clin Oral Investig. 2014;18:1941-1948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 266. | Aleksić Z, Janković S, Dimitrijević B, Divnić-Resnik T, Milinković I, Leković V. [The use of platelet-rich fibrin membrane in gingival recession treatment]. Srp Arh Celok Lek. 2010;138:11-18. [PubMed] |
| 267. | Sambhav J, Rohit R, Ranjana M, Shalabh M. Platelet rich fibrin (Prf) and β-tricalcium phosphate with coronally advanced flap for the management of grade-II furcation defect. Ethiop J Health Sci. 2014;24:269-272. [PubMed] |
| 268. | Tatullo M, Marrelli M, Cassetta M, Pacifici A, Stefanelli LV, Scacco S, Dipalma G, Pacifici L, Inchingolo F. Platelet Rich Fibrin (P.R.F.) in reconstructive surgery of atrophied maxillary bones: clinical and histological evaluations. Int J Med Sci. 2012;9:872-880. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 269. | Sharma A, Pradeep AR. Autologous platelet-rich fibrin in the treatment of mandibular degree II furcation defects: a randomized clinical trial. J Periodontol. 2011;82:1396-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 270. | Dincă O, Zurac S, Stăniceanu F, Bucur MB, Bodnar DC, Vlădan C, Bucur A. Clinical and histopathological studies using fibrin-rich plasma in the treatment of bisphosphonate-related osteonecrosis of the jaw. Rom J Morphol Embryol. 2014;55:961-964. [PubMed] |
| 271. | Kim JW, Kim SJ, Kim MR. Leucocyte-rich and platelet-rich fibrin for the treatment of bisphosphonate-related osteonecrosis of the jaw: a prospective feasibility study. Br J Oral Maxillofac Surg. 2014;52:854-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 272. | Soydan SS, Uckan S. Management of bisphosphonate-related osteonecrosis of the jaw with a platelet-rich fibrin membrane: technical report. J Oral Maxillofac Surg. 2014;72:322-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 273. | Liao HT, Chen CT, Chen CH, Chen JP, Tsai JC. Combination of guided osteogenesis with autologous platelet-rich fibrin glue and mesenchymal stem cell for mandibular reconstruction. J Trauma. 2011;70:228-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 274. | Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Scacco S, Inchingolo AD, Dipalma G, Vermesan D, Abbinante A, Cagiano R. Trial with Platelet-Rich Fibrin and Bio-Oss used as grafting materials in the treatment of the severe maxillar bone atrophy: clinical and radiological evaluations. Eur Rev Med Pharmacol Sci. 2010;14:1075-1084. [PubMed] |
| 275. | Simonpieri A, Del Corso M, Sammartino G, Dohan Ehrenfest DM. The relevance of Choukroun’s platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft. Part II: implant surgery, prosthodontics, and survival. Implant Dent. 2009;18:220-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 276. | Kuz’minykh IA. [Clinical experience in osteoplastic material Allomatrix-implant and fibrin rich platelets use in surgical treatment of jaw radicular cysts]. Stomatologiia (Mosk). 2009;88:51-53. [PubMed] |
| 277. | Nagaveni NB, Kumari KN, Poornima P, Reddy V. Management of an endo-perio lesion in an immature tooth using autologous platelet-rich fibrin: a case report. J Indian Soc Pedod Prev Dent. 2015;33:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 278. | Davis VL, Abukabda AB, Radio NM, Witt-Enderby PA, Clafshenkel WP, Cairone JV, Rutkowski JL. Platelet-rich preparations to improve healing. Part II: platelet activation and enrichment, leukocyte inclusion, and other selection criteria. J Oral Implantol. 2014;40:511-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 279. | Goyal L. Clinical effectiveness of combining platelet rich fibrin with alloplastic bone substitute for the management of combined endodontic periodontal lesion. Restor Dent Endod. 2014;39:51-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 280. | Hotwani K, Sharma K. Platelet rich fibrin - a novel acumen into regenerative endodontic therapy. Restor Dent Endod. 2014;39:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 281. | Nacopoulos C, Dontas I, Lelovas P, Galanos A, Vesalas AM, Raptou P, Mastoris M, Chronopoulos E, Papaioannou N. Enhancement of bone regeneration with the combination of platelet-rich fibrin and synthetic graft. J Craniofac Surg. 2014;25:2164-2168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 282. | Khetarpal A, Chaudhry S, Talwar S, Verma M. Endodontic management of open apex using MTA and platelet - rich fibrin membrane barrier: A newer matrix concept. J Clin Exp Dent. 2013;5:e291-e294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 283. | Li Q, Pan S, Dangaria SJ, Gopinathan G, Kolokythas A, Chu S, Geng Y, Zhou Y, Luan X. Platelet-rich fibrin promotes periodontal regeneration and enhances alveolar bone augmentation. Biomed Res Int. 2013;2013:638043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 284. | Mishra N, Narang I, Mittal N. Platelet-rich fibrin-mediated revitalization of immature necrotic tooth. Contemp Clin Dent. 2013;4:412-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 285. | Del Corso M, Mazor Z, Rutkowski JL, Dohan Ehrenfest DM. The use of leukocyte- and platelet-rich fibrin during immediate postextractive implantation and loading for the esthetic replacement of a fractured maxillary central incisor. J Oral Implantol. 2012;38:181-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 286. | Peck MT, Marnewick J, Stephen LX, Singh A, Patel N, Majeed A. The use of leukocyte- and platelet-rich fibrin (L-PRF) to facilitate implant placement in bone-deficient sites: a report of two cases. SADJ. 2012;67:54-56, 58-59. [PubMed] |
| 287. | Rudagi KB, Rudagi B. One-step apexification in immature tooth using grey mineral trioxide aggregate as an apical barrier and autologus platelet rich fibrin membrane as an internal matrix. J Conserv Dent. 2012;15:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 288. | Shivashankar VY, Johns DA, Vidyanath S, Kumar MR. Platelet Rich Fibrin in the revitalization of tooth with necrotic pulp and open apex. J Conserv Dent. 2012;15:395-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 289. | Karunakar P, Prasanna JS, Jayadev M, Shravani GS. Platelet-rich fibrin, “a faster healing aid” in the treatment of combined lesions: A report of two cases. J Indian Soc Periodontol. 2014;18:651-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 290. | Johns DA, Shivashankar VY, Krishnamma S, Johns M. Use of photoactivated disinfection and platelet-rich fibrin in regenerative Endodontics. J Conserv Dent. 2014;17:487-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 291. | Sam G, Shivashankar VY. Management of a pathologically migrated upper anterior tooth using platelet-rich fibrin and a modified crown preparation technique. J Indian Soc Periodontol. 2014;18:786-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 292. | Kumar RV, Shubhashini N. Platelet rich fibrin: a new paradigm in periodontal regeneration. Cell Tissue Bank. 2013;14:453-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 293. | Saluja H, Dehane V, Mahindra U. Platelet-Rich fibrin: A second generation platelet concentrate and a new friend of oral and maxillofacial surgeons. Ann Maxillofac Surg. 2011;1:53-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 294. | Sammartino G, Dohan Ehrenfest DM, Carile F, Tia M, Bucci P. Prevention of hemorrhagic complications after dental extractions into open heart surgery patients under anticoagulant therapy: the use of leukocyte- and platelet-rich fibrin. J Oral Implantol. 2011;37:681-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 295. | Joseph V R, Sam G, Amol NV. Clinical evaluation of autologous platelet rich fibrin in horizontal alveolar bony defects. J Clin Diagn Res. 2014;8:ZC43-ZC47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 296. | Baslarli O, Tumer C, Ugur O, Vatankulu B. Evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. Med Oral Patol Oral Cir Bucal. 2015;20:e111-e116. [PubMed] |
| 297. | Barone A, Ricci M, Romanos GE, Tonelli P, Alfonsi F, Covani U. Buccal bone deficiency in fresh extraction sockets: a prospective single cohort study. Clin Oral Implants Res. 2014;Mar 31; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 298. | Hauser F, Gaydarov N, Badoud I, Vazquez L, Bernard JP, Ammann P. Clinical and histological evaluation of postextraction platelet-rich fibrin socket filling: a prospective randomized controlled study. Implant Dent. 2013;22:295-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 299. | Girish Rao S, Bhat P, Nagesh KS, Rao GH, Mirle B, Kharbhari L, Gangaprasad B. Bone regeneration in extraction sockets with autologous platelet rich fibrin gel. J Maxillofac Oral Surg. 2013;12:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 300. | Zhao JH, Tsai CH, Chang YC. Clinical and histologic evaluations of healing in an extraction socket filled with platelet-rich fibrin. J Dent Sci. 2011;6:116-122. [RCA] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 301. | Simon BI, Gupta P, Tajbakhsh S. Quantitative evaluation of extraction socket healing following the use of autologous platelet-rich fibrin matrix in humans. Int J Periodontics Restorative Dent. 2011;31:285-295. [PubMed] |
| 302. | Gürbüzer B, Pikdöken L, Tunali M, Urhan M, Küçükodaci Z, Ercan F. Scintigraphic evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. J Oral Maxillofac Surg. 2010;68:980-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 303. | Simon BI, Zatcoff AL, Kong JJW, O’Connell SM. Clinical and Histological Comparison of Extraction Socket Healing Following the Use of Autologous Platelet-Rich Fibrin Matrix (PRFM) to Ridge Preservation Procedures Employing Demineralized Freeze Dried Bone Allograft Material and Membrane. Open Dent J. 2009;3:92–99. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 304. | Kfir E, Kfir V, Kaluski E. Immediate bone augmentation after infected tooth extraction using titanium membranes. J Oral Implantol. 2007;33:133-138. [PubMed] |
| 305. | Mohamed JB, Alam MN, Singh G, Chandrasekaran SN. Alveolar bone expansion for implant placement in compromised aesthetic zone - case series. J Clin Diagn Res. 2014;8:237-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 306. | Krasny M, Krasny K, Kamiński A, Zadurska M, Piekarczyk P, Fiedor P. Evaluation of safety and efficacy of radiation-sterilized bone allografts in reconstructive oral surgery. Cell Tissue Bank. 2013;14:367-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 307. | Triveni MG, TarunKumar AB, Vinita Jain, Dhoom S Meh. Alveolar Ridge Preservation with β-TCP Graft and Platelet-Rich Fibrin. Int J of Oral Implant and Clin Res. 2012;3:96-100. |
| 308. | Krasny K, Kamiński A, Krasny M, Zadurska M, Piekarczyk P, Fiedor P. Clinical use of allogeneic bone granulates to reconstruct maxillary and mandibular alveolar processes. Transplant Proc. 2011;43:3142-3144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 309. | Peck MT, Marnewick J, Stephen L. Alveolar ridge preservation using leukocyte and platelet-rich fibrin: a report of a case. Case Rep Dent. 2011;2011:345048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 310. | Chen Y, Niu Z, Xue Y, Yuan F, Fu Y, Bai N. Improvement in the repair of defects in maxillofacial soft tissue in irradiated minipigs by a mixture of adipose-derived stem cells and platelet-rich fibrin. Br J Oral Maxillofac Surg. 2014;52:740-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 311. | Kulkarni MR, Thomas BS, Varghese JM, Bhat GS. Platelet-rich fibrin as an adjunct to palatal wound healing after harvesting a free gingival graft: A case series. J Indian Soc Periodontol. 2014;18:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 312. | Toffler M. Guided bone regeneration (GBR) using cortical bone pins in combination with leukocyte- and platelet-rich fibrin (L-PRF). Compend Contin Educ Dent. 2014;35:192-198. [PubMed] |
| 313. | Liu B, Tan XY, Liu YP, Xu XF, Li L, Xu HY, An R, Chen FM. The adjuvant use of stromal vascular fraction and platelet-rich fibrin for autologous adipose tissue transplantation. Tissue Eng Part C Methods. 2013;19:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 314. | Marrelli M, Tatullo M. Influence of PRF in the healing of bone and gingival tissues. Clinical and histological evaluations. Eur Rev Med Pharmacol Sci. 2013;17:1958-1962. [PubMed] |
| 315. | Jain V, Triveni MG, Kumar AB, Mehta DS. Role of platelet-rich-fibrin in enhancing palatal wound healing after free graft. Contemp Clin Dent. 2012;3:S240-S243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 316. | Chang YC, Zhao JH. Effects of platelet-rich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aust Dent J. 2011;56:365-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 317. | Tsai CH, Shen SY, Zhao JH, Chang YC. Platelet-rich fibrin modulates cell proliferation of human periodontally related cells in vitro. J Dent Sci. 2009;4:130-135. [RCA] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 318. | Soffer E, Ouhayoun JP, Anagnostou F. Fibrin sealants and platelet preparations in bone and periodontal healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:521-528. [PubMed] |
| 319. | Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Landes C, Sader R, Kirkpatrick C, Choukroun J. Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol. 2014;40:679-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 373] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 320. | Fan WJ, Yang M, Zhang C, Xue R, Zhang W, Qin HX. [Effects of Choukroun’s platelet-rich fibrin on human gingival fibroblasts proliferation, migration and type I collagen secretion]. Zhonghua Kouqiang Yixue Zazhi. 2013;48:72-76. [PubMed] |
| 321. | Yang KC, Wang CH, Chang HH, Chan WP, Chi CH, Kuo TF. Fibrin glue mixed with platelet-rich fibrin as a scaffold seeded with dental bud cells for tooth regeneration. J Tissue Eng Regen Med. 2012;6:777-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 322. | Huang FM, Yang SF, Zhao JH, Chang YC. Platelet-rich fibrin increases proliferation and differentiation of human dental pulp cells. J Endod. 2010;36:1628-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 323. | Dohan Ehrenfest DM, Diss A, Odin G, Doglioli P, Hippolyte MP, Charrier JB. In vitro effects of Choukroun’s PRF (platelet-rich fibrin) on human gingival fibroblasts, dermal prekeratinocytes, preadipocytes, and maxillofacial osteoblasts in primary cultures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:341-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 324. | Maney P, Amornporncharoen M, Palaiologou A. Applications of plasma rich in growth factors (PRGF) in dental surgery: a review. J West Soc Periodontol Periodontal Abstr. 2013;61:99-104. [PubMed] |
| 325. | Anitua E, Orive G, Pla R, Roman P, Serrano V, Andía I. The effects of PRGF on bone regeneration and on titanium implant osseointegration in goats: a histologic and histomorphometric study. J Biomed Mater Res A. 2009;91:158-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 326. | Singh S, Singh A, Singh S, Singh R. Application of PRF in surgical management of periapical lesions. Natl J Maxillofac Surg. 2013;4:94-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 327. | Del Fabbro M, Boggian C, Taschieri S. Immediate implant placement into fresh extraction sites with chronic periapical pathologic features combined with plasma rich in growth factors: preliminary results of single-cohort study. J Oral Maxillofac Surg. 2009;67:2476-2484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 328. | Anitua E, Prado R, Orive G. Bilateral sinus elevation evaluating plasma rich in growth factors technology: a report of five cases. Clin Implant Dent Relat Res. 2012;14:51-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 329. | Anitua E, Prado R, Orive G. A lateral approach for sinus elevation using PRGF technology. Clin Implant Dent Relat Res. 2009;11 Suppl 1:e23-e31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 330. | Birang R, Torabi A, Shahabooei M, Rismanchian M. Effect of plasma-rich in platelet-derived growth factors on peri-implant bone healing: An experimental study in canines. Dent Res J (Isfahan). 2012;9:93-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 331. | Birang R, Tavakoli M, Shahabouei M, Torabi A, Dargahi A, Soolari A. Investigation of peri-implant bone healing using autologous plasma rich in growth factors in the canine mandible after 12 weeks: a pilot study. Open Dent J. 2011;5:168-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 332. | Lafzi A, Faramarzi M, Shirmohammadi A, Behrozian A, Kashefimehr A, Khashabi E. Subepithelial connective tissue graft with and without the use of plasma rich in growth factors for treating root exposure. J Periodontal Implant Sci. 2012;42:196-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 333. | Lafzi A, Chitsazi MT, Farahani RM, Faramarzi M. Comparative clinical study of coronally advanced flap with and without use of plasma rich in growth factors in the treatment of gingival recession. Am J Dent. 2011;24:143-147. [PubMed] |
| 334. | Lafzi A, Shirmohammadi A, Faramarzi M, Jabali S, Shayan A. Clinical Comparison of Autogenous Bone Graft with and without Plasma Rich in Growth Factors in the Treatment of Grade II Furcation Involvement of Mandibular Molars. J Dent Res Dent Clin Dent Prospects. 2013;7:22-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 335. | Mansouri SS, Ghasemi M, Darmian SS, Pourseyediyan T. Treatment of Mandibular Molar Class II Furcation Defects in Humans With Bovine Porous Bone Mineral in Combination With Plasma Rich in Growth Factors. J Dent (Tehran). 2012;9:41-49. [PubMed] |
| 336. | Fuerst G, Gruber R, Tangl S, Sanroman F, Watzek G. Enhanced bone-to-implant contact by platelet-released growth factors in mandibular cortical bone: a histomorphometric study in minipigs. Int J Oral Maxillofac Implants. 2003;18:685-690. [PubMed] |
| 337. | Bakhtiar H, Vatanpour M, Rayani A, Navi F, Asna-Ashari E, Ahmadi A, Jafarzadeh H. The plasma-rich in growth factor as a suitable matrix in regenerative endodontics: a case series. N Y State Dent J. 2014;80:49-53. [PubMed] |
| 338. | Anitua E, Murias-Freijo A, Alkhraisat MH, Orive G. Clinical, radiographical, and histological outcomes of plasma rich in growth factors in extraction socket: a randomized controlled clinical trial. Clin Oral Investig. 2015;19:589-600. [PubMed] |
| 339. | Mogharehabed A, Birang R, Torabinia N, Nasiri S, Behfarnia P. Socket preservation using demineralized freezed dried bone allograft with and without plasma rich in growth factor: A canine study. Dent Res J (Isfahan). 2014;11:460-468. [PubMed] |
| 340. | Farina R, Bressan E, Taut A, Cucchi A, Trombelli L. Plasma rich in growth factors in human extraction sockets: a radiographic and histomorphometric study on early bone deposition. Clin Oral Implants Res. 2013;24:1360-1368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 341. | Haraji A, Lassemi E, Motamedi MH, Alavi M, Adibnejad S. Effect of plasma rich in growth factors on alveolar osteitis. Natl J Maxillofac Surg. 2012;3:38-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 342. | Anitua E, Begoña L, Orive G. Clinical evaluation of split-crest technique with ultrasonic bone surgery for narrow ridge expansion: status of soft and hard tissues and implant success. Clin Implant Dent Relat Res. 2013;15:176-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 343. | Anitua E, Tejero R, Zalduendo MM, Orive G. Plasma rich in growth factors promotes bone tissue regeneration by stimulating proliferation, migration, and autocrine secretion in primary human osteoblasts. J Periodontol. 2013;84:1180-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 344. | Anitua E, Sanchez M, Merayo-Lloves J, De la Fuente M, Muruzabal F, Orive G. Plasma rich in growth factors (PRGF-Endoret) stimulates proliferation and migration of primary keratocytes and conjunctival fibroblasts and inhibits and reverts TGF-beta1-Induced myodifferentiation. Invest Ophthalmol Vis Sci. 2011;52:6066-6073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 345. | Kim JM, Sohn DS, Bae MS, Moon JW, Lee JH, Park IS. Flapless transcrestal sinus augmentation using hydrodynamic piezoelectric internal sinus elevation with autologous concentrated growth factors alone. Implant Dent. 2014;23:168-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 346. | Del Fabbro M, Bortolin M, Taschieri S, Weinstein RL. Effect of autologous growth factors in maxillary sinus augmentation: a systematic review. Clin Implant Dent Relat Res. 2013;15:205-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 347. | Sohn DS, Heo JU, Kwak DH, Kim DE, Kim JM, Moon JW, Lee JH, Park IS. Bone regeneration in the maxillary sinus using an autologous fibrin-rich block with concentrated growth factors alone. Implant Dent. 2011;20:389-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 348. | Yu B, Wang Z. Effect of concentrated growth factors on beagle periodontal ligament stem cells in vitro. Mol Med Rep. 2014;9:235-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 349. | Peter M, Paul K. Use of Concentrated Growth Factor (CGF) in implantology Australasian Dental Practice, 2010. Available from: http://connection.ebscohost.com/c/articles/51907135/use-concentrated-growth-factor-cgf-implantology. |
| 350. | Kim TH, Kim SH, Sándor GK, Kim YD. Comparison of platelet-rich plasma (PRP), platelet-rich fibrin (PRF), and concentrated growth factor (CGF) in rabbit-skull defect healing. Arch Oral Biol. 2014;59:550-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 351. | Gheno E, Palermo A, Buffoli B, Rodella LF. The effectiveness of the use of xenogeneic bone blocks mixed with autologous Concentrated Growth Factors (CGF) in bone regeneration techniques: a case series. J Osseointegr. 2014;6:37-42. |
| 352. | Longo F, Guida A, Aversa C, Pavone E, Di Costanzo G, Ramaglia L, Ionna F. Platelet rich plasma in the treatment of bisphosphonate-related osteonecrosis of the jaw: personal experience and review of the literature. Int J Dent. 2014;2014:298945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |