Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.696
Revised: June 29, 2024
Accepted: July 8, 2024
Published online: August 18, 2024
Processing time: 81 Days and 17.5 Hours
Normal vertical and horizontal offset is essential for hip biomechanics, muscle functioning and gait pattern. Total hip arthroplasty (THA) should aim to restore normal offset with implantation of femoral and acetabular components. This would be possible with proper preoperative planning, templating and ensuring implant options are available for offset restoration. Templating is essential for understanding the vertical and horizontal offset change, especially in hip arthritis presenting late with significant limb length discrepancy at THA. Planning should include appropriate soft tissue releases and the use of ideal implants to achieve restoration of horizontal and vertical offset. Under correction of horizontal offset at THA for fracture neck of femur could result in abductor fatigue, limp and increased wear. Restoration of horizontal offset is imperative at THA for a frac
Core Tip: Total hip arthroplasty (THA) requires careful attention to achieve restoration of both the vertical and horizontal offset. The vertical offset is critical to establish the correct limb length; inadequate restoration of vertical offset results in limb length discrepancy and poor clinical outcomes. The horizontal offset plays a role in obtaining optimal abductor tension and function, allowing for normal gait. Failure to achieve normal horizontal offset leads to sub-optimal abductor function, fatigue, limp, increased wear, and possible THA instability. Pre-operative templating and intra-operative execution of this plan allow for offset restoration, appropriate soft-tissue releases, and suitable implant selection, which ultimately results in hip center restoration and recreation of normal hip biomechanics.
- Citation: Oommen AT. Offset restoration in total hip arthroplasty: Important: A current review. World J Orthop 2024; 15(8): 696-703
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/696.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.696
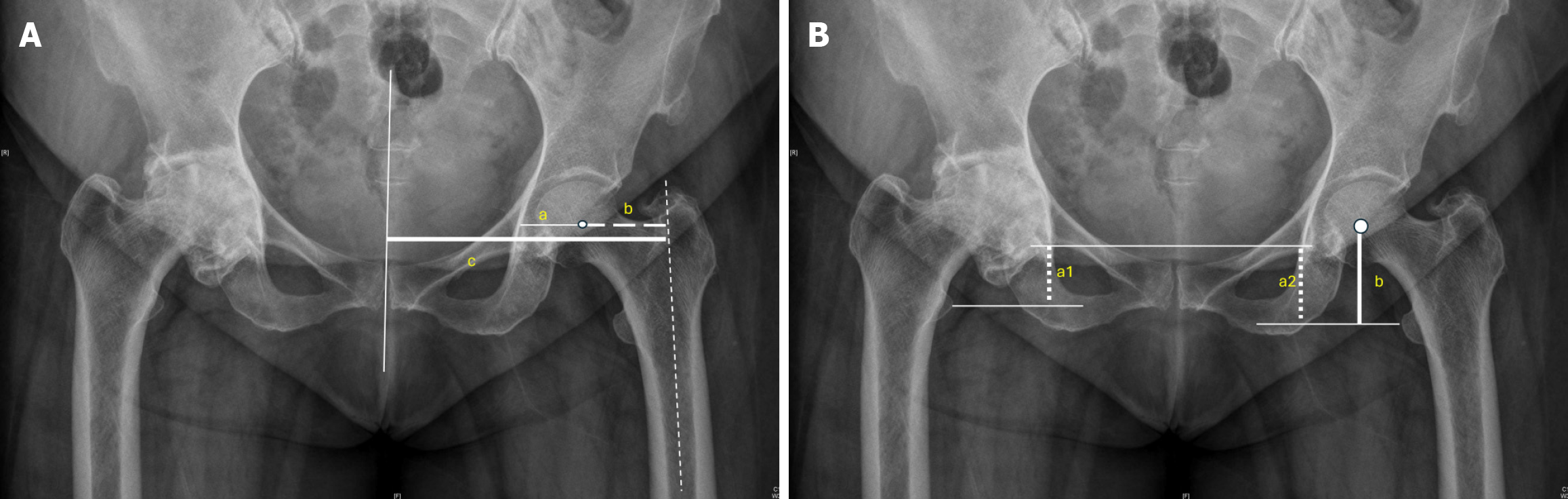
Total hip arthroplasty (THA) aims to restore biomechanics and function as close as possible to the native hip[1]. This can be accurately achieved by restoring the acetabular inclination, version and, more importantly, the center of rotation (COR). The correct COR allows for the establishment of the acetabular, femoral, and global offset. Acetabular offset is measured from the COR to the true floor of the acetabulum or to the center of the pelvis. Femoral offset is defined as the distance from the COR to the center of the femoral canal. In this horizontal plane, the combination of acetabular and femoral offset is defined as a global offset.
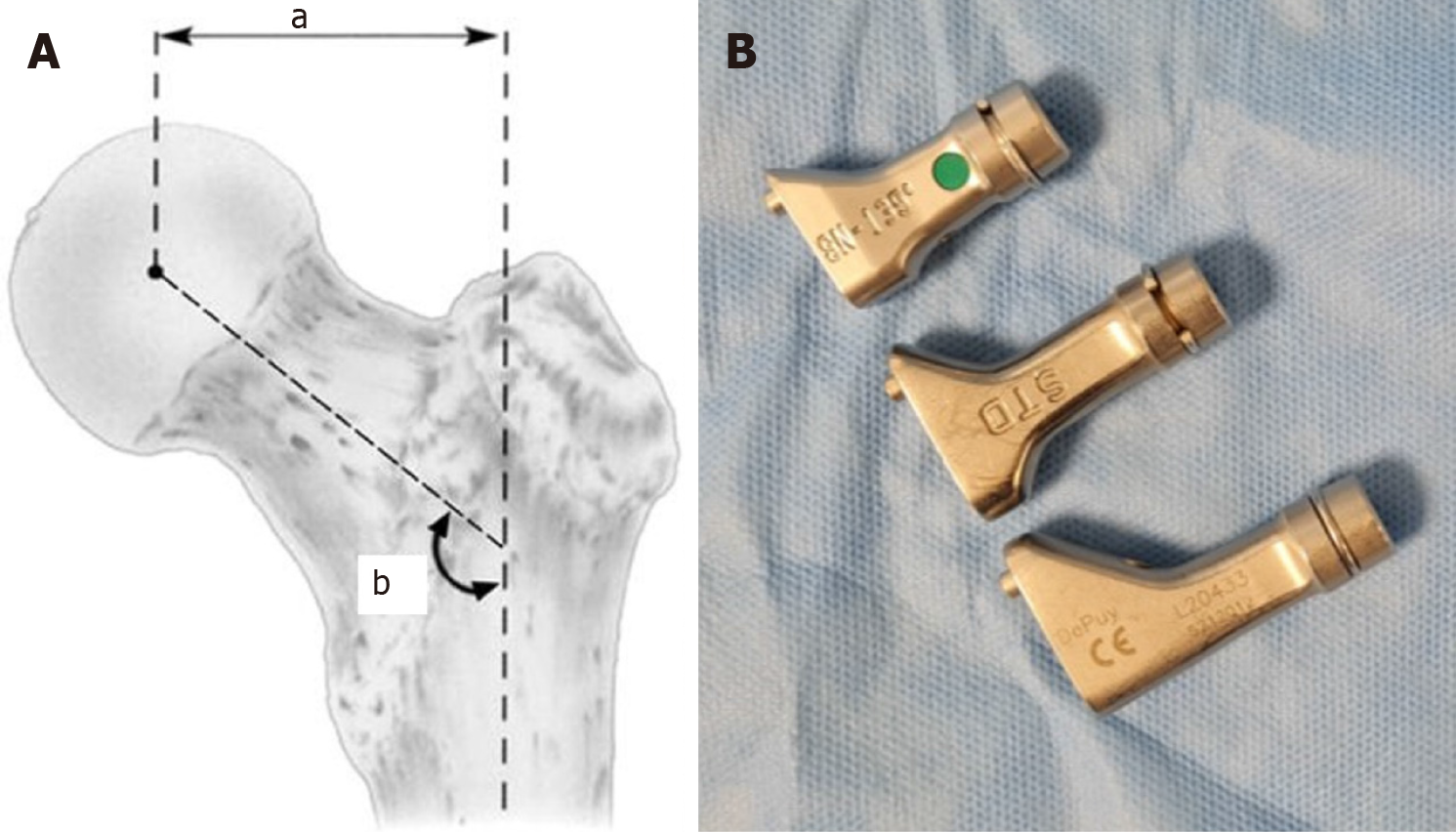
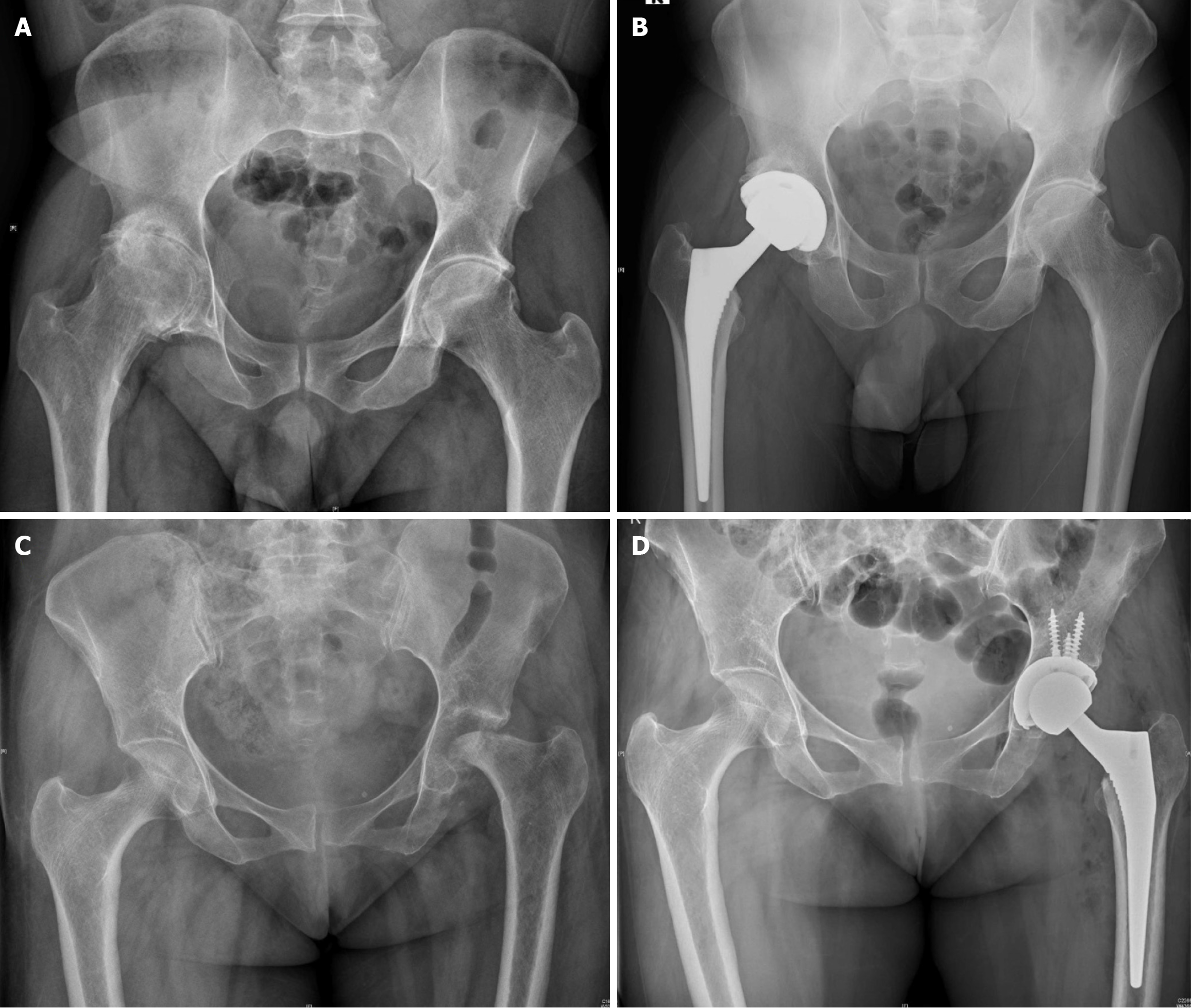
Once the COR has been established, both horizontal and vertical offset restoration is required for the recreation of native hip biomechanics (Figures 1 and 2)[1–5]. The acetabular, femoral, and global offsets are ideally templated pre-operatively, assessed intra-operatively, and critiqued post-operatively to ensure ideal correction. Adequate horizontal offset is necessary for optimal functioning of the abductors (Figure 3); a decrease in horizontal offset could lead to abductor fatigue and a persistent Trendelenberg gait. Hip function significantly improves with proper restoration of horizontal offset[1]. Improper restoration of vertical offset can result in limb length discrepancy, resulting in an unhappy patient.
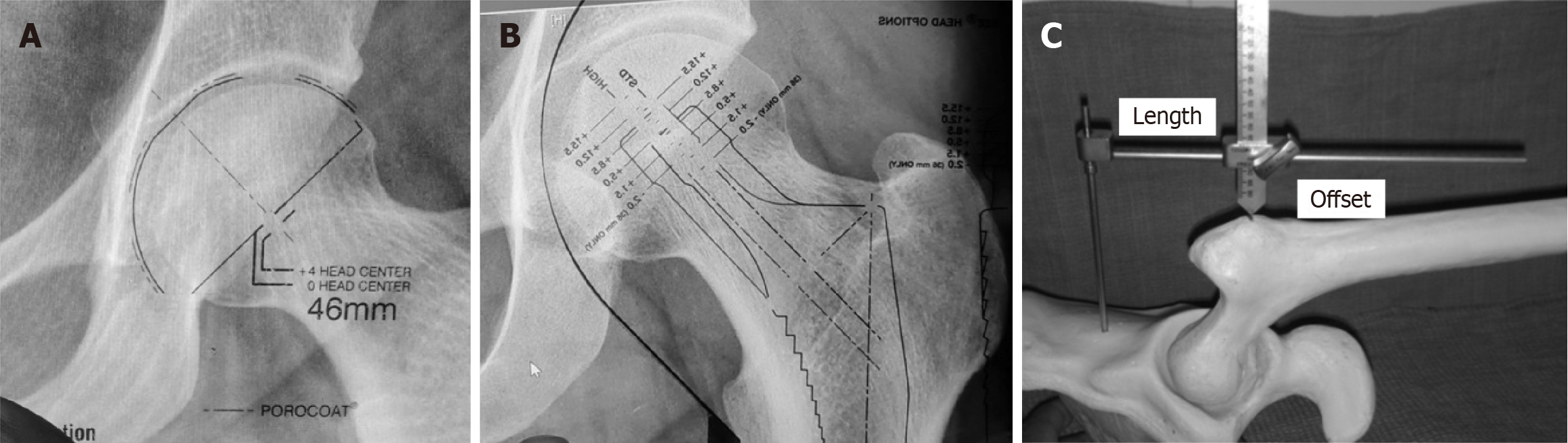
Planning for THA includes pre-operative templating, which must be corroborated with the intra-operative findings. The size of the femoral and acetabular components and the offset requirements are assessed to enable restoration of normal hip biomechanics, leg length and hip center restoration.
Two-dimensional templating can be done routinely in almost all centers, while 3D-templating requires technology-assisted THA. Three-dimensional templating could prove to be more precise. However, 2D templating provides reliable information for intra-operative assessment[6–8].
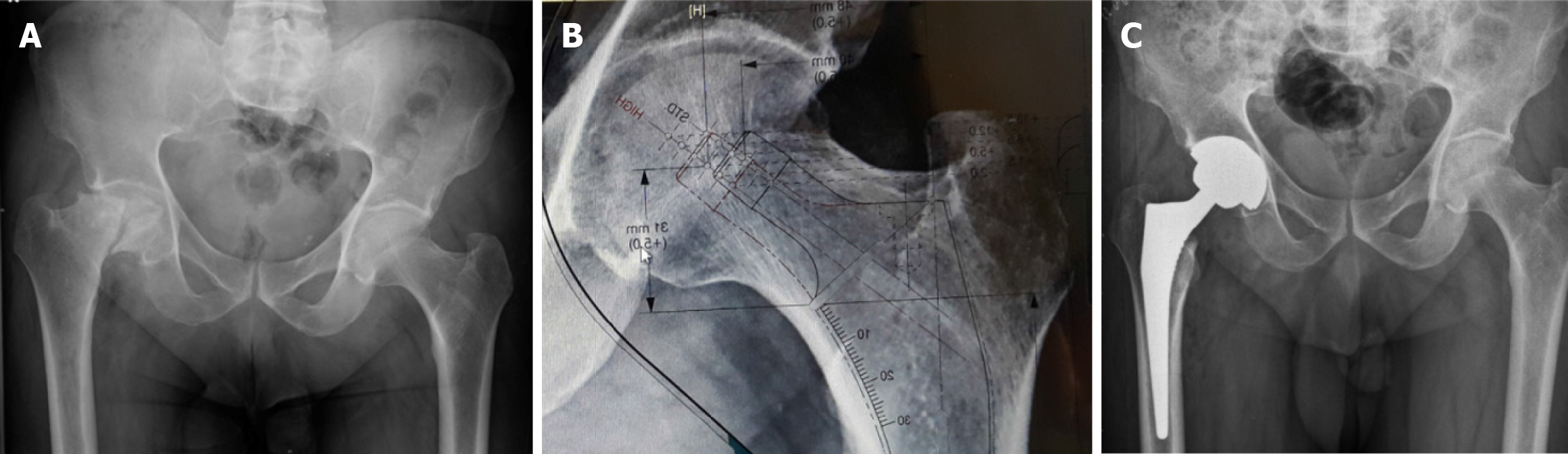
Templating provides valuable information regarding the position of the COR and femoral offset, as well as the proposed sizing and position of the acetabular and femoral components. The various trial offset options can restore the horizontal offset before the femoral component is implanted (Figures 3 and 4). Pre-operative planning should be done with specific attention to restoring the COR and matching options to restore the horizontal and vertical offset (Figure 2B).
Acetabular true floor identification is important intra-operatively to ensure appropriate reaming, medialization, and COR restoration. The appropriate medialization with the restoration of the femoral offset would be ideal for restoring the hip global offset, outcome and function[1]. Reduction in global offset could lead to impingement, instability and increased risk of dislocation[1].
Patient-specific restoration is possible with proper templating and pre-operative planning[6,7,9,10]. Individual hip biomechanics can be restored with information gleaned from proper pre-operative templating. Trial implants can be used to ascertain the ideal options before final component implantation. An increase in neck length would achieve correction of both the horizontal and vertical offset, resulting in increased offset and soft-tissue irritation (e.g. trochanteric bursitis) and an undesired limb length discrepancy. A high offset stem would only change the horizontal offset without affecting the limb length (Figures 5 and 6). Functional joint scores have been reported as better with minimal increase in the acetabular and global offset[7]. Under correction or increase in offset can be avoided by careful pre-operative templating and intra-operative execution (Figure 2B).
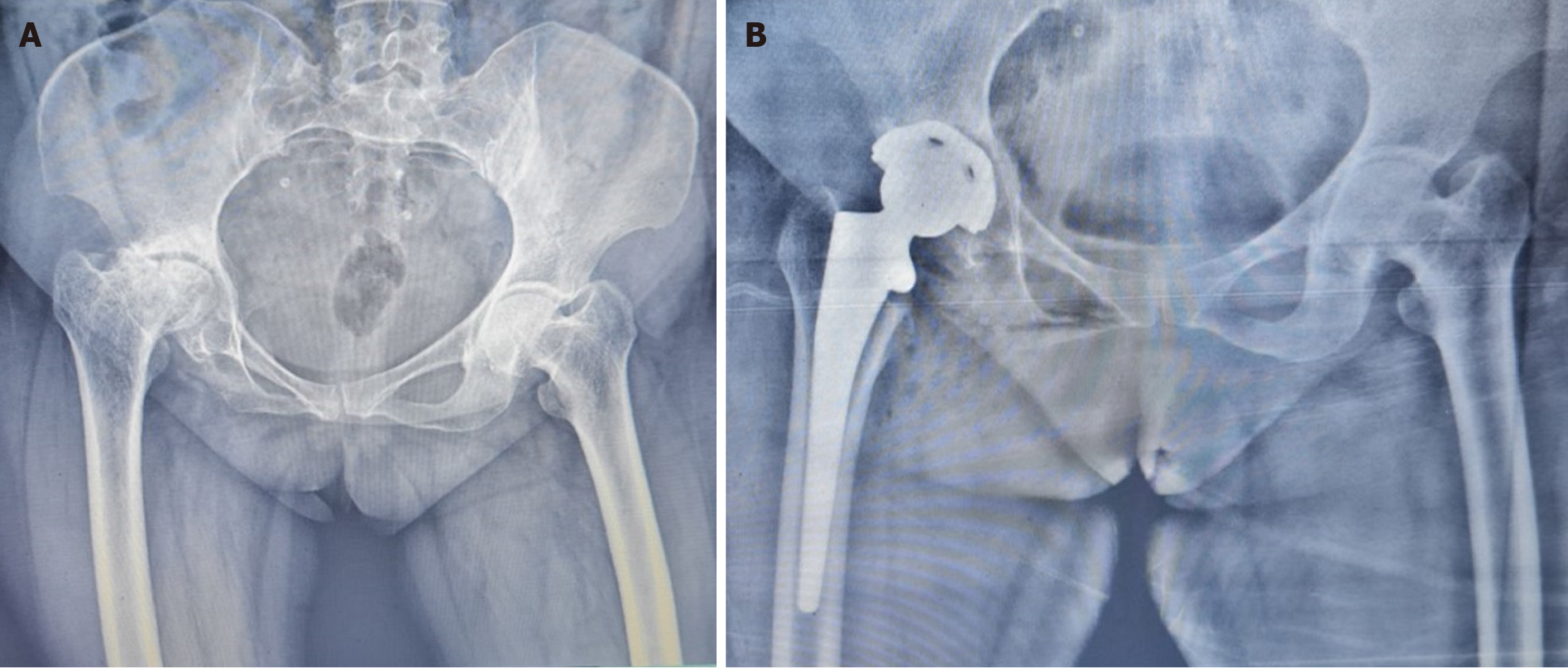
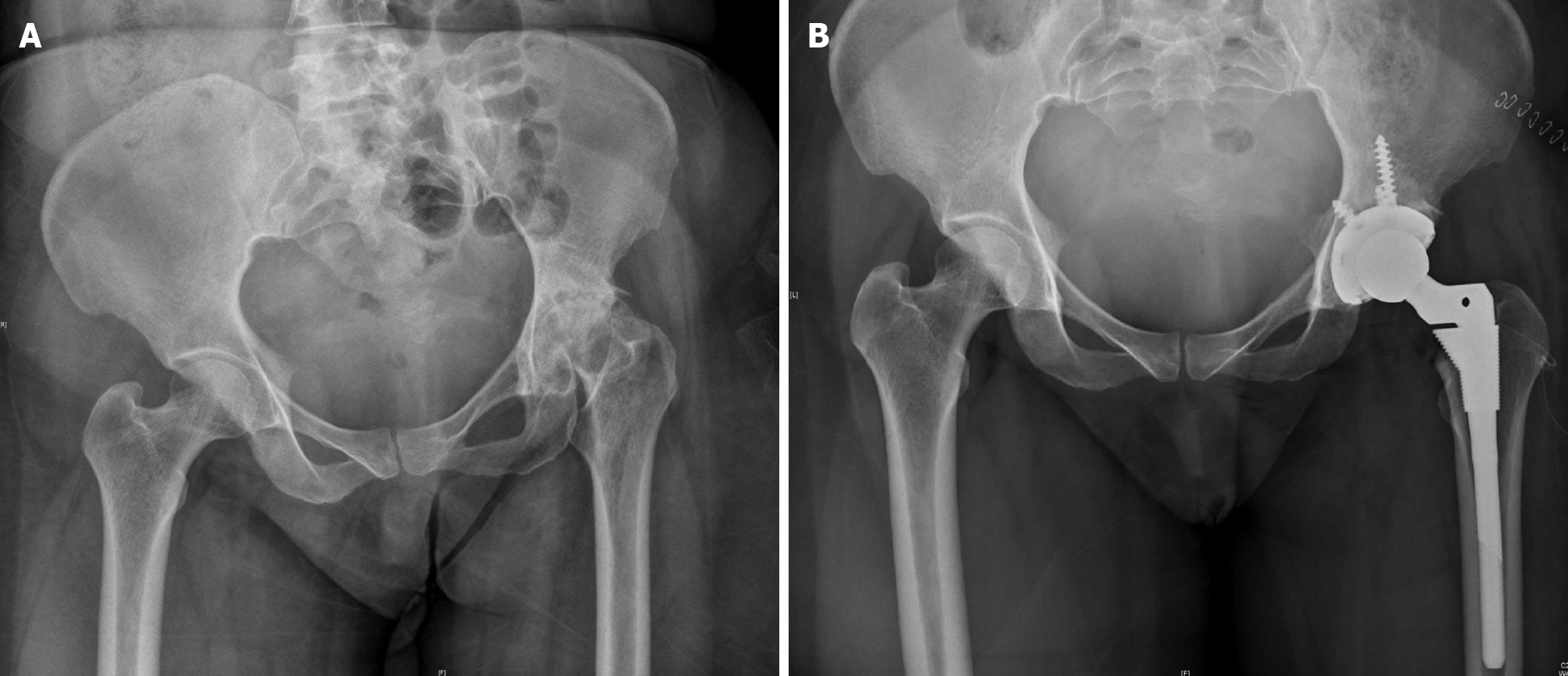
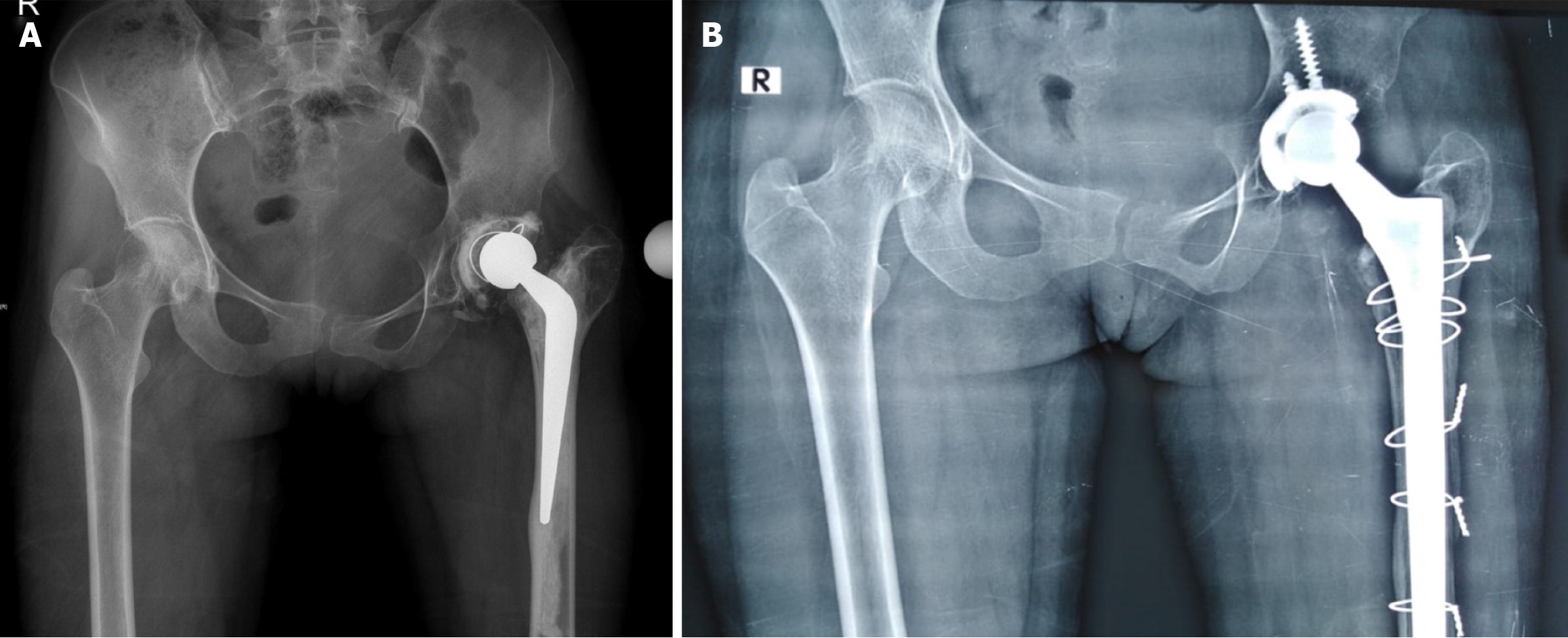
THA for fracture neck of femur in an older individual can provide excellent functional outcomes with proper restoration of the horizontal offset. Recent evidence suggests that incorrect offset restoration could impair function and outcome in these situations. The risk of inaccurate restoration seems to be higher in surgeons without regular experience in hip arthroplasty[11]. THA for a fractured neck of the femur should be done with appropriate pre-operative planning and templating to restore the length and offset (Figure 7).
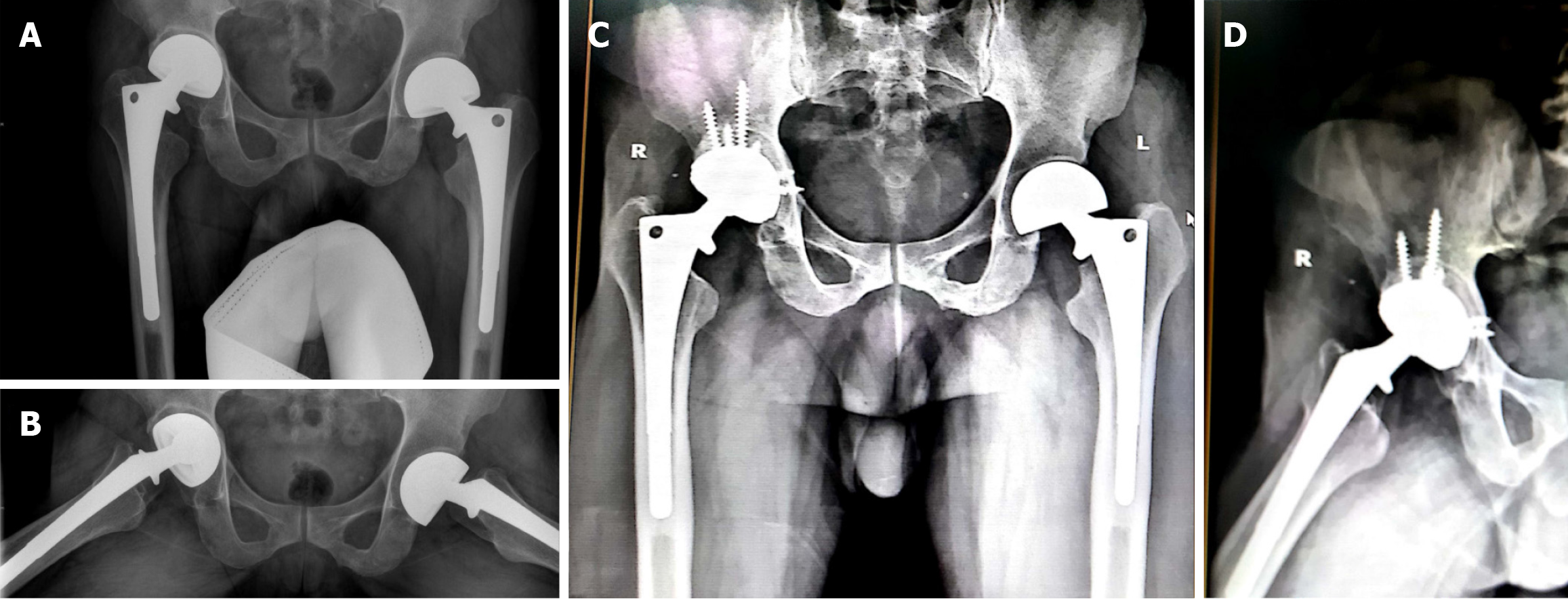
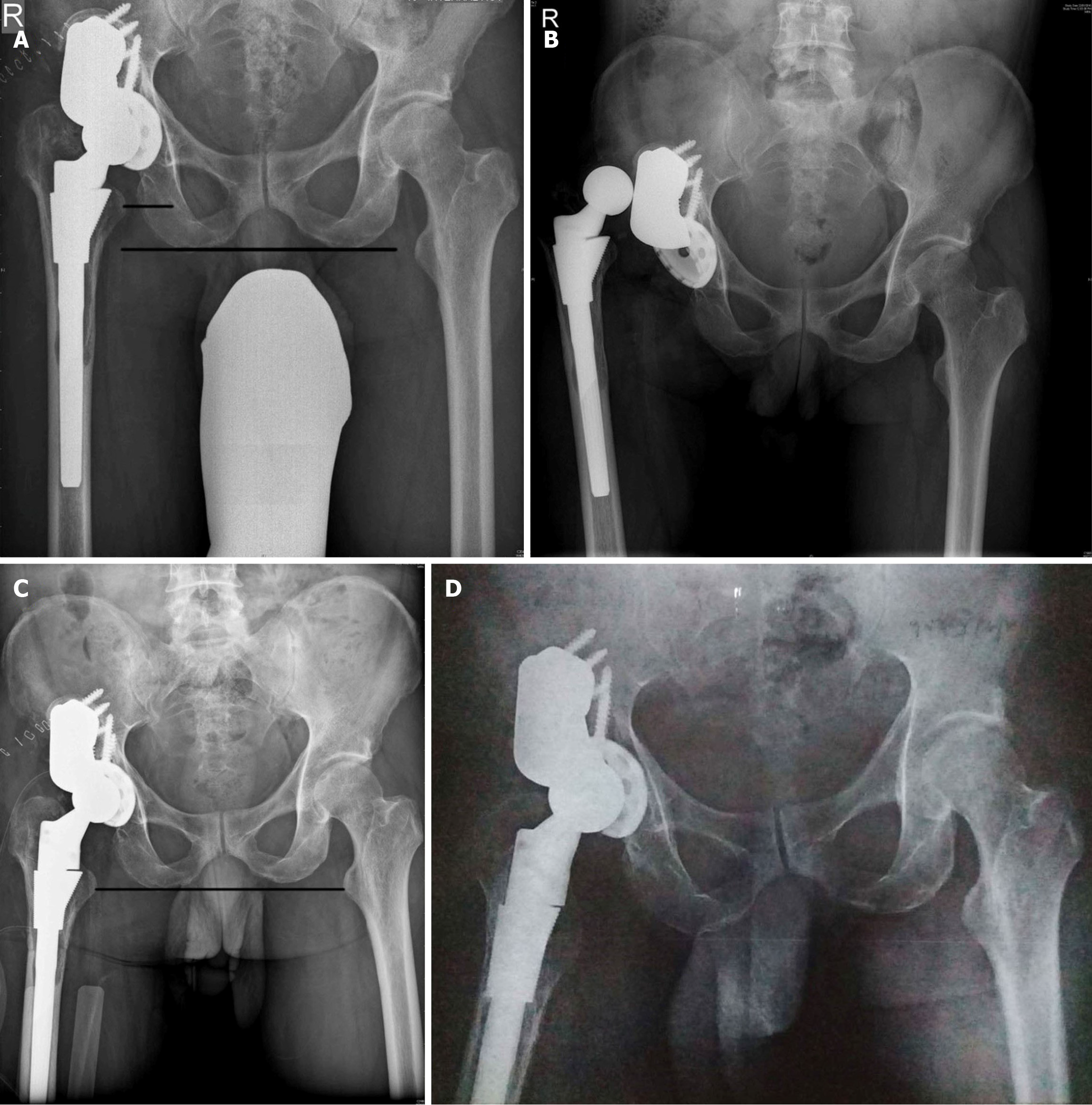
The restoration of horizontal offset is necessary in hips with proximal migration along with acetabular defects requiring reconstruction. Hip COR with the establishment of the horizontal and vertical offset is critical as horizontal offset plays a significant role in abductor function (Figures 8 and 9).
Indication for revision THA could be inadequate restoration of offset with well-fixed femoral and acetabular components. Use of the bio ball adapter to restore the offset in revision THA has been reported with good one-year results[12].
Recent data suggest that establishing the horizontal and vertical offset improves function and longevity and postpones the need for revision. Satisfaction was much lower in individuals with inadequate restoration of offset and length.
Offset restoration with particular attention to horizontal and vertical offset is needed to recreate native hip biomechanics. A minimal increase in horizontal offset up to 5 mm restores hip biomechanics, function with favorable long-term outcomes, while decreased offset can prove detrimental[1]. Inadequate restoration of both horizontal and vertical offset could lead to dislocation, which would require revision to establish normal length and offset (Figure 10). Failure to restore offset would result in a reduced range of motion and functional outcome[13]. Femoral stems are available with a short neck and standard and high offset options. Offset options are essential in offset restoration as seen in various studies[1,3,5,7,14,15]. Using high-offset stems has increased stability and reduced dislocation rates in hip arthroplasty[16]. Modular necks have also been considered for offset adjustment and restoration at THA. Modularity, especially at the neck, should be avoided, and using modular necks for THA offset restoration has shown poor results, especially in obese patients[17].
Restoration of offset should be individual based with appropriate preoperative and intraoperative templating and assessment to achieve normal function and good outcome with longevity. Under correction and overcorrection should be avoided[9,13].
Offset restoration at THA requires careful preoperative and intraoperative templating to avoid under-correction. The trial neck options should be available after preoperative templating. An increase in offset can be avoided with intraoperative templating and trial reduction before final implantation.
I acknowledge Dr Neil Sheth, Professor, Chief of Orthopedic Surgery–Pennsylvania Hospital, University of Pennsylvania, United States for inputs with editing the manuscript.
| 1. | Luca DiGiovanni P, Gasparutto X, Armand S, Hannouche D. The modern state of femoral, acetabular, and global offsets in total hip arthroplasty: a narrative review. EFORT Open Rev. 2023;8:117-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 2. | Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131-141. [PubMed] |
| 3. | Hu X, Zheng N, Chen Y, Dai K, Dimitriou D, Li H, Tsai TY. Optimizing the Femoral Offset for Restoring Physiological Hip Muscle Function in Patients With Total Hip Arthroplasty. Front Bioeng Biotechnol. 2021;9:645019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | De Fine M, Romagnoli M, Toscano A, Bondi A, Nanni M, Zaffagnini S. Is there a role for femoral offset restoration during total hip arthroplasty? A systematic review. Orthop Traumatol Surg Res. 2017;103:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | de Waard S, Verboom T, Bech NH, Sierevelt IN, Kerkhoffs GM, Haverkamp D. Femoroacetabular offset restoration in total hip arthroplasty; Digital templating a short stem vs a conventional stem. World J Orthop. 2022;13:139-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Wong JRY, Gibson M, Aquilina J, Parmar D, Subramanian P, Jaiswal P. Pre-Operative Digital Templating Aids Restoration of Leg-Length Discrepancy and Femoral Offset in Patients Undergoing Total Hip Arthroplasty for Primary Osteoarthritis. Cureus. 2022;14:e22766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 7. | Cech A, Kase M, Kobayashi H, Pagenstert G, Carrillon Y, O'Loughlin PF, Aït-Si-Selmi T, Bothorel H, Bonnin MP. Pre-operative planning in THA. Part III: do implant size prediction and offset restoration influence functional outcomes after THA? Arch Orthop Trauma Surg. 2020;140:563-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Reinbacher P, Smolle MA, Friesenbichler J, Draschl A, Leithner A, Maurer-Ertl W. Pre-operative templating in THA using a short stem system: precision and accuracy of 2D versus 3D planning method. J Orthop Traumatol. 2022;23:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 9. | Weber M, Grifka J, Renkawitz T. Patient-Specific Restoration of Biomechanics in Total Hip Arthroplasty. Z Orthop Unfall. 2019;157:292-299. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Della Valle AG, Padgett DE, Salvati EA. Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg. 2005;13:455-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 183] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 11. | Shah HN, Barrett AA, Finlay AK, Arora P, Bellino MJ, Bishop JA, Gardner MJ, Miller MD, Huddleston JI 3rd, Maloney WJ, Goodman SB, Amanatullah DF. Arthroplasty for femoral neck fractures is at risk for under restoration of lateral femoral offset. Hip Int. 2024;34:134-143. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Chimeno C, Fernández-Valencia JÁ, Alías A, Serra A, Postnikov Y, Combalia A, Muñoz-Mahamud E. Contribution of the Bioball(TM) head-neck adapter to the restoration of femoral offset in hip revision arthroplasty with retention of a well-fixed cup and stem. Int Orthop. 2023;47:2245-2251. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Weber M, Merle C, Nawabi DH, Dendorfer S, Grifka J, Renkawitz T. Inaccurate offset restoration in total hip arthroplasty results in reduced range of motion. Sci Rep. 2020;10:13208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Saunders P, Shaw D, Sidharthan S, Young SK; Board T. Hip offset and leg-length restoration in revision hip arthroplasty with a monoblock, hydroxyapatite-coated stem. Hip Int. 2023;33:880-888. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Biggi S, Banci L, Tedino R, Capuzzo A, Cattaneo G, Tornago S, Camera A. Restoring global offset and lower limb length with a 3 offset option double-tapered stem. BMC Musculoskelet Disord. 2020;21:646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Vigdorchik JM, Sharma AK, Elbuluk AM, Carroll KM, Mayman DJ, Lieberman JR. High Offset Stems Are Protective of Dislocation in High-Risk Total Hip Arthroplasty. J Arthroplasty. 2021;36:210-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | Solou K, Panagopoulos A, Tatani I, Megas P. Fracture of femoral neck in modular total hip arthroplasty: a systematic review of the literature. Hip Int. 2024;34:409-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |