Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.713
Revised: May 29, 2024
Accepted: June 25, 2024
Published online: August 18, 2024
Processing time: 183 Days and 19.1 Hours
Total knee arthroplasty (TKA) can improve pain, quality of life, and functional outcomes. Although uncommon, postoperative complications are extremely consequential and thus must be carefully tracked and communicated to patients to assist their decision-making before surgery. Identification of the risk factors for complications and readmissions after TKA, taking into account common causes, temporal trends, and risk variables that can be changed or left unmodified, will benefit this process.
To assess readmission rates, early complications and their causes after TKA at 30 days and 90 days post-surgery.
This was a prospective and retrospective study of 633 patients who underwent TKA at our hospital between January 1, 2017, and February 28, 2022. Of the 633 patients, 28 were not contactable, leaving 609 who met the inclusion criteria. Both inpatient and outpatient hospital records were retrieved, and observations were noted in the data collection forms.
Following TKA, the 30-day and 90-day readmission rates were determined to be 1.1% (n = 7) and 1.8% (n = 11), respectively. The unplanned visit rate at 30 days following TKA was 2.6% (n = 16) and at 90 days was 4.6% (n = 28). At 90 days, the unplanned readmission rate was 1.4% (n = 9). Reasons for readmissions included medical (27.2%, n = 3) and surgical (72.7%, n = 8). Unplanned readmissions and visits within 90 days of follow-up did not substantially differ by age group (P = 0.922), body mass index (BMI) (P = 0.633), unilateral vs bilateral TKA (P = 0.696), or patient comorbidity status (30-day P = 0.171 and 90-day P = 0.813). Reoperation rates after TKA were 0.66% (n = 4) at 30 days and 1.15% (n = 8) at 90 days. The average length of stay was 6.53 days.
In this study, there was a low readmission rate following TKA. There was no significant correlation between read
Core Tip: As the rates of total knee arthroplasty are currently increasing, there is a need to study the potential complications that may occur after the surgery. This study highlights the complications that occur postoperatively and potential risk factors that can contribute to the complications. It also assesses the relationship between age, sex, co-morbidities, length of stay, and early readmission after surgery, categorizing these readmissions by surgical and medical reasons depending on the type of treatment received by the patients.
- Citation: Jethi T, Jain D, Garg R, Selhi HS. Readmission rate and early complications in patients undergoing total knee arthroplasty: A retrospective study. World J Orthop 2024; 15(8): 713-721
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/713.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.713
Knee osteoarthritis (OA) is a chronic degenerative disorder of multifactorial etiology characterized by the loss of articular cartilage, hypertrophy of bone at the margins, subchondral sclerosis, and range of biochemical and morphological al
The risk factors for OA vary from person to person, including age, sex, obesity, genetics, diet, and joint injury, according to the stage of the disease[3]. It is difficult to distinguish between single and clustered risk factors associated with the development or progression of the disease.
There is no cure for OA, and most treatments aim to improve symptoms and function. Optimal management of pa
In most situations, TKA is indicated for patients who have chronic, severe symptoms that persist beyond the limits of all conservative and non-operative therapy options. TKA is contraindicated in patients suffering from local knee infection (sepsis) or ongoing remote (extra-articular) infection or bacteremia, vascular dysfunction, or neuroarthropathic degene
Demographic factors such as age, sex, and body mass index (BMI) have varying and complicated effects. Age intervals are not uniform among studies, with some using 5- or 10-year intervals, and others using a specific number. The classification of predictive factors by various studies when estimating risk, as well as increasing age, weight, and the physical activity of TKA patients, may complicate matters[8].
Complications occurring after TKA include the following: Thromboembolism, which is one of the most significant complications; deep venous thrombosis, which is one of the most serious and potentially life-threatening complications; pulmonary embolism, one of the most feared complications; and infection, which is rare, occurring in only 2% to 3% of cases. Patellofemoral complications after TKA include patellofemoral instability, patellar fracture, patellar component failure, patellar component loosening, patellar clunk syndrome, and extensor mechanism rupture. Neurovascular complications after TKA, such as arterial injury, are rare and occur in only 0.03% to 0.2% of patients, with 25% resulting in amputation. Periprosthetic supracondylar femur fractures after TKA are also infrequent (0.3% to 2%)[9].
As there is an increased rate of patients undergoing TKA, readmission rates have increased. Studying the risk factors helps us identify different preventable causes of readmission in TKA. In a population of TKA recipients, understanding the risk factors for readmission following joint arthroplasty helps clinicians better understand the postoperative course of their patients. Knowing the potential risks and mitigation strategies, as well as how to identify patients with the highest risk of readmission, will improve the effectiveness and efficiency of care[10].
The largest hospital readmission rates have been found to occur in the first 30 days after surgery, indicating that patients are at greatest risk of being readmitted to the hospital in the early phase of post-surgery. The reported 5%-8% readmission rate of patients after TKA is concerning[11]. Readmission may be an indication that patients were not thoroughly prepared for discharge after surgery and may have not fully understood the discharge instructions and guidelines for the postoperative phase, which could have supported better post-surgical outcomes[11].
Compared to the number of readmissions from day 31 to day 90, more 30-day readmissions have been reported as problems related to surgery; in particular, 71% of the issues during the first 30 days are related to surgery, as opposed to 47% of the remaining 60 days in a 90-day period. After completing joint replacement, 90 days is a preferable time period for recording readmissions due to surgery[12]. There is a prominent trend towards reduced hospital length of stay (LOS) after TKA. There has also been increased utilization of TKA surgery on an outpatient basis[13]. A short LOS is associated with higher 30-day readmission rates, and following an index surgery, LOS > 1 day increases the odds of 90-day readmission[14]; however, the optimal LOS after TKA remains a subject of debate.
There is limited literature on this topic in the Indian population. Thus, the present study was conducted to study the pattern of readmission in patients who underwent primary TKA in order to study complications and risk factors in this patient population.
The present prospective and retrospective study included patients who underwent TKA from January 1, 2017, through February 28, 2022, with a minimum follow-up of 3 months. Patients were contacted by either telephone or personal interview. Hospital in-patient and outpatient records were retrieved and data collection forms were filled.
The study included all patients who underwent primary TKA and excluded patients who underwent revision TKA and who were not willing to participate in the study. Readmission rates at 30 days and 90 days were assessed. Of the 633 patients, 28 were not able to be contacted, leaving 609 who met the inclusion criteria. Variables that were studied included time and reason for readmission, LOS, complications after TKA, and hospital visits not requiring admission to the hospital.
The average age of patients in the study was 62.87 years (range: 35-91 years), and 69% were females while 31% were males (Table 1). The majority (54.5%) of patients were overweight, of whom 4.6% had class 1 obesity; the remaining patients had normal BMI. The BMI range of patients in the study was 22 kg/m2 to 35.64 kg/m2, with a mean BMI of 26.7 kg/m2 (Table 1).
| Study variable | Cases, n | Percent, % | |
| Age in year | ≤ 40 | 5 | 0.8 |
| 41-50 | 43 | 7.1 | |
| 51-60 | 197 | 32.3 | |
| 61-70 | 251 | 41.2 | |
| 71-80 | 104 | 17.1 | |
| > 80 | 9 | 1.5 | |
| Sex | Female | 420 | 69 |
| Male | 189 | 31 | |
| Body mass index in kg/m2 | < 24.9 (normal) | 249 | 40.8 |
| 25-29.9 (overweight) | 332 | 54.5 | |
| > 30 (class 1 obesity) | 28 | 4.6 | |
| Diagnosis | Osteoarthritis | 593 | 97.4 |
| Rheumatoid arthritis | 16 | 2.6 | |
| Laterality | Bilateral | 304 | 49.9 |
| Unilateral | 305 | 50.1 | |
| Duration of complaint | < 1 | 3 | 0.5 |
| 1-2.0 | 26 | 4.3 | |
| 2-5.0 | 168 | 27.6 | |
| 5-10.0 | 239 | 39.2 | |
| > 10 | 173 | 28.4 | |
| Charlson comorbidity index | < 2 | 399 | 65.5 |
| 2-3.0 | 156 | 25.6 | |
| > 4 | 54 | 8.9 | |
| Length of stay in day | 6 | 297 | 48.8 |
| 7 | 306 | 50.2 | |
| 8 | 4 | 0.7 | |
| 10 | 1 | 0.2 | |
| 13 | 1 | 0.2 | |
Of the total patients who underwent TKA, 97.4% had OA and only 2.6% of patients had rheumatoid arthritis. In total, 304 of 609 patients underwent bilateral TKA and 305 patients underwent unilateral TKA, for a total of 913 operated knees. The majority of patients had Charlson co-morbidity scores < 2 (65.5%), indicating mild severity of the associated co-morbidity. Another (8.9%) patients had scores > 4, whereas (25.6%) had scores ranging from 2 to 3.0. The LOS in the hospital for most patients was 7 days, with a range of LOS from 6 days to 13 days; the average LOS was 6.53 days. The majority of patients undergoing TKA had complaints for 2-10 years (2-5 years: 27.6%; 5-10 years: 39.2%). A total of 4.8% of patients had complaints for less than 2 years, whereas 28.4% had complaints for more than 10 years (Table 1).
In our study, 16 of the 28 unplanned visits occurred within the first 30 days after TKA, comprising 2.6% of total cases (Table 2).
| Unplanned visit after TKA within 30 days | Follow-up | Cases, n | Percent, % | |
| Occurred | No | 593 | 97.40 | |
| Yes | 16 | 2.60 | ||
| Reason | Febrile illness | 2 | 0.40 | |
| Urinary tract infection | 2 | 0.40 | ||
| Neurological issues | 1 | 0.20 | ||
| Lower back ache | 1 | 0.20 | ||
| Post TKA pain | 3 | 0.60 | ||
| Wound complications | 5 | 1.00 | ||
| Other surgery-related complications | 2 | 0.40 |
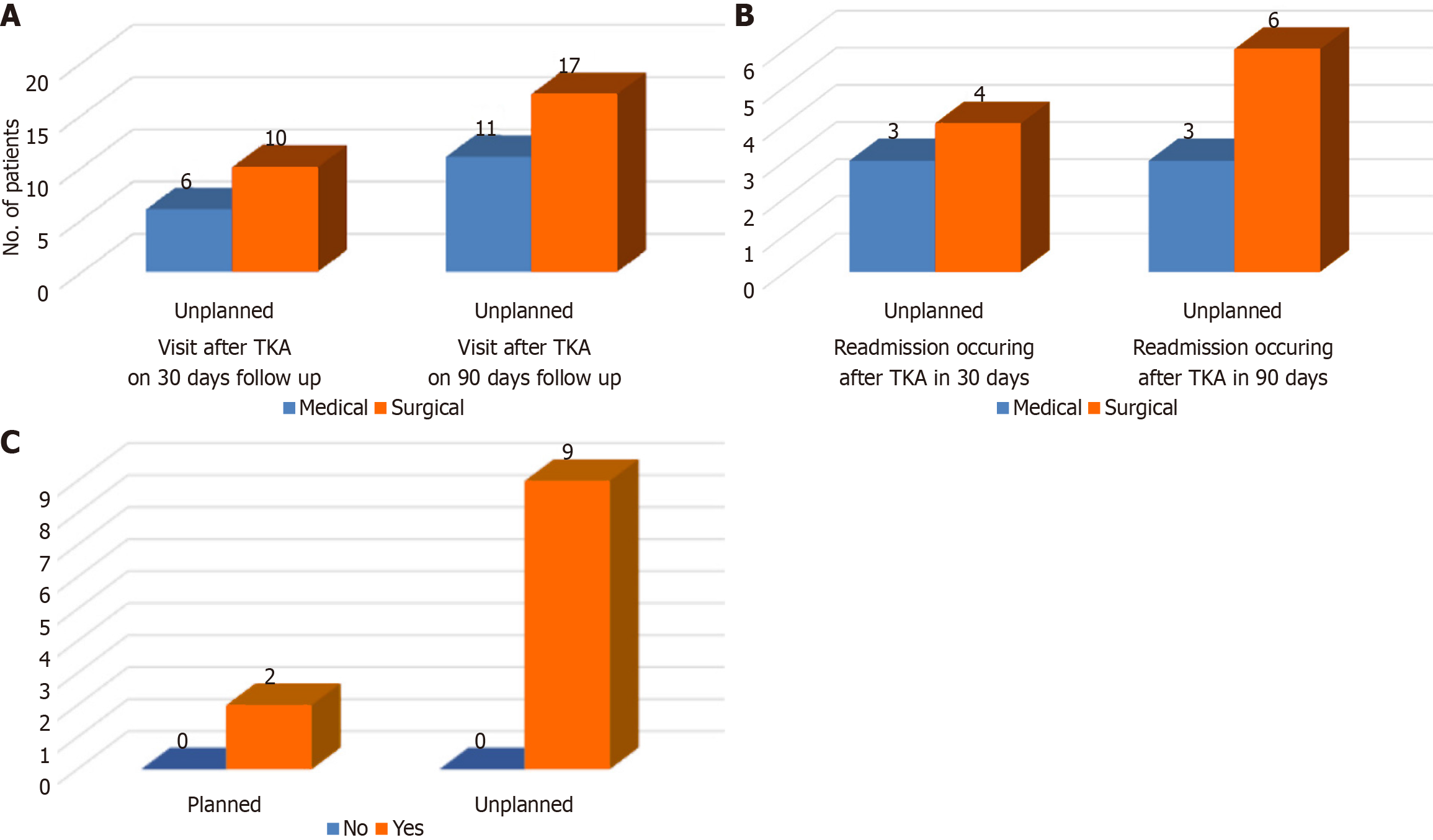
Of the 16 unplanned visits, there were 7 unplanned readmissions, occurring in the first 30 days of TKA. The rate of readmission in the first 30 days of follow-up was found to be 1.1%. In our 90-day follow-up, there were a total of 28 unplanned visits to the hospital, and the rate of unplanned visits was found to be 4.6% (Table 3). The reasons for unplanned visits at the 30-day and 90-day follow-up are depicted in Figure 1A. In our 90-day post-TKA follow-up, there were 11 readmissions, 2 of which were planned and 9 of which were unplanned, yielding a readmission rate of 1.8% (n = 11) and an unplanned readmission rate of 1.4% (n = 9). The reasons for readmission at the 30-day and 90-day follow-up are illustrated in Figure 1B (Table 4).
| Unplanned visit after TKA within 90 days | Follow-up | Cases, n | Percent, % |
| Occurred | No | 815 | 95.40 |
| Yes | 8 | 4.60 | |
| Reason for unplanned visits within 90 days | Febrile illness | 3 | 0.60 |
| Urinary tract infection | 3 | 0.60 | |
| Neurological issues | 2 | 0.40 | |
| Generalized body weakness | 1 | 0.20 | |
| Lower back ache | 2 | 0.40 | |
| Soft tissue injury over knee | 2 | 0.40 | |
| Post TKA pain | 7 | 1.40 | |
| Wound complications | 5 | 1.00 | |
| Other surgery-related complication | 3 | 0.60 |
| Reasons for readmissions within 90 days | Cases, n | Percent, % |
| Febrile illness | 2 | 0.40 |
| Neurological issues | 2 | 0.40 |
| Talonavicular degeneration | 1 | 0.20 |
| Soft tissue injury over the knee | 2 | 0.40 |
| Wound complications | 4 | 0.80 |
The 30-day and 90-day reoperation rates after TKA were 0.66% (n = 4) and 1.15% (n = 8), respectively (Table 5).
| Readmission after TKA | On 30-day follow-up | On 90-day follow-up |
| Our study | 1.1% (n = 7) | 1.8% (n = 11) |
| Urish et al[19] | 4% (n = 703) | 5.8% (n = 1209) |
| Cassard et al[16] | 3.3% (n = 2) outpatient | NA |
| 4.9% (n = 25) inpatient | ||
| Avram et al[15] | 2% (n = 55) | NA |
| Workman et al[26] | 2.8% (n = 210) | NA |
| Ali and Bottle[21] | 6.0% (n = 37195) | NA |
| D'Apuzzo et al[22] | 5.8% (n = 22076) | NA |
Unplanned readmissions and visits within 90 days of follow-up after TKA did not significantly correlate with age group
There were no mortalities at the 30-day and 90-day follow-ups.
There was a low readmission rate following TKA. There was no significant correlation between readmission rates at the 90 days follow-up and patient factors such as age, BMI, and co-morbidity status. Comparisons of unplanned readmissions after TKA with other studies are shown in Table 6.
| Unplanned readmission after TKA | On 30-day follow-up | On 90-day follow-up |
| In our study | 1.1% (n = 7) | 1.4% (n = 9) |
| Schairer et al[18] | 4% (n = 57) | 8% (n = 118) |
| Urish et al[19] | 4% (n = 703) | 5.8% (n = 1209) |
| Cassard et al[16] | 3.3% (n = 2) outpatient | NA |
| 4.9% (n = 25) inpatient | ||
| D'Apuzzo et al[22] | 5.8% (n = 22076) | NA |
| Odum and Springer[27] | 12% outpatient1 | NA |
| 6% inpatient1 | ||
| Ali and Bottle[21] | 6.0% (n = 37195) | NA |
| Workman et al[26] | 2.8% (n = 210) | NA |
| Avram et al[15] | 2% (n = 55) | NA |
| Yohe et al[20] | 4.7% (n = 566) | NA |
The current study enrolled 633 patients who underwent TKA between January 1, 2017, through February 28, 2022, 28 of whom were excluded as they could not be reached. The mean patient age was 62.87 years. The average age of readmitted patients was 63 years. No positive correlation was found between age and unplanned visits and readmissions at 90 days following TKA (P = 0.922). The average age of readmitted patients in this study is in the range of that reported in pre
Yohe et al[20] examined the rate and risks of 30-day complications and unplanned readmissions in patients older than 80 years and concluded that patients older than 84 years are at higher risk of minor complications than those aged 80 years to 84 years. Ali and Bottle[21], D'Apuzzo et al[22], and Gould et al[23] showed that increasing age is associated with a significant and progressive increase in the risk of all-cause readmission for all age groups. Schairer et al[18] showed no differences in age between patients who were or were not readmitted.
In patients undergoing TKA, females predominate over males. In our study, male patients had significantly higher co-morbidities (P = 0.003). The study by Ali and Bottle[21] showed that males had a significantly higher risk of readmission for all types of readmissions. D'Apuzzo et al[22], Gould et al[23], and Urish et al[19] showed that male patients had a higher risk of readmission independent of other risk factors. The study by Yohe et al[20] showed that male patients had a lower risk than female patients for minor complications postoperatively after TKA. Schairer et al[18] concluded that there was no relationship between sex type and patient readmission rate in their study.
In our study, 32.8% of patients suffered from hypertension. Other associated co-morbidities found in a minority of patients were type 2 diabetes (14.4%), coronary artery disease (4.4%), asthma (0.3%), hypothyroidism (2.6%), and rheu
There was no significant correlation between the co-morbidity status of patients and unplanned readmissions at 30 days (P = 0.171) and 90 days (P = 0.813), or between co-morbidity status and unplanned visits at 30 days (P = 0.363) and 90 days (P = 0.554). Benito et al[14] concluded in their study that diabetes and coronary artery disease represent potential risk factors for 90-day readmission after TKA. In their systematic review and meta-analysis, Gould et al[23] included 69 studies in which risk factors associated with 30-day readmission were hypertension, congestive heart failure, diabetes, an elevated preoperative international normalized ratio, elevated serum blood urea nitrogen, reduced serum albumin, depression, drug abuse, a history of cancer, and chronic kidney disease. A review on readmission rates by Fischer et al[24] found that, for certain diseases such as heart failure, the patient’s condition is the major driver behind repeated ad
In our study, 5 of 609 patients had developed a surgical site wound complication that prompted unplanned visits at the 30-day follow-up. Of these patients, 4 had been readmitted and required surgical intervention, with 1 patient having developed erythema at the surgical site, 1 having bleeding from the suture line, and 2 patients having discharge from the suture line. Three of these patients were managed with knee arthrotomy and lavage and one with debridement with vacuum-assisted closure (VAC) application. A total of 2 of 609 patients were admitted with soft tissue injuries requiring readmission between 30 days and 90 days after TKA. In all, 28 of 609 patients had an unplanned visit to the hospital within 90 days of TKA; specifically, 16 (2.6%) of the 28 unplanned visits occurred within the first 30 days of TKA. Ten of the unplanned visits within the first 30 days of TKA were for surgical reasons, whereas the remaining six were for medical reasons. In our 90-day follow-up after TKA, of the 28 (4.6%) unplanned visits, 17 were due to surgical reasons and 11 were due to medical reasons. Cassard et al[16] found that unplanned visits to the hospital within 30 days of TKA was 4.8% (n = 3) in the outpatient setting and 2.4% (n = 12) in the inpatient setting. In our study, 11 of the 609 (1.8%) patients were readmitted to the hospital in the 90 days follow-up period. Of the 11 patients, 2 had a planned readmission and 9 had an unplanned readmission. Of these 11 readmissions, there were a total of 7 (1.1%) unplanned readmissions that occurred within the first 30 days of TKA and no planned readmissions. Of the seven unplanned readmissions, two were due to febrile illnesses, which were managed with oral antibiotics with packed red blood cell transfusion and intravenous antibiotics, respectively, one was due to stroke, for which anticoagulants and thrombolytics were given, and four were due to wound-related complications, which were managed with knee arthrotomy and lavage and debridement with VAC application. Three of these unplanned readmissions occurred for medical reasons and four were due to sur
In our 30-day to 90-day follow-up period, four readmissions occurred, of which two were planned and two were unplanned; one was due to a spine tumor, which was excised, one was due to talonavicular degeneration, which was managed with ankle arthrodesis, and two were due to soft tissue injuries over the knee, which were managed with wound wash and suturing and debridement and VAC application, respectively. All patients were discharged to their homes.
Re-operation rates in the 30-day and 90-day follow-up after TKA were found to be 0.66% (n = 4) and 1.15% (n = 8), respectively. Unplanned readmissions and visits within 90 days of follow-up did not significantly correlate with age group (P = 0.922), BMI (P = 0.633), or unilateral vs bilateral TKA (P = 0.696). Unplanned readmissions within the first 30 days after TKA and data on unplanned visits within the first 30 days of follow-up following TKA were not substantial enough for a correlation to be identified.
Reduced LOS after TKA is a noticeable trend in the Western world. The use of TKA as an outpatient procedure has also increased. Because most patients are transferred to nursing homes or inpatient rehabilitation facilities in the west, the average LOS is shorter. Low LOS was linked to greater 30-day readmission rates in studies by Ali and Bottle[21] and Cram et al[25]. In India, many patients are discharged home with limited access to medical care, which justifies a longer LOS and adequate optimization (physiotherapy, wound dressings, intravenous antibiotics) of patients before discharge. In our study, there was a low rate of unplanned visits and readmissions, as patients were optimized following surgery before being discharged. However, additional studies with a larger sample size are needed in the Indian population to determine the effect of LOS on readmission and other factors that affect readmission rates.
In our study, patients had a low readmission rate following TKA. There was no significant correlation between read
The author would like to express their gratitude to Dr. Deepak Jain (Professor, Department of Orthopaedics, DMC & H, Ludhiana) for mentoring guidance and Dr. Rajnish Garg (Professor and Head, Department of Orthopaedics, DMC & H, Ludhiana) for additional scholarly guidance in the completion of this study.
| 1. | Firestein GS, Budd RC, Gabriel SE, McInnes IB, O'Dell JR. Etiology and Pathogenesis of Rheumatoid Arthritis. In: Koretzky G, editor. Kelley's Textbook of Rheumatology. 11th ed. Elsevier, 2020. |
| 2. | Courtney PM, Rozell JC, Melnic CM, Lee GC. Who Should Not Undergo Short Stay Hip and Knee Arthroplasty? Risk Factors Associated With Major Medical Complications Following Primary Total Joint Arthroplasty. J Arthroplasty. 2015;30:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Abramoff B, Caldera FE. Osteoarthritis: Pathology, Diagnosis, and Treatment Options. Med Clin North Am. 2020;104:293-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 661] [Article Influence: 132.2] [Reference Citation Analysis (0)] |
| 4. | Gross DE, Brenner SL, Esformes I, Gross ML. Arthroscopic treatment of degenerative joint disease of the knee. Orthopedics. 1991;14:1317-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975-1997: an update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop Scand. 2001;72:503-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 251] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 6. | Hsu H, Siwiec RM. Knee Arthroplasty. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 7. | Varacallo M, Luo TD, Mabrouk A, Johanson NA. Total Knee Arthroplasty Techniques. 2024 May 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 8. | Gould D, Dowsey MM, Spelman T, Jo O, Kabir W, Trieu J, Bailey J, Bunzli S, Choong P. Patient-Related Risk Factors for Unplanned 30-Day Hospital Readmission Following Primary and Revision Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Courtney PM, Boniello AJ, Berger RA. Complications Following Outpatient Total Joint Arthroplasty: An Analysis of a National Database. J Arthroplasty. 2017;32:1426-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 206] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 10. | Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374:1543-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 646] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 11. | Pamilo KJ, Torkki P, Peltola M, Pesola M, Remes V, Paloneva J. Fast-tracking for total knee replacement reduces use of institutional care without compromising quality. Acta Orthop. 2018;89:184-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Which Hospital and Clinical Factors Drive 30- and 90-Day Readmission After TKA? J Arthroplasty. 2016;31:2099-2107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | Bozic KJ, Chiu V. Emerging ideas: Shared decision making in patients with osteoarthritis of the hip and knee. Clin Orthop Relat Res. 2011;469:2081-2085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Benito J, Stafford J, Judd H, Ng M, Corces A, Roche MW. Length of Stay Increases 90-day Readmission Rates in Patients Undergoing Primary Total Joint Arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 2022;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 15. | Avram V, Petruccelli D, Winemaker M, de Beer J. Total joint arthroplasty readmission rates and reasons for 30-day hospital readmission. J Arthroplasty. 2014;29:465-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Cassard X, Garnault V, Corin B, Claverie D, Murgier J. Outpatient total knee arthroplasty: Readmission and complication rates on day 30 in 61 patients. Orthop Traumatol Surg Res. 2018;104:967-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Schmidt AM, Garval M, Gromov K, Holm C, Larsen JR, Runge C, Vase M, Mikkelsen LR, Mortensen L, Skou ST. Feasibility, safety, and patient-reported outcomes 90 days after same-day total knee arthroplasty: a matched cohort study. Acta Orthop. 2022;93:509-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 18. | Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2014;472:181-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 192] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 19. | Urish KL, Qin Y, Li BY, Borza T, Sessine M, Kirk P, Hollenbeck BK, Helm JE, Lavieri MS, Skolarus TA, Jacobs BL. Predictors and Cost of Readmission in Total Knee Arthroplasty. J Arthroplasty. 2018;33:2759-2763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 20. | Yohe N, Funk A, Ciminero M, Erez O, Saleh A. Complications and Readmissions After Total Knee Replacement in Octogenarians and Nonagenarians. Geriatr Orthop Surg Rehabil. 2018;9:2151459318804113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Ali AM, Bottle A. The Validity of All-Cause 30-Day Readmission Rate as a Hospital Performance Metric After Primary Total Hip and Knee Arthroplasty: A Systematic Review. J Arthroplasty. 2019;34:1831-1836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | D'Apuzzo M, Westrich G, Hidaka C, Jung Pan T, Lyman S. All-Cause Versus Complication-Specific Readmission Following Total Knee Arthroplasty. J Bone Joint Surg Am. 2017;99:1093-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 23. | Gould D, Dowsey M, Spelman T, Jo I, Kabir W, Trieu J, Choong P. Patient-related risk factors for unplanned 30-day readmission following total knee arthroplasty: a protocol for a systematic review and meta-analysis. Syst Rev. 2019;8:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Fischer C, Lingsma HF, Marang-van de Mheen PJ, Kringos DS, Klazinga NS, Steyerberg EW. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS One. 2014;9:e112282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 196] [Cited by in RCA: 203] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 25. | Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308:1227-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 674] [Cited by in RCA: 734] [Article Influence: 56.5] [Reference Citation Analysis (0)] |
| 26. | Workman KK, Angerett N, Lippe R, Shin A, King S. Thirty-Day Unplanned Readmission after Total Knee Arthroplasty at a Teaching Community Hospital: Rates, Reasons, and Risk Factors. J Knee Surg. 2020;33:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Odum SM, Springer BD. In-Hospital Complication Rates and Associated Factors After Simultaneous Bilateral Versus Unilateral Total Knee Arthroplasty. J Bone Joint Surg Am. 2014;96:1058-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |