Published online Nov 29, 2022. doi: 10.5317/wjog.v11.i4.40
Peer-review started: July 18, 2022
First decision: August 1, 2022
Revised: August 5, 2022
Accepted: November 23, 2022
Article in press: November 23, 2022
Published online: November 29, 2022
Processing time: 132 Days and 17.7 Hours
Epithelioid hemangioendothelioma (EHE) is an extremely rare tumor with a prevalence of one in a million and a very heterogenous spectrum of disease that varies from an indolent to a metastasizing aggressive disease, with the liver, lung and bone being the primarily involved organs. Peritoneal forms of EHE are even rare, and only 12 cases have been reported to date in the literature.
A 66-year-old female came to our attention complaining low abdominal and perineal pain. Magnetic resonance imaging examination showed a 52 mm × 58 mm × 32 mm cystic mass with some smooth septa, simulating an ovarian cyst. Explorative laparoscopy demonstrated the presence of a peritoneal mass of augmented consistency connected with a sigmoid epiploic appendix in the right side of the Pouch of Douglas, that was surgically removed. Histological exa-mination revealed a primitive peritoneafl hemangioendothelioma. The patient easily recovered from surgery with no residual pain or discomfort. She is regularly attending a 3-years follow-up that is negative for local recurrence of disease or distant metastases.
Peritoneal form of EHE often simulates masses of other nature, as in our case. Given its unspecific clinical and radiological presentation, patients are often forced to a large series of tests and examinations before reaching a definitive diagnosis, that can only histologically made. The possibility of EHE should always be considered in case of unexplained chronic abdominal pain associated to a non-specific mass.
Core Tip: In this article we describe the case of a woman of middle age who came to our observation for chronic abdominal pain. Diagnostic examinations showed a mass of undefined nature which simulated an ovarian cyst due to its pelvic position and its morphological features. Histological examination revealed a primary peritoneal hemangioendothelioma, which is an extremely rare form of epithelioid hemangioendothelioma, with only 12 cases reported in the literature to date. Epithelioid hemangioendothelioma has a very heterogenous spectrum of disease that varies from an indolent to a metastasizing aggressive disease, with the liver, lung and bone being the primarily involved organs.
- Citation: Spinelli C, Ghionzoli M, Strambi S. Primary peritoneal hemangioendothelioma simulating an ovarian cyst: A case report and review of literature. World J Obstet Gynecol 2022; 11(4): 40-46
- URL: https://www.wjgnet.com/2218-6220/full/v11/i4/40.htm
- DOI: https://dx.doi.org/10.5317/wjog.v11.i4.40
Epithelioid hemangioendothelioma (EHE) is an extremely rare neoplasm with a prevalence of 1:1000000[1], and as such, the current reported cases are limited to single reports and series aimed to better describe the clinical, pathologic, and molecular characteristics, as well as the best treatment approaches[2].
The spectrum of disease is very heterogenous and varies greatly between an indolent disease and a metastasizing aggressive disease, with the liver, lung and bone being the primarily involved organs[2]. However, EHE can occur in various anatomical sites such as retroperitoneum, ovary, pleura, lymph nodes and subcutaneous fat[1], making the clinical presentation very unspecific and the diagnosis often challenging. Given its heterogeneity, also the prognosis differs from one patient to another. Traditionally, risk factors for worse outcomes have comprised anemia and weight loss, as well as pulmonary symptoms such as pleurisy[3,4]. An increased mitotic activity and size have also been seen to be correlated with a worse prognosis[5]. Peritoneal forms of EHE are seldom described: To date only 12 other cases have been reported (Table 1)[6-12].
| Ref. | Journal | Number of cases | Average age | Sex | Treatment |
| Kalisher et al[6], 1968 | Cancer | 1 | 30 | F | Surgery |
| Shih et al[7], 1995 | J Pediatr Surg | 1 | 13 | F | Surgery |
| Lin et al[8], 1996 | Am J Surg Pathol | 3 | 52 | 2 F; 1 M | Surgery |
| Attanoos et al[9], 1997 | Histopathology | 1 | 51 | M | Surgery |
| Ratan et al[10], 1999 | Surg Today | 1 | 11 | F | Surgery |
| Melzack et al[11], 2004 | Virchows Arch | 2 | 28.5 | 2 M | Surgery |
| Posligua et al[12], 2006 | Int J Surg Pathol | 3 | 45.6 | 2 M; 1 F | Surgery |
| Total | 12 | 19.2 | 6 F; 6 M |
In this article we describe the case of a woman of middle age who came to our observation for abdominal pain, which was then discovered to be caused by a primary peritoneal hemangioendothelioma simulating an ovarian cyst.
A 66-year-old female with history of right mammalian quadrantectomy followed by radiotherapy for breast cancer came to our attention complaining low abdominal and perineal pain.
A recent routinely gynecological examination showed the presence at ultrasound of a small fluid collection in the Douglas pouch, with normal genital organs.
There is no history of past illness.
There is no personal and family history.
The physical examination and the laboratory blood tests including tumor markers levels (CEA, Ca 19.9, Ca 125, aFP) were all normal.
Does not involve laboratory examination.
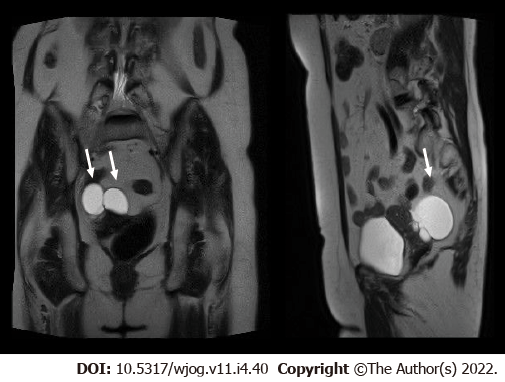
Colonoscopy was completely negative while abdominal contrast-enhancement computed tomography (CT) examination confirmed the presence of a 76 mm × 52 mm fluid collection with some incomplete septa located in the right paramedian region of the Douglas pouch with mild delayed enhancement. The patient was then submitted to an abdominal magnetic resonance imaging which detected the presence of a 52 mm × 58 mm × 32 mm cystic mass with some smooth septa, simulating an ovarian cyst (Figure 1).
Considering the impossibility to discriminate the nature of the mass, we decided to perform a diagnostic abdominal explorative laparoscopy.
During surgery, a peritoneal mass of augmented consistency strictly connected with a sigmoid epiploic appendix was found in the right side of the Pouch of Douglas and surgically removed. Extemporaneous histological examination revealed the presence of a focal central area of necrosis and blood vessels of various dimension, intense chronic inflammation consisting of lympho-monocytoid cells, plasma-cells and hystiocytes filled with hemosiderin, without atypic cells. No further surgical resection was therefore performed. Post-operative course was deemed uneventful, and the patient was discharged on 3rd post-operative day.
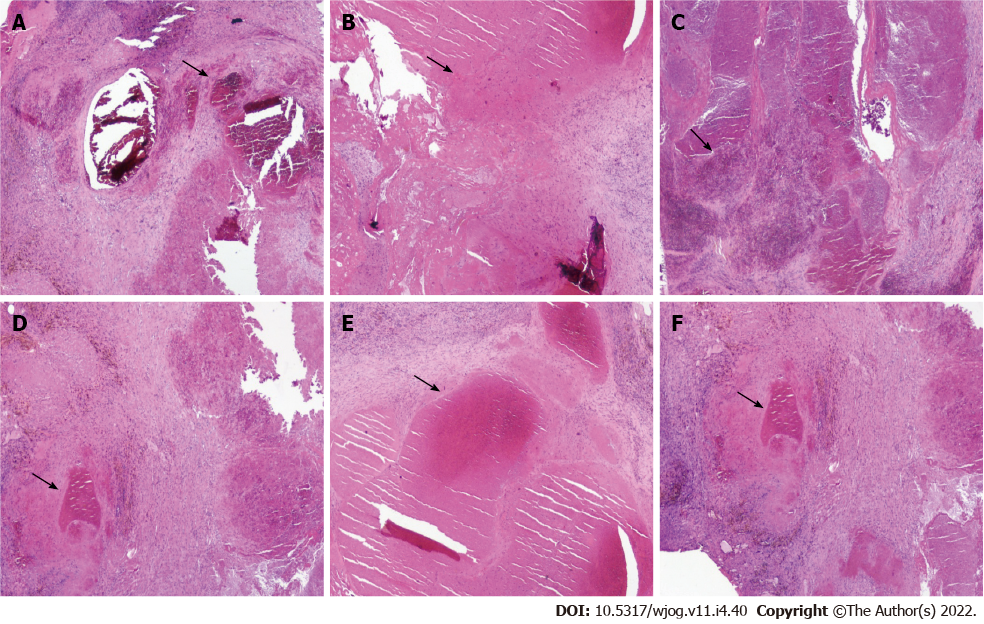
Definitive histological and immunohistochemistry examination demonstrated a primitive peritoneal hemangioendothelioma which consisted of a vascularized proliferation of blood vessels associated with involutive aspects and necrosis (Figure 2). A regular 3-years scheduled ultrasound and abdominal CT scan follow-up has shown neither local recurrence of the disease nor distant metastases. Currently, the patient is in good clinical condition without any residual pain or discomfort. Written informed consent was obtained from the patient for the anonymous publication of the case.
EHE is defined as a localized intrusive vascular tumor which originates from endothelial cells. It may originate from any anatomical site and can metastasize to soft tissues, bones and viscera[13]. The first description of EHE comes from Dail and Liebow in 1975: They defined it as an intravascular bronchoalveolar tumor involving the lungs[14]. The term “epithelioid hemangioendothelioma” was then coined by Weiss and Enzinger in 1982[15], to highlight a neoplasm made of “rounded or slightly spindled eosinophilic endothelial cells that grows in small nests or cords”. Nowadays, the World Health Organization (WHO) and the International Society for the Study of Vascular Anomalies (ISSVA) classify EHE as a localized, intrusive and potentially metastasizing vascular tumor[16,17].
Mean age at presentation is 43 years, with the female sex having a slightly higher preponderance than the male sex (1.6 female patients to 1 male patient)[1,13]. In the pediatric population, only 24 cases have been described, with a mean age of 12 years[18]. Liver (21%), bone (14%), and lung (12%) are the most frequent sites of involvement of EHE, but this neoplasm can affect many other sites throughout the body, such as the neck region, the abdominal organs, the genitourinary tract, and also lymph nodes and breast[13].
Exact causes of EHE are still unknown. Tanas et al[19] identified WWTR1 (3q25) and CAMTA1 (1p36) as a couple of genes involved in the t(1;3)(p36;q25) chromosomal translocation that is seen in almost every EHE. However, Antonescu et al[20] depicted a different group of EHE, which is seen more frequently in younger patients and without sex predilection, that shows a YAP1-TFE3 gene fusion. In addition, another study[21] has proposed the role of chronic Bartonella infection in the pathogenesis of EHE: in fact, the intraerythrocytic and intraendothelial infections, that this microorganism induces, could be linked to the rise of vascular tumors like EHE.
As to the peritoneal form of EHE, the main symptoms are abdominal pain and enlargement, with or without ascites, sometimes associated to nausea, vomiting and weight loss. Our patient reported an intermitting chronic abdominal pain, localized in the lower abdominal quadrants. The recurrent nature of this pain can be explained by the fact that the mass, simulating an ovarian cyst, underwent periodical episodes of blooding, also causing fluid collects. Shiba et al[22], in a multicenter retrospective study on 42 Japanese patients, interestingly reported that the presence of symptoms at diagnosis, along with a tumor size greater than 3 cm, were significantly correlated with poor outcomes.
Imaging diagnostic in case of peritoneal EHE usually points out an unclear soft-tissue mass displaying reduced enhancement[23]. It can be associated with signs of invasion of the neighboring structures[13]. Comparison with previous imaging may demonstrate the slow growth rate commonly seen with EHE and less likely to be caused by any other tumor[1]. An omental mass, potentially presenting with tiny implants or wider nodules, is the most typical finding at surgery[12]. In our case, the surgical exploration showed the presence of a peritoneal mass, of augmented consistency, located in the Douglas pouch. Peritoneal carcinomatosis and malignant mesothelioma can easily simulate the aspect of EHE, and because of its rare prevalence, this can lead surgeons to not primarily consider EHE in the differential diagnosis. On the frozen section, the amount of the characteristic round cells with prominent cytoplasmic vacuoles containing erythrocytes is not always significant, but the myxohyaline feature in the stroma can be helpful; the presence of eosinophils is suggestive of EHE, as well[24,25]. Despite the widely infiltrative nature of peritoneal EHE, the single tumor cells generally show only minimal atypia, and the mitotic activity is generally low[12]. Some studies showed that histologic findings of spindle tumor cells and enhanced mitosis (above three mitotic figures per 50 HPF) are associated with worse outcome[1,5,26,27]. The mass of our patient also consisted of a central area of necrosis, vessels of various dimension, intense chronic inflammation with lympho-monocytoid cells, plasma-cells, hystiocytes filled with hemosiderin; no atypic cells were found. Posligua et al[12] also suggest the use of electron microscopy in the diagnosis of EHE, because it allows to demonstrate the presence of Weibel-Palade bodies, that have been seen to be more specific for peritoneal EHE, compared to other visceral and soft tissues forms[28].
Immunohistochemistry is an essential part of the diagnostic algorithm, that allows to differentiate primary peritoneal EHE from morphologic pretenders, including carcinoma, mesothelioma of the epithelioid or deciduoid types, peritoneal deciduosis, epithelioid leiomyosarcoma, and malignant gastrointestinal stromal tumor with epithelioid features. In this regard, studies demonstrate that the vascular markers of factor VIII-antigen, CD31, CD34 and thrombomodulin, are very helpful to differentiate EHE from the other tumor types[12].
Because of the variable presentation, course, and outcome of EHE, there is not a standard treatment plan, and the type of therapy must be tailored for every patient[13]. For asymptomatic patients or those with comorbidities precluding treatment, an initial period of observation with repeated clinical and imaging evaluation is recommended to assess the possible progression of the disease[29]. To date, surgical resection represents the most practiced therapeutic option[30] even if few studies[29,31] have shown a reduced response of EHE tumors to the association of conventional chemotherapy and antiangiogenic therapy, which targets vascular endothelial growth factor receptors that are expressed in EHE. In this regard, molecules such as carboplatin, paclitaxel and bevacizumab have been used. Other studies have demonstrated clinical benefits obtained among patients (56%) treated with sirolimus as a single agent[32]. Immune inhibitors are being tested for the treatment of sarcomas and could potentially have a role in the future treatment plan of EHE[33,34] Therapeutic strategies may be developed aiming to WWTR1-CAMTA1 or YAP1-TFE3 mutations, which are common in EHE[19,20].
EHE is a rare form of sarcoma that can present in any part of the body, and the peritoneal form of EHE often simulates masses of other nature, as in our case. Given its unspecific clinical and radiological presentation, patients are often forced to a large series of tests end examinations before reaching a definitive diagnosis, that can be made only histologically. The possibility of EHE should always be considered in case of slowly growing tumors that invade adjacent organs in the classic sites, as well as in case of unexplained chronic abdominal pain associated to a non-specific neoformation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Paparoupa M, Germany; Tong Y, China S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Sardaro A, Bardoscia L, Petruzzelli MF, Portaluri M. Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev. 2014;8:259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 138] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 2. | Rosenberg A, Agulnik M. Epithelioid Hemangioendothelioma: Update on Diagnosis and Treatment. Curr Treat Options Oncol. 2018;19:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 3. | Amin RM, Hiroshima K, Kokubo T, Nishikawa M, Narita M, Kuroki M, Nakatani Y. Risk factors and independent predictors of survival in patients with pulmonary epithelioid haemangioendothelioma. Review of the literature and a case report. Respirology. 2006;11:818-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Rosengarten D, Kramer MR, Amir G, Fuks L, Berkman N. Pulmonary epithelioid hemangioendothelioma. Isr Med Assoc J. 2011;13:676-679. [PubMed] |
| 5. | Deyrup AT, Tighiouart M, Montag AG, Weiss SW. Epithelioid hemangioendothelioma of soft tissue: a proposal for risk stratification based on 49 cases. Am J Surg Pathol. 2008;32:924-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 199] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 6. | Kalisher L, Straatsma GW, Rosenberg BF, Vaitkevicius VK. Primary malignant hemangio- endothelioma of the greater omentum. A case report. Cancer. 1968;22:1126-1130. [PubMed] [DOI] [Full Text] |
| 7. | Shih SL, Sheu JC, Chen BF, Ma YC. Malignant hemangioendothelioma presenting as omental masses in a child. J Pediatr Surg. 1995;30:118-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Lin BT, Colby T, Gown AM, Hammar SP, Mertens RB, Churg A, Battifora H. Malignant vascular tumors of the serous membranes mimicking mesothelioma. A report of 14 cases. Am J Surg Pathol. 1996;20:1431-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 99] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Attanoos RL, Dallimore NS, Gibbs AR. Primary epithelioid haemangioendothelioma of the peritoneum: an unusual mimic of diffuse malignant mesothelioma. Histopathology. 1997;30:375-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Ratan S, Bhatnagar V, Gupta SD, Mitra DK. Epithelioid hemangioendothelioma of the greater omentum: report of a case. Surg Today. 1999;29:919-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Melzack R. Phantom limbs. Sci Am. 1992;266:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 12. | Posligua L, Anatelli F, Dehner LP, Pfeifer JD. Primary peritoneal epithelioid hemangioendothelioma. Int J Surg Pathol. 2006;14:257-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Jang JK, Thomas R, Braschi-Amirfarzan M, Jagannathan JP. A Review of the Spectrum of Imaging Manifestations of Epithelioid Hemangioendothelioma. AJR Am J Roentgenol. 2020;215:1290-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Dail D, Liebow AA. Intravascular bronchioloalveolar tumor. Am J Pathol. 1975;78:6a-7a. |
| 15. | Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 16. | Merrow AC, Gupta A, Patel MN, Adams DM. 2014 Revised Classification of Vascular Lesions from the International Society for the Study of Vascular Anomalies: Radiologic-Pathologic Update. Radiographics. 2016;36:1494-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 17. | Sepulveda A, Buchanan EP. Vascular tumors. Semin Plast Surg. 2014;28:49-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Cousin S, Le Loarer F, Crombé A, Karanian M, Minard-Colin V, Penel N. [Epithelioid hemangioendothelioma]. Bull Cancer. 2019;106:73-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Tanas MR, Sboner A, Oliveira AM, Erickson-Johnson MR, Hespelt J, Hanwright PJ, Flanagan J, Luo Y, Fenwick K, Natrajan R, Mitsopoulos C, Zvelebil M, Hoch BL, Weiss SW, Debiec-Rychter M, Sciot R, West RB, Lazar AJ, Ashworth A, Reis-Filho JS, Lord CJ, Gerstein MB, Rubin MA, Rubin BP. Identification of a disease-defining gene fusion in epithelioid hemangioendothelioma. Sci Transl Med. 2011;3:98ra82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 287] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 20. | Antonescu CR, Le Loarer F, Mosquera JM, Sboner A, Zhang L, Chen CL, Chen HW, Pathan N, Krausz T, Dickson BC, Weinreb I, Rubin MA, Hameed M, Fletcher CD. Novel YAP1-TFE3 fusion defines a distinct subset of epithelioid hemangioendothelioma. Genes Chromosomes Cancer. 2013;52:775-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 412] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 21. | Mascarelli PE, Iredell JR, Maggi RG, Weinberg G, Breitschwerdt EB. Bartonella species bacteremia in two patients with epithelioid hemangioendothelioma. J Clin Microbiol. 2011;49:4006-4012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Shiba S, Imaoka H, Shioji K, Suzuki E, Horiguchi S, Terashima T, Kojima Y, Okuno T, Sukawa Y, Tsuji K, Umemoto K, Asagi A, Todaka A, Ueno M, Ikeda M, Morizane C, Furuse J. Clinical characteristics of Japanese patients with epithelioid hemangioendothelioma: a multicenter retrospective study. BMC Cancer. 2018;18:993. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 23. | Epelboym Y, Engelkemier DR, Thomas-Chausse F, Alomari AI, Al-Ibraheemi A, Trenor CC 3rd, Adams DM, Chaudry G. Imaging findings in epithelioid hemangioendothelioma. Clin Imaging. 2019;58:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Hamlat A, Casallo-Quilliano C, Saikali S, Lesimple T, Brassier G. Epithelioid hemangioendothelioma of the infundibular-hypothalamic region: case report and literature review. J Neurooncol. 2004;67:361-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Pinet C, Magnan A, Garbe L, Payan MJ, Vervloet D. Aggressive form of pleural epithelioid haemangioendothelioma: complete response after chemotherapy. Eur Respir J. 1999;14:237-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Kitaichi M, Nagai S, Nishimura K, Itoh H, Asamoto H, Izumi T, Dail DH. Pulmonary epithelioid haemangioendothelioma in 21 patients, including three with partial spontaneous regression. Eur Respir J. 1998;12:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 139] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 27. | Schmoldt A, Benthe HF, Haberland G. Digitoxin metabolism by rat liver microsomes. Biochem Pharmacol. 1975;24:1639-1641. [RCA] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 84] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Tsuneyoshi M, Dorfman HD, Bauer TW. Epithelioid hemangioendothelioma of bone. A clinicopathologic, ultrastructural, and immunohistochemical study. Am J Surg Pathol. 1986;10:754-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 120] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 29. | Yousaf N, Maruzzo M, Judson I, Al-Muderis O, Fisher C, Benson C. Systemic treatment options for epithelioid haemangioendothelioma: the Royal Marsden Hospital experience. Anticancer Res. 2015;35:473-480. [PubMed] |
| 30. | Wu X, Li B, Zheng C, Hong T, He X. Clinical characteristics of epithelioid hemangioendothelioma: a single-center retrospective study. Eur J Med Res. 2019;24:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 31. | Belmont L, Zemoura L, Couderc LJ. Pulmonary epithelioid haemangioendothelioma and bevacizumab. J Thorac Oncol. 2008;3:557-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Stacchiotti S, Provenzano S, Dagrada G, Negri T, Brich S, Basso U, Brunello A, Grosso F, Galli L, Palassini E, Libertini M, Colia V, Gronchi A, Dei Tos AP, Crippa F, Morosi C, Pilotti S, Casali PG. Sirolimus in Advanced Epithelioid Hemangioendothelioma: A Retrospective Case-Series Analysis from the Italian Rare Cancer Network Database. Ann Surg Oncol. 2016;23:2735-2744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 33. | Veenstra R, Kostine M, Cleton-Jansen AM, de Miranda NF, Bovée JV. Immune checkpoint inhibitors in sarcomas: in quest of predictive biomarkers. Lab Invest. 2018;98:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Thomas R, Somarouthu B, Alessandrino F, Kurra V, Shinagare AB. Atypical Response Patterns in Patients Treated With Nivolumab. AJR Am J Roentgenol. 2019;1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (1)] |