Peer-review started: November 13, 2016
First decision: March 7, 2017
Revised: March 15, 2017
Accepted: April 4, 2017
Article in press: April 7, 2017
Published online: May 6, 2017
Processing time: 147 Days and 15.5 Hours
Hemophilia A is an X-linked recessive disorder characterized by a deficiency of coagulation factor VIII (FVIII) and therefore by a greater risk of bleeding during percutaneous interventional procedures and during the dual antiplatelet therapy (DAPT) in patients with ischemic heart disease. Information regarding safe percutaneous procedures in hemophiliacs is limited. Since the introduction of FVVIII concentrates, the life expectancy of hemophiliac patients has improved and consequently, the rate of ischemic heart disease in this population is increased. Frequently the replacement therapy can trigger the onset of an acute coronary syndrome. We report a case of a patient with mild Hemophilia A, who presents with unstable angina, treated successfully with coronary angioplasty and drug eluting stent implantation without replacement of FVVIII, treated with long term DAPT without major bleeding after six months of follow up.
Core tip: Hemophilia is a rare condition, but in some cases, could create difficulties in the management of other disease, such as acute coronary syndrome and unstable angina. Data in literature regarding this condition are lacking. This case report would be an example of the management of patients with mild deficit of Factor VIII activity according to the recent consensus.
- Citation: Carbone A, Formisano T, Natale F, Cappelli Bigazzi M, Tartaglione D, Golia E, Gragnano F, Crisci M, Bianchi RM, Calabrò R, Russo MG, Calabrò P. Management of unstable angina in a patient with Haemophilia A. World J Hematol 2017; 6(2): 28-31
- URL: https://www.wjgnet.com/2218-6204/full/v6/i2/28.htm
- DOI: https://dx.doi.org/10.5315/wjh.v6.i2.28
Hemophilia A is an X-linked recessive disorder with frequency of approximately 1 in 8500 live births, characterized by a deficiency of coagulation factor VIII (FVIII) and therefore by a greater risk of bleeding. Hemophilia A is defined “mild” when the activity of FVIII is greater than 5% (> 0015 IU/mL) and presents episodes of bleeding after hematological stress (surgery, childbirth, trauma). It is a moderate disorder for levels of FVIII activity between 1% and 5% (0.01-0.05 IU/mL)[1]. The severe form, in which the activity of FVIII is < 1% (< 0.01 IU/mL), represents 50% of cases and is characterized by spontaneous bleeding in the joints and muscles and high risk of intracranial hemorrhage[1]. Since the introduction of FVIII concentrates in 1960 and the preventive treatment in 1970 the life expectancy of this patients, in developed countries, has improved. Consequently, the rate of ischemic heart disease in this population is increased. Kulkarni et al[2] assessed the prevalence of ischemic heart disease in 3422 American patients with hemophilia, analyzing discharge records from the hospital between 1993 and 1998. The prevalence of coronary heart disease was 0.05% in patients under 30 years of age and 15.2% in those aged 60 or more[2], similar to the general population[3]. Girolami et al[4,5] have shown that most of thrombotic cardiovascular events in hemophiliac patients occur during the infusion of recombinant FVIII or DDAVP.
The first line therapy of Acute Coronary Syndromes is the percutaneous transluminal coronary angioplasty (PTCA) and stent implantation. In hemophiliacs, invasive treatment is more dangerous because they have increased risk of bleeding during the procedure and with the use of anticoagulants and antiplatelet agents. The management of unstable angina in this population is suggested by a Consent Document of the World Federation of Hemophilia[6]. Experts recommend levels of FVIII activity of 80%, during the PTCA, and in 48 h, achieved through the infusion of recombinant FVIII.
We show a case of a patient with mild Hemophilia A who presents with unstable angina, not triggered by the infusion of clotting factor concentrate, treated successfully with coronary angioplasty and drug eluting stent (DES) implantation without replacement of FVIII.
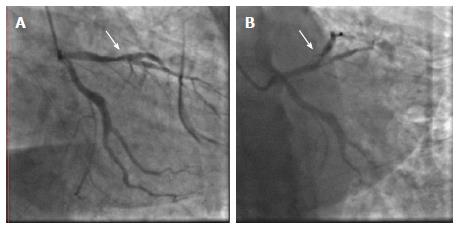
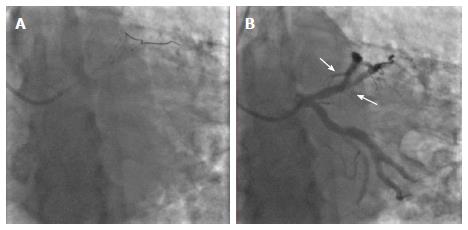
A 55 years old age man with mild deficit of FVIII activity (FVIII activity of 50%), HCV-related liver disease, tobacco use, hypertension, dyslipidemia, family history of cardiovascular disease, prostate cancer in treatment with anti - androgen hormone therapy, came to our attention for worsening of constrictive chest pain at rest persisting for a month, for which he performed ECG exercise test positive. The patient did not report neither history of coronary heart disease nor intra-articular or intramuscular hemorrhage. He was admitted to the Department of Cardiology for practicing coronary angiography and eventually angioplasty and coronary stenting. During hospitalization, despite optimal anti-ischemic drug therapy (bisoprolol 2.5 mg, nitroglycerin patch of 10 mg, atorvastatin 80 mg, telmisartan 80 mg; Cardioaspirin 100 mg, the patient experienced recurrent episodes of constrictive chest pain with no changes of electrocardiogram and negative cardiac marker of necrosis. The level of FVIII activity, before the procedure, was 50% defining a very mild deficit. Catheterization was performed through the right radial artery with 6 F sheath. The coronary angiogram revealed the presence of 70% calcified stenosis of the left anterior descending artery at its middle part, involving the bifurcation of the first diagonal branch, with a calcific stenosis at its middle portion (Figure 1). During the procedure Bivalirudin was administered as a bolus and Clopidogrel loading dose of 600 mg was given before the procedure. PTCA and stenting with 2 Zotarolimus eluting stents DES 2.75 mm × 18 mm and 3.0 mm × 26 mm was performed using Minicrush technique (Figure 2A). Lastly, we performed a post-dilation with kissing balloon technique with non-compliant balloons, 5 mm × 15 mm (on the LAD) and 3.0 mm × 15 mm (on the diagonal branch). The final angiographic result was excellent with TIMI flow 3 (Figure 2B). The hemostasis at the puncture site was performed using Radistop, which was removed after eight hours without evidence of bleeding or hematoma. After the procedure, the patient was monitored in the Cardiology ward and the clinical conditions were good and hemodynamically stable during the hospitalization. In particular, there were no bleeding or further episodes of chest pain. The patient was discharged after 72 h of observation on DAPT (Aspirin 100 mg/d; Clopidogrel 75 mg/d) for one year, in addition to anti ischemic therapy previously reported. At six months follow up, the patient did not report any major bleedings and was asymptomatic.
PTCA in hemophiliacs has a greater risk of bleeding than in general population for many reasons. Arterial puncture is related to high risk of local complications, reduced by recombinant FVIII administration, by radial artery puncture and using effective hemostasis system for the puncture site. The management of unstable angina in hemophiliacs is suggested by a Consent Document of the World Federation of Hemophilia[6]. Experts recommend levels of FVIII activity of 80%, during the PTCA, and in the following 48 h, achieved through the infusion of recombinant FVIII, but this increases the risk of acute thrombosis in patients with unstable plaques. Many cases of myocardial infarction have been described during administration of coagulation factor concentrates, prothrombin complex and desmopressin[5,7]. Moreover, Girolami et al[4,5] have shown that most of thrombotic cardiovascular events in hemophiliac patients occur during the infusion of recombinant FVIII or desmopressin.
In the reported case, we decided to not pretreat the patient with replacement therapy, taking in account the clinical history free of major bleeding and the level of FVIII activity. To improve procedural safety, we undertook angiography using a radial approach, minimizing the risk of local complications. As anticoagulant during the interventional procedure we used Bivalirudin, a direct thrombin inhibitor, associated with lower rate of bleeding and with positive results in hemophiliac patient. Antiplatelet agents are needed to prevent in-stent thrombosis. The current guidelines suggest 1 year of dual antiplatelet therapy (DAPT) for DES and one month for bare metal stent[8]. Considering that Haemophilia is not associated with any platelet defect, antiplatelet agents should be given according to guidelines: indeed, acute stent thrombosis in patients with coagulation defects not receiving DAPT after stenting have been described in literature[9]. In the past BMS were preferred to DES for the shorter duration of DAPT[10]. New generation of DES do not need long-term DAPT, making treatment duration similar to that required for BMS. Moreover, drug-coated stent demonstrates superior safety and efficacy with one month of DAPT in patients at high bleeding risk[10].
In summary, we described the case of a patient with mild Haemophilia A presenting with unstable angina, treated with PTCA and stenting of the LAD at a bifurcation site with DES. The procedure was carried out safely, using the new generation DES. After six months of follow up the patient was in therapy with DAPT and had not experienced any complications and had no FVIII replacement.
A 55-year-old age man with mild deficit of factor VIII (FVIII) activity came to the authors’ attention for worsening of constrictive chest pain at rest persisting for a month.
Unstable angina in patient with mild hemophilia.
Acute myocardial infarction, atypical chest pain.
Deficit of FVIII activity.
The coronary angiogram revealed the presence of 70% calcified stenosis of the left anterior descending artery.
Unstable angina due to significant stenosis of one epicardial coronary artery.
Angioplasty and stenting of the coronary stenosis, dual antiplatelet treatment for one year.
Hemophilia A is an X-linked recessive disorder characterized by a deficiency of coagulation FVIII and therefore by a greater risk of bleeding. Angioplasty and stenting is more dangerous in this population and also the use of anticoagulants and antiplatelet agents.
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty, is a minimally invasive, endovascular procedure to widen narrowed or obstructed arteries.
Guidelines about the management of acute coronary syndrome in hemophiliacs don’t exist, and their treatment should be tailored. Mild hemophilia should be not pretreat with recombinant factor therapy, considering the low bleeding risk.
This case report is very interesting and clinically relevant.
Manuscript source: Unsolicited manuscript
Specialty type: Hematology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Classen CF, Moschovi MA, Sato A, Zimmer J S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Darby SC, Kan SW, Spooner RJ, Giangrande PL, Hill FG, Hay CR, Lee CA, Ludlam CA, Williams M. Mortality rates, life expectancy, and causes of death in people with hemophilia A or B in the United Kingdom who were not infected with HIV. Blood. 2007;110:815-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 375] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 2. | Kulkarni R, Soucie JM, Evatt BL. Prevalence and risk factors for heart disease among males with hemophilia. Am J Hematol. 2005;79:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 98] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:188-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 912] [Cited by in RCA: 950] [Article Influence: 73.1] [Reference Citation Analysis (0)] |
| 4. | Girolami A, Randi ML, Ruzzon E, Zanon E, Girolami B. Myocardial infarction, other arterial thrombosis and invasive coronary procedures, in hemaophilia B: a critical evaluation of reported cases. J Thromb Thrombolysis. 2005;20:43-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Girolami A, Ruzzon E, Fabris F, Varvarikis C, Sartori R, Girolami B. Myocardial infarction and other arterial occlusions in hemophilia a patients. A cardiological evaluation of all 42 cases reported in the literature. Acta Haematol. 2006;116:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | Ferraris VA, Boral LI, Cohen AJ, Smyth SS, White GC. Consensus review of the treatment of cardiovascular disease in people with hemophilia A and B. Cardiol Rev. 2015;23:53-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Fefer P, Gannot S, Lubetsky A, Martinowitz U, Matetzky S, Guetta V, Segev A. Percutaneous coronary intervention in patients with haemophilia presenting with acute coronary syndrome: an interventional dilemma: case series, review of the literature, and tips for management. J Thromb Thrombolysis. 2013;35:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4045] [Cited by in RCA: 4391] [Article Influence: 439.1] [Reference Citation Analysis (0)] |
| 9. | Bovenzi F, De Luca L, Signore N, Fusco F, de Luca I. Abciximab for the treatment of an acute thrombotic coronary occlusion during stent implantation in a patient with severe hemophilia B. Ital Heart J. 2003;4:728-730. [PubMed] |
| 10. | Kolh P, Windecker S, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014;46:517-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 591] [Article Influence: 53.7] [Reference Citation Analysis (0)] |