Published online Feb 18, 2024. doi: 10.5312/wjo.v15.i2.156
Peer-review started: October 4, 2023
First decision: December 12, 2023
Revised: December 20, 2023
Accepted: January 8, 2024
Article in press: January 8, 2024
Published online: February 18, 2024
Processing time: 125 Days and 18.3 Hours
The minimal clinically important difference (MCID) is defined as the smallest meaningful change in a health domain that a patient would identify as important. Thus, an improvement that exceeds the MCID can be used to define a successful treatment for the individual patient.
To quantify the rate of clinical improvement following anatomical total shoulder arthroplasty for glenohumeral osteoarthritis.
Patients were treated with the Global Unite total shoulder platform arthroplasty between March 2017 and February 2019 at Herlev and Gentofte Hospital, Denmark. The patients were evaluated preoperatively and 3 months, 6 months, 12 months, and 24 months postoperatively using the Western Ontario Osteoarthritis of the Shoulder index (WOOS), Oxford Shoulder Score (OSS) and Constant-Murley Score (CMS). The rate of clinically relevant improvement was defined as the proportion of patients who had an improvement 24 months postoperatively that exceeded the MCID. Based on previous literature, MCID for WOOS, OSS, and CMS were defined as 12.3, 4.3, and 12.8 respectively.
Forty-nine patients with a Global Unite total shoulder platform arthroplasty were included for the final analysis. Mean age at the time of surgery was 66 years (range 49.0-79.0, SD: 8.3) and 65% were women. One patient was revised within the two years follow-up. The mean improvement from the preoperative assess
Based on three shoulder-specific outcome measures we find that approximately 90% of patients has a clinically relevant improvement. This is a clear message when informing patients about their prognosis.
Core Tip: In this study, we present a new approach for analyzing and interpreting improvement in patient-reported outcome measures (PROM) scores by linking the improvement in PROM scores to the minimal clinical difference for each patient. We found that approximately 90% of patients treated with an anatomical total shoulder arthroplasty for glenohumeral osteoarthritis had a clinically relevant improvement two years postoperatively.
- Citation: Nyring MRK, Olsen BS, Amundsen A, Rasmussen JV. High rate of clinically relevant improvement following anatomical total shoulder arthroplasty for glenohumeral osteoarthritis. World J Orthop 2024; 15(2): 156-162
- URL: https://www.wjgnet.com/2218-5836/full/v15/i2/156.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i2.156
The anatomical total shoulder arthroplasty is the most common type of arthroplasty for glenohumeral osteoarthritis in Denmark[1,2] and it has long been known that the anatomical total shoulder arthroplasty yields pain relief and improved shoulder function in the treatment of glenohumeral osteoarthritis[3]. In this study, a platform shoulder arthroplasty system is used. The platform system is characterized by the ability of converting an anatomical arthroplasty to a reverse shoulder arthroplasty with retention of the stem. A systematic review[4] reported statistically significant lower compli
Improvements after shoulder arthroplasty are often reported as mean improvement for the entire population. In large populations, even small mean improvements can lead to a statistically significant improvement. The question is whether these statistically significant improvements are also clinically relevant for the patients. To assess this, the minimal clinically important difference (MCID) can be included in the analyses. MCID is a measurement tool in the interpretation of changes in patient-reported outcome measures (PROM) scores and it is defined as the smallest meaningful change in a health domain that a patient would identify as important[5]. An improvement exceeding MCID is therefore regarded as clinically relevant. The MCID can also provide an important insight into how the patients are doing on an individual level. By focusing on the improvements in PROM scores from preoperatively to postoperatively for each individual patient, we can get a precise estimate of how many patients who achieve a clinically relevant improvement. This gives a better indication of how successful the surgery is at patient level.
The primary aim was to determine the proportion of patients achieving a clinically important improvement after treatment with an anatomical total shoulder platform arthroplasty for osteoarthritis. Our hypothesis was that the anatomical total shoulder arthroplasty with a common platform system would lead to significant improvement for a high proportion of patients.
Between March 2017 and February 2019 all patients referred to Herlev and Gentofte University Hospital with glenohumeral osteoarthritis indicating an anatomical total shoulder arthroplasty were evaluated and offered participation. The following inclusion and exclusion criteria were applied before offering participation:
(1) Primary glenohumeral osteoarthritis independent of previous joint preserving surgery; (2) Osteoarthritis on plain radiographs with standard anterior-posterior and lateral projections; (3) Insufficient effect of non-surgical treatment with symptoms severe enough to justify shoulder arthroplasty; and (4) American Society of Anesthesiology (ASA) scores 1-3, physically fit for surgery and rehabilitation.
(1) Below 18 years of age; (2) Cognitive or linguistic impairment; (3) Rotator cuff insufficiency defined as rotator cuff lesions or grade 2 fat infiltrations on magnetic resonance imaging according to the Goutallier classification[6,7] verified with impaired functional strength and perioperative findings; (4) Insufficient preoperative glenoid bone-stock or large (> 1 cm) humeral bone cysts on computed tomography (CT) verified with perioperative findings; and (5) ASA scores 4-5.
The included patients were treated with the Global Unite Anatomical Shoulder Arthroplasty System (DePuy Synthes, Raynham, Massachusetts, United States of America). Operations were performed or supervised by one of five experienced shoulder surgeons. All procedures were performed with the patient under general anesthesia in beach chair position and with the standard deltopectoral approach and subscapularis tenodesis. The literature on rehabilitation after shoulder arthroplasty surgery is sparse. At our institution, a sling was used for the first two weeks. After two weeks non-weight bearing training was allowed since we want the patients start movements early. However, we focus on protecting the subscapularis, why weight bearing training is not allowed before six weeks. All patients were supervised by a physiotherapist once a week for a minimum of three months. The patients were asked to complete the Western Ontario Osteoarthritis of the Shoulder score (WOOS), the Oxford Shoulder Score (OSS) and the Constant-Murley Score (CMS) preoperatively and subsequently at three months, six months, one year and two years postoperatively. The rate of clinically relevant improvement was defined as the proportion of patients who had an improvement between the preoperative measurement and the final follow-up measurement at two years that exceeded the MCID.
The Western Ontario Osteoarthritis of the Shoulder index is a disease-specific patient-reported outcome score[8]. There are 19 questions divided into four domains: Physical symptoms, sports and work, lifestyle, and emotions. Each question is answered on a visual analogue scale ranging from 0 to 100. The overall score ranges from 0 to 1900, with 1900 being the worst. For ease of interpretation, we converted the total score to a percentage of the maximum score with 100 being the best. We used the Danish version of WOOS which was translated according to international guidelines[9] and validated using classical test theory in a cohort of patients treated with shoulder arthroplasty for osteoarthritis[10]. MCID is reported to be 12.3 points for WOOS[11] in patients with glenohumeral osteoarthritis treated with an anatomical total shoulder arthroplasty.
The Oxford Shoulder Score is a measurement tool for the assessment of pain and function after elective shoulder surgery[12]. There are 12 questions with each item scored from 0 to 4. The overall score ranges from 0 to 48, with 48 being the best. We use a Danish version of OSS which was translated according to international guidelines and validated using classical test theory[13]. MCID is reported to be 4.3 points for OSS[11] in patients with glenohumeral osteoarthritis treated with an anatomical total shoulder arthroplasty.
The Constant-Murley Score is a combined subjective and objective assessment tool. The score has four sub-scale scores: Pain (15 points), activities of daily living (20 points), range of motion (40 points), and strength (25 points). The total score ranges from 0 to 100, with 100 being the best. We used a Danish version[14] of the modified score described by Constant et al[15]. MCID is reported to be 12.8 points for CMS in patients with glenohumeral osteoarthritis or rheumatoid arthritis treated with an anatomical total shoulder arthroplasty[16].
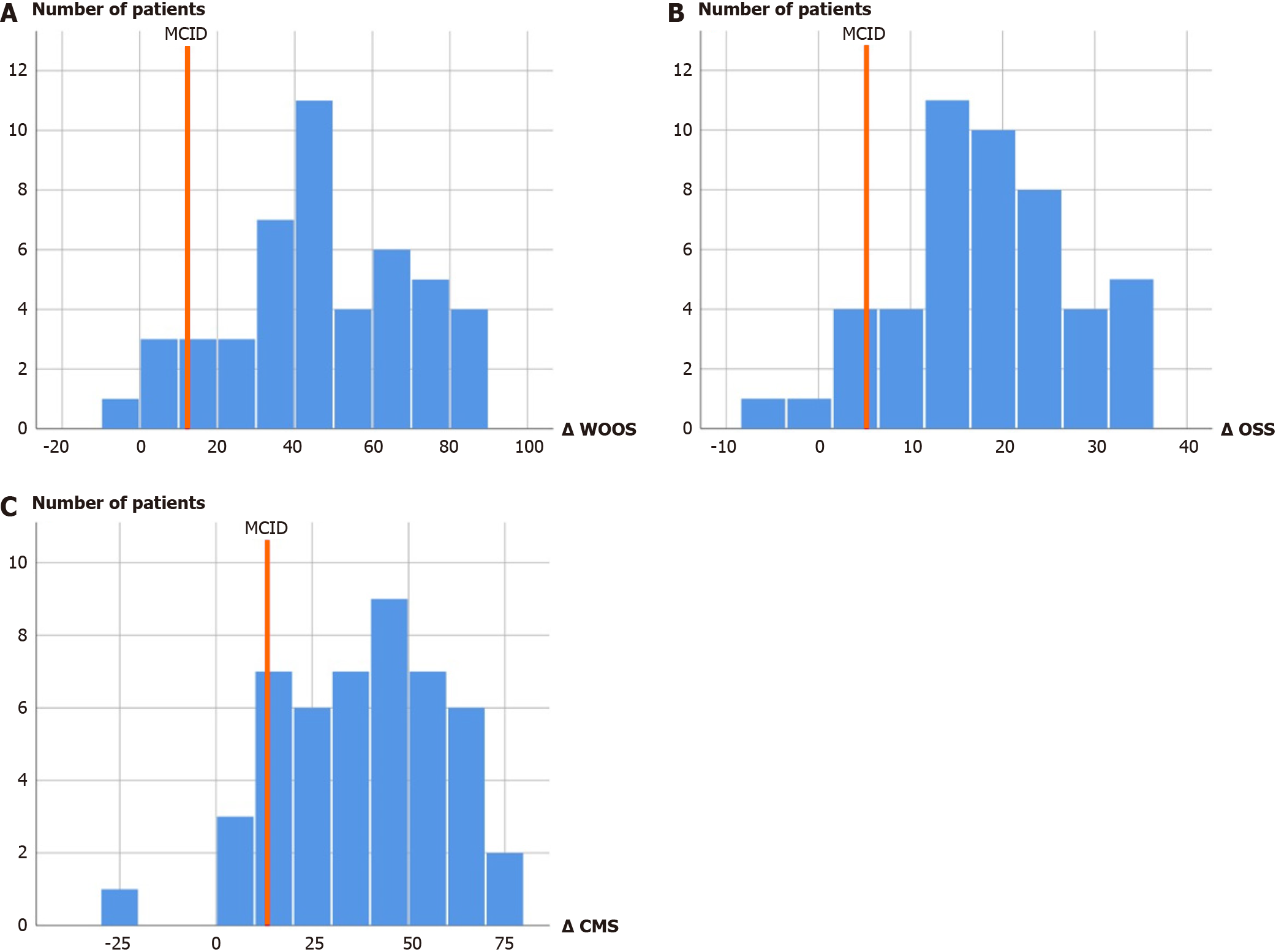
SPSS (IBM Corp, Armonk, NY, United States) was used for the statistical analysis. The level of statistical significance was set at P < 0.05 and P value were 2-tailed. The differences between preoperative and postoperative data are normally distributed (Figure 1). Therefore, we used the paired sample t-test to test for differences within the same groups.
Fifty-five patients with a Global Unite Anatomical Shoulder Arthroplasty were included. Two patients died and four patients did not respond to the invitation for the two-year follow-up, which left 49 patients for the final analysis. Mean age at the time of surgery was 66 years (range: 49-79, SD: 8.3) and 65% were women. One patient was revised within the two years follow-up. This patient was revised 18 months postoperatively because of periprosthetic joint infection with four out of five tissue samples positive for Cutibacteirum Acnes. The follow up results two years after the primary surgery for this patient were 23 for WOOS, 17 for OSS and 25 for CMS and are included in the overall analysis. None of the six patients who were lost to follow-up was revised.
Forty-one patients (87%) had an improvement in WOOS that exceeded the MCID, five patients improved less than the MCID, and one patient had an outcome at two years that was worse than the preoperative score. Forty-five patients (94%) had an improvement in OSS that exceeded the MCID, one patient improved less than the MCID and two patients had an outcome at two years that was worse than the preoperative score. Forty-two patients (88%) had an improvement in CMS that exceeded the MCID, five patients improved less than the MCID, and one patient had an outcome at two years that was worse than the preoperative score. For all three outcome measures, the majority of patients improved much more than the MCID (Figure 1). The patient in need of revision surgery had scores below the MCID in all three outcome measures. However, it was a different patient reporting a two-year outcome worse than the preoperative score.
The mean WOOS, OSS, and CMS were 82.1 (range 22.2 to 100.0), 40.7 (range 15.0 to 48.0) and 66.4 (range 19.0 to 98.0) at two years. The scores improved continuously during the follow-up period (Table 1). The mean improvement from the preoperative assessment to the two-year follow-up was 46.1 points [95% confidence interval (95%CI): 39.7-53.3, P < 0.005] for WOOS, 18.2 points (95%CI: 15.5-21.0, P < 0.005) for OSS and 37.8 points (95%CI: 31.5-44.0, P < 0.005) for CMS. For all three outcome measures, the mean improvement exceeded the associated MCID.
| Preoperative | 3 months | 6 months | 1 yr | 2 yr | |
| WOOS | 35.6 (5.5-74.1) | 73.8 (48.6-96.8) | 76.8 (22.7-98.6) | 81.4 (34.9-99.7) | 83.9 (22.2-100.0) |
| OSS | 22.4 (5.0-38.0) | 36.6 (19.0-47.0) | 38.3 (14.0-48.0) | 40.0 (17.0-48.0) | 40.7 (15.0-48.0) |
| CMS | 28.5 (7.0-71.0) | 48.1 (20.0-87.0) | 53.7 (27.0-81.0) | 61.0 (25.0-95.0) | 66.4 (19.0-98.0) |
In a prospective cohort of patients with glenohumeral osteoarthritis treated with an anatomical total shoulder arthroplasty, we found the proportion of patients who had a clinically important improvement to be 87% for WOOS, 94% for OSS and 88% for CMS.
It might be problematic to make conclusions on the treatment effect based on mean values from PROM scores. The mean values provide an estimate on group level, but do not give any information on individual level. When reporting mean values, it is unknown whether everyone have an improvement that corresponds to the mean value or if most of the patients have a large improvement, while a few patients have a very poor outcome. We have presented a method to remedy this issue by linking the improvement in PROM scores to the MCID for each patient. The MCID is defined as the smallest meaningful change in the PROM score that a patient would identify as important[5]. To give a better estimate of how the individual patient is doing, it would therefore be interesting to report the proportion of patients who achieve this improvement. For three different outcome measures, we found that approximately 90% of the patients achieved an improvement which exceed the MCID. This is equivalent to saying that 90% of patients who are treated with an anatomical total shoulder arthroplasty for osteoarthritis achieve a significant clinical improvement two years after surgery. In our opinion, this is a clear and tangible message which can be used by the surgeon to inform the patients about their prognosis.
According to our knowledge, no previous studies have reported the proportion of patients who exceed the MCID for WOOS or OSS. In a combined group of patients with either an anatomical or a reverse total shoulder arthroplasty, Simovitch et al[16] found that the MCID for CMS was 5.7. Based on this MCID value, the authors concluded that 94.7% of the patients in their cohort achieved a result at two years which exceed the MCID for CMS. In the subgroup of patients who were treated with an anatomical total shoulder arthroplasty, the authors defined the MCID for CMS as 12.8, which is the value we used in this study. Although the authors reported this MCID for CMS, they did not report the proportion of patients with an anatomical total shoulder arthroplasty who exceeded this MCID. Therefore, according to our knowledge, no previous studies have reported the proportion exceeding the MCID for CMS in patients with an anatomical total shoulder arthroplasty. In a study by Ahmed et al[17], they analyzed improvements in the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) based on patients with an anatomical total shoulder arthroplasty used for glenohumeral osteoarthritis. They found 89% of the patients to either have a moderate or substantial clinical benefit, corresponding to an improvement that exceeds the MCID. In addition, a study by Cohn et al[18] based on patients treated with either an anatomical or reverse total shoulder arthroplasty, found that the proportion of patients exceeding MCID two years postoperatively was 90% for ASES and 89 % for CMS. These results are very relatable to this study, contributing to an increase of the external validity.
PROM scores can be difficult for patients to understand and some questions might not be relevant to all patients. In addition, they can be very time consuming. In the study by Cohn et al[18] they tried to remedy these issues of the PROM scores by also using the Single Assessment Numeric Evaluation (SANE) score, which is based on only one question. They compared the correlation between the SANE score and ASES and CMS, and concluded a moderate correlation between the PROM scores and approximately the same percentage of patients exceeding the MCID. However, it is unknown whether this correlation also exists for WOOS and OSS.
The MCID for CMS is based on patients with glenohumeral osteoarthritis or rheumatoid arthritis treated with an anatomical total shoulder arthroplasty. The MCID for WOOS and OSS are based on patients with glenohumeral osteoarthritis treated with an anatomical total shoulder arthroplasty. Thus, the MCID values are, to a great extent, directly attributable to the population in this study. An important limitation in the use of MCID is the dependency on the diagnoses and treatments from which they are determined[19]. Therefore, it is a clear advantage of this study that the MCID values used are based on almost the same cohort of patients as analyzed in this study.
The mean two years WOOS, OSS, and CMS reported in this study are comparable to previous reported postoperative values based on shoulder arthroplasty registries[2,20,21]. This substantiates an extrapolation of the above results to a general population of patients with glenohumeral osteoarthritis treated with an anatomical total shoulder arthroplasty. However, it would be of great interest to validate the proportion of patients achieving a clinically important improvement in a larger multicenter study or a registry study in order to further increase the external validity.
In this study we have presented a new approach for analyzing and interpreting improvement in PROMs after shoulder arthroplasty for osteoarthritis. Previous studies have reported statistically significant and clinically relevant improvement in mean values. However, mean values does necessarily reflect the outcome of a patient, and it can be difficult to use in patient-guidance. We found that approximately 90% of patients who were treated with an anatomical total shoulder arthroplasty with a common platform system for osteoarthritis had a clinically relevant improvement. This is a clear and distinct message that together with information about implant survival can be used to inform patients about their prognosis following surgery.
Anatomical shoulder arthroplasties used for glenohumeral osteoarthritis are often evaluated by mean improvement in patient reported outcome measurements. However, these mean improvements do not talk much about how the individual patient is performing. Therefore, we have aimed to focus on each individual patient’s improvement. These improvements are linked to the minimal clinical important difference, allowing us to determine the proportion of patients achieving a clinically relevant improvement.
To determine the proportion of patients with glenohumeral osteoarthritis and treated with an anatomical shoulder arthroplasty that achieve a clinically relevant improvement. This a new way of analyzing the results which is much more relevant to the individual patient.
To determine the proportion of patients having a clinically relevant improvement two years postoperatively after treatment with an anatomical total shoulder arthroplasty. In future research, we believe that this will be a frequently used analysis method.
We used data from three different patient reported outcome measurements. The improvements from preoperatively to two years postoperatively were connected to the associated minimal clinically important difference (MCID). The proportion of patients exceeding the MCID was defined as the rate of clinically relevant improvement.
The rate of clinically relevant improvement was 87%, 94%, and 88% for the three different patient reported outcome measurements.
Using a new method for analysis of improvements in patient reported outcome measurements, we found that approximately 90% of patients with glenohumeral osteoarthritis and treated with an anatomical shoulder arthroplasty achieved a clinically relevant improvement.
In future research, this method will probably be a frequently used analysis method. The results of this study should be confirmed in larger cohorts.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Danish Orthopedic Society.
Specialty type: Orthopedics
Country/Territory of origin: Denmark
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oommen AT, India S-Editor: Chen YL L-Editor: A P-Editor: Yuan YY
| 1. | International Committee of Medical Journal Editors. International Committee of Medical Journal Editors (ICMJE) authorship guidelines. 2023. [cited 1 October 2023]. Available from: https://www.icmje.org/. |
| 2. | Rasmussen JV, Amundsen A, Sørensen AKB, Klausen TW, Jakobsen J, Jensen SL, Olsen BS. Increased use of total shoulder arthroplasty for osteoarthritis and improved patient-reported outcome in Denmark, 2006-2015: a nationwide cohort study from the Danish Shoulder Arthroplasty Registry. Acta Orthop. 2019;90:489-494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am. 2005;87:1947-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 206] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 4. | Kirsch JM, Khan M, Thornley P, Gichuru M, Freehill MT, Neviaser A, Moravek J, Miller BS, Bedi A. Platform shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2018;27:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Christiansen DH, Frost P, Falla D, Haahr JP, Frich LH, Svendsen SW. Responsiveness and Minimal Clinically Important Change: A Comparison Between 2 Shoulder Outcome Measures. J Orthop Sports Phys Ther. 2015;45:620-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;78-83. [PubMed] |
| 7. | Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1037] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 8. | Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: The Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9:771-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 191] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3427] [Cited by in RCA: 3634] [Article Influence: 113.6] [Reference Citation Analysis (0)] |
| 10. | Rasmussen JV, Jakobsen J, Olsen BS, Brorson S. Translation and validation of the Western Ontario Osteoarthritis of the Shoulder (WOOS) index - the Danish version. Patient Relat Outcome Meas. 2013;4:49-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Nyring MRK, Olsen BS, Amundsen A, Rasmussen JV. Minimal Clinically Important Differences (MCID) for the Western Ontario Osteoarthritis of the Shoulder Index (WOOS) and the Oxford Shoulder Score (OSS). Patient Relat Outcome Meas. 2021;12:299-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78:593-600. [PubMed] |
| 13. | Frich LH, Noergaard PM, Brorson S. Validation of the Danish version of Oxford Shoulder Score. Dan Med Bull. 2011;58:A4335. [PubMed] |
| 14. | Ban I, Troelsen A, Christiansen DH, Svendsen SW, Kristensen MT. Standardised test protocol (Constant Score) for evaluation of functionality in patients with shoulder disorders. Dan Med J. 2013;60:A4608. [PubMed] |
| 15. | Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17:355-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 604] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 16. | Simovitch R, Flurin PH, Wright T, Zuckerman JD, Roche CP. Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. J Shoulder Elbow Surg. 2018;27:298-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 332] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 17. | Ahmed R, Lanham NS, Peterson JR, Jobin CM, Levine WN. Characterization of ASES score pain and functional improvement after anatomic total shoulder arthroplasty: a patient-centered perspective. J Shoulder Elbow Surg. 2022;31:1042-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Cohn MR, Kunze KN, Polce EM, Nemsick M, Garrigues GE, Forsythe B, Nicholson GP, Cole BJ, Verma NN. Establishing clinically significant outcome thresholds for the Single Assessment Numeric Evaluation 2 years following total shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:e137-e146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 19. | Holmgren T, Oberg B, Adolfsson L, Björnsson Hallgren H, Johansson K. Minimal important changes in the Constant-Murley score in patients with subacromial pain. J Shoulder Elbow Surg. 2014;23:1083-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Mowbray J, Van Niekerk M, Frampton C, Hirner M. The outcomes of shoulder arthroplasty in those aged ≥70 years with glenohumeral arthritis: a New Zealand Joint Registry study. J Shoulder Elbow Surg. 2022;31:799-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Flynn L, Patrick MR, Roche C, Zuckerman JD, Flurin PH, Crosby L, Friedman R, Wright TW. Anatomical and reverse shoulder arthroplasty utilizing a single implant system with a platform stem: A prospective observational study with midterm follow-up. Shoulder Elbow. 2020;12:330-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |