Revised: August 22, 2013
Accepted: August 28, 2013
Published online: September 28, 2013
Processing time: 189 Days and 16 Hours
Malignant peripheral nerve sheath tumor (MPNST) is an uncommon sarcoma which arises from pluripotent stem cells of the neural crest and differentiates predominantly towards Schwann cells. Low grade spinal MPNST with skeletal muscle differentiation (malignant triton tumor) is vanishingly rare. In this study, we report a case of a 53-year-old female with a homogenously enhancing C2-C4 extradural lesion. The lesion demonstrated a biphasic histologic pattern with a diffusely infiltrating, atypical spindle cell component strongly positive for vimentin and focally positive for S-100. The second component consisted of diffusely scattered clusters of mature skeletal muscle cells which were positive for desmin, fast myosin and muscle specific actin but negative for Myogenin and MyoD-1. The Ki-67 labeling index was low (< 1%) and no necrosis was identified. The present case is remarkable because of its rare location, low grade histology and unusual immunophenotype of the skeletal muscle component, which were not previously described.
Core tip: Malignant peripheral nerve sheath tumor (MPNST) is an uncommon sarcoma with dismal prognosis. Low grade MPNST with skeletal muscle differentiation (malignant triton tumor) in cervical spine is vanishingly rare. The present case is remarkable because of its rare location, low grade histological features and unusual immunophenotype of the mature skeletal muscle component, which were not previously described. Thus, our study expands the morphological spectrum and the clinicopathological significance of this uncommon tumor. These novel findings should be interesting to the neuropathologists, neurologists and neurosurgeons.
- Citation: Zhang M, Weaver M, Khurana JS, Mukherjee AL. Low grade spinal malignant triton tumor with mature skeletal muscle differentiation. World J Neurol 2013; 3(3): 75-78
- URL: https://www.wjgnet.com/2218-6212/full/v3/i3/75.htm
- DOI: https://dx.doi.org/10.5316/wjn.v3.i3.75
Malignant peripheral nerve sheath tumor (MPNST) is an uncommon soft tissue sarcoma which arises from pluripotent stem cells of the neural crest and differentiates towards Schwann cells[1]. Spinal MPNSTs are rare and have dismal prognosis[2]. MPSNT with coexistence of rhabdomyosarcomatous elements are termed malignant triton tumor (MTT)[3] and have been rarely reported in the spinal cord[4]. Typically, they are high grade with worse prognosis compared to conventional MPNST[5,6]. Low grade spinal MTT is vanishingly rare with a single case reported in literature[2]. A low grade spinal MTT with cytologically benign and immunophenotypically mature skeletal muscle component has not been previously described.
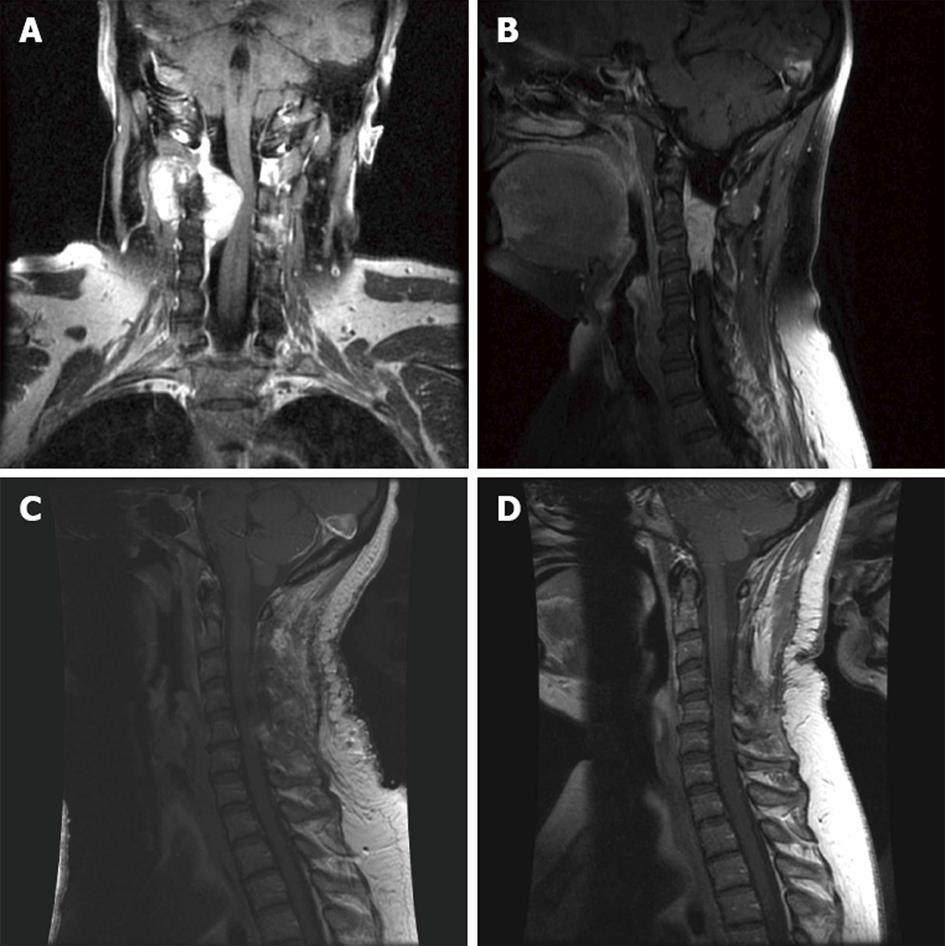
A 53-year-old female without family history or stigmata of neurofibromatosis presented with worsening neck pain and right sided neck stiffness. The pain is present in the left side (buzzing in left hip and left heel). The quality of the pain is described as aching and shooting (pulling, popping) and the severity of the pain is at 6/10. The symptoms are aggravated by position and twisting. The pain is worse during the night while the stiffness is present all day. Physical examination is unremarkable except for right facial nerve weakness nerve. MRI showed a homogenously enhancing C2-C4 intraspinal extradural lesion exiting out the foramen at C2-C3 in a dumbbell fashion (Figure 1A and B). A C2-C4 laminectomy was performed by using a combination of Leksell rongerus, Kerrisons and curettes. A tannish shear mass was identified in the epidural space from C2 to the top of C4. The mass was debulked from the inside using the combination of pituitary rongeurs as well as cavitron ultrasonic surgical aspirator debulking and bipolar electrocautery. The post-operative MRI showed markedly decreased mass effect on the cervical cord (Figure 1C). Bone stimulator and cervical collar were placed after surgery. The patient is treated with Percocet for analgesia and managed by physical therapy. No adjuvant treatment no radiation treatment were started. She is currently under regular follow up every six month (Figure 1D, 10 mo post-operative MRI), without evidence of recurrence (23 mo post surgery).
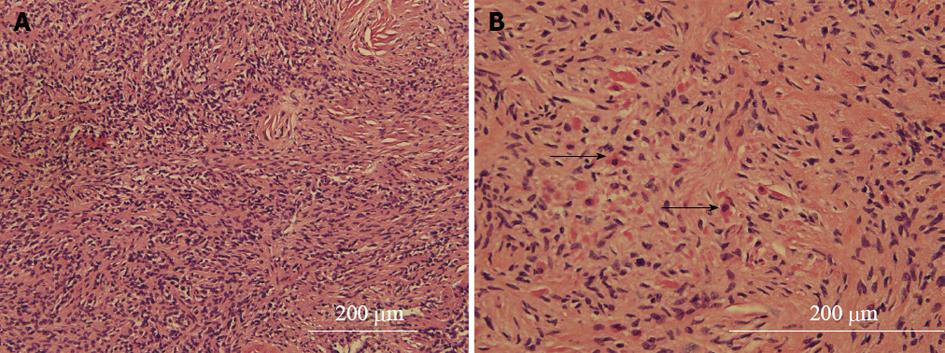
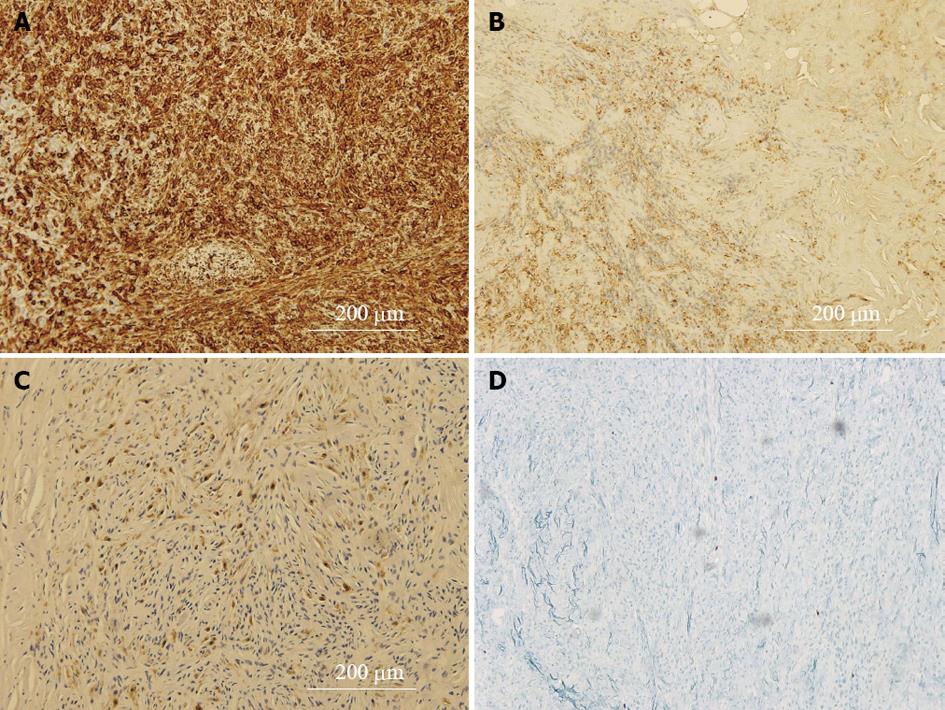
The tumor was received as tan soft tissue aggregates measuring 5.0 cm × 3.4 cm × 0.8 cm. Microscopic examination demonstrated a distinctly biphasic neoplasm with an infiltrating, moderately atypical amitotic spindle cell component (Figure 2A). This component had hypercellular areas that alternate with paucicellular highly collagenized areas containing small-spindled nuclei with a wavy appearance, suggestive of a low grade malignant peripheral nerve sheath tumor[7]. The second component consisted of diffusely scattered clusters of mature appearing amitotic small skeletal muscle cells (Figure 2B). The immunohistochemical studies showed the spindle cell component to be strongly positive for vimentin (Figure 3A) and focally positive for S-100 (Figure 3B), CD57. Rare cells were positive for CD34 and CD117. The neoplastic cells were negative for smooth muscle actin, estrogen receptor, EMA, AE1/AE3 and p53. The small round cells with skeletal muscle morphology showed a mature skeletal muscle phenotype with expression of desmin, fast myosin and muscle specific actin (Figure 3C). However, they were negative for rhabdomyoblastic markers Myogenin and MyoD-1. Neurofilament protein immunostain did not show any entrapped axons in the lesion. The Ki-67 labeling index was low (< 1%) (Figure 3D) and no necrosis was identified. The immunomorphological features were interpreted to be consistent with unusual low grade variant of MPNST with mature skeletal muscle differentiation. Neurofibroma and cellular schwannoma were also considered in the differential diagnosis. But hypercellularity, nuclear enlargement (three times the size of neurofibroma nucleus), infiltrative growth pattern, lack of neurofilament immunostaining and focal S-100 positivity favored the diagnosis of low grade MPNST. Of note, cellular schwannoma is typically strongly and diffusely positive for S-100 and neurofibromas shows entrapped neurofilament positive axons.
The present case is remarkable because of its location, low grade histology and unique phenotype of the skeletal muscle component. A literature review of the spinal MPNSTs revealed a total of 59 reported cases with only one case showing exclusive extradural location in cervical spine[2,8]. Exclusively extradural cervical spinal location of our case is unusual. Spinal MPNSTs, reported in the literature typically show high grade histology (necrosis, high mitotic rate and Ki-67 labeling index) and have worse prognosis compared to conventional MPNST[5,8,9]. Only a small number of MPNSTs are low grade (15%) and they can have diverse histopathology, location and growth patterns[7,9]. Smooth muscle differentiation has been reported in a case of low grade MPNST[10]. However, mature skeletal muscle component in a low grade MPNST has not been previously reported.
The skeletal muscle component was diffuse and seemed an integral part of the tumor. The diffuse nature of the skeletal muscle component excluded the possibility that this was entrapped muscle at the edge of the tumor. Malignant triton tumors typically have a rhabdomyosarcomatous component[3]. Benign triton tumor usually refers to neuromuscular hamartomas, where mature skeletal muscle replaces nerve fascicles[11]. In contrast to conventional MTT which are positive for rhabdomyoblastic markers Myogenin and MyoD-1, both markers are negative in our case. MyoD-1 and myogenin are members of the Myogenic transcriptional regulatory protein, are the most widely used markers to express the early in skeletal muscle differentiation. They are very sensitive and specific for the diagnosis of immature skeletal muscle in rhabdomyosarcoma. Mature skeletal muscle component in a diffusely infiltrating peripheral nerve sheath tumor with hypercellularity and nuclear atypia is very unusual. Low grade MTT has been reported in the oral cavity[12] and recently in lumber spine[2]. In both the cases, immunophenotypic maturity of the skeletal muscle component was not evaluated by MyoD-1 and Myogenin immunostain. In the only reported low grade spinal MTT, the patient is alive after 18 mo with no evidence of disease following total surgical removal and radiotherapy[2]. Although the clinical indication of such features is still undetermined, the mature skeletal muscle differentiation might indicate a better prognosis than the conventional MTT, evidenced by the prolonged disease free interval of our patient (23 month post surgery without chemotherapy and radiation therarpy).
In conclusion, here we have reported a case of low-grade MTT with unusual location and distinctive mature skeletal muscle differentiation, which expands the morphological spectrum of this rare tumor.
P- Reviewers Schmidt J, Siu PM S- Editor Wen LL L- Editor A E- Editor Yan JL
| 1. | Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97-109. [PubMed] |
| 2. | Prieto R, Pascual JM, García-Cabezas MA, López-Barea F, Barrios L, González-Llanos F. Low-grade malignant triton tumor in the lumbar spine: a rare variant of malignant peripheral nerve sheath tumor with rhabdomyoblastic differentiation. Neuropathology. 2012;32:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Stasik CJ, Tawfik O. Malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation (malignant triton tumor). Arch Pathol Lab Med. 2006;130:1878-1881. [PubMed] |
| 4. | Crandon IW, Char G, Reynolds C, Wellington P, Williams E. Malignant triton tumour of the spine: a case report. West Indian Med J. 1995;44:143-145. [PubMed] |
| 5. | Kourea HP, Bilsky MH, Leung DH, Lewis JJ, Woodruff JM. Subdiaphragmatic and intrathoracic paraspinal malignant peripheral nerve sheath tumors: a clinicopathologic study of 25 patients and 26 tumors. Cancer. 1998;82:2191-2203. [PubMed] |
| 6. | Victoria L, McCulloch TM, Callaghan EJ, Bauman NM. Malignant triton tumor of the head and neck: A case report and review of the literature. Head Neck. 1999;21:663-670. [PubMed] |
| 7. | Yamaguchi U, Hasegawa T, Hirose T, Chuman H, Kawai A, Ito Y, Beppu Y. Low grade malignant peripheral nerve sheath tumour: varied cytological and histological patterns. J Clin Pathol. 2003;56:826-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Ghosh A, Sastri SB, Srinivas D, Mahadevan A, Anandappa CB, Shankar SK. Malignant triton tumor of cervical spine with hemorrhage. J Clin Neurosci. 2011;18:721-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Isla A, Gutierrez M, Casillas M, Gil JL. Malignant triton tumor in the thoracic spine. Childs Nerv Syst. 2000;16:256-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Rodriguez FJ, Scheithauer BW, Abell-Aleff PC, Elamin E, Erlandson RA. Low grade malignant peripheral nerve sheath tumor with smooth muscle differentiation. Acta Neuropathol. 2007;113:705-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Awasthi D, Kline DG, Beckman EN. Neuromuscular hamartoma (benign “triton” tumor) of the brachial plexus. Case report. J Neurosurg. 1991;75:795-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | James JA, Bali NS, Sloan P, Shanks JH. Low-grade malignant Triton tumor of the oral cavity: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:699-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |