Published online Jun 18, 2023. doi: 10.5312/wjo.v14.i6.411
Peer-review started: December 27, 2022
First decision: March 14, 2023
Revised: March 29, 2023
Accepted: May 15, 2023
Article in press: May 15, 2023
Published online: June 18, 2023
Processing time: 173 Days and 14.7 Hours
Life expectancy in patients with Duchenne muscular dystrophy (DMD) has improved due to advances in medical care. DMD patients develop progressive spinal deformity after loss of ambulatory function and onset of wheelchair dependence for mobility. There is limited published data on the effect of spinal deformity correction on long-term functional outcomes, quality of life (QoL), and satisfaction in DMD patients.
To investigate the long-term functional outcomes following spinal deformity correction in DMD patients.
This was a retrospective cohort study from 2000-2022. Data was collected from hospital records and radiographs. At follow-up, patients completed the muscular dystrophy spine questionnaire (MDSQ). Statistical analysis was performed by linear regression analysis and ANOVA to analyse clinical and radiographic factors significantly associated with MDSQ scores.
Forty-three patients were included with mean age 14.4 years at surgery. Spino-pelvic fusion was performed in 41.9% of patients. Mean surgical time was 352.1 min and mean blood loss was 36% of estimated total blood volume. Mean hospital stay was 14.1 d. Postoperative complications occurred in 25.6% of patients. Mean preoperative scoliosis was 58°, pelvic obliquity 16.4°, thoracic kyphosis 55.8°, lumbar lordosis 11.1°, coronal balance 3.8 cm, and sagittal balance + 6.1 cm. Mean surgical correction of scoliosis was 79.2% and of pelvic obliquity was 80.8%. Mean follow-up was 10.9 years (range: 2-22.5). Twenty-four patients had died at follow-up. Sixteen patients completed the MDSQ at mean age 25.4 years (range 15.2-37.3). Two patients were bed-ridden and 7 were on ventilatory support. Mean MDSQ total score was 38.1. All 16 patients were satisfied with the results of spinal surgery and would choose surgery again if offered. Most patients (87.5%) reported no severe back pain at follow-up. Factors significantly associated with functional outcomes (MDSQ total score) included greater duration of post-operative follow-up, age, scoliosis postoperatively, correction of scoliosis, increased lumbar lordosis postoperatively, and greater age at loss of independent ambulation.
Spinal deformity correction in DMD patients leads to positive long-term effects on QoL and high patient satisfaction. These results support spinal deformity correction to improve long-term QoL in DMD patients.
Core Tip: Duchenne muscular dystrophy (DMD) patients develop progressive spinal deformity after loss of independent ambulation. There is limited data on the effect of spinal deformity correction on long-term functional outcomes or satisfaction in DMD patients. This retrospective cohort study investigated long-term functional outcomes following spinal deformity correction in DMD patients, reporting clinical, surgical, radiographic and functional outcomes. All patients were satisfied with surgical outcomes at long-term follow-up. Surgical correction of spinal deformity can have favourable long-term effects on quality of life (QoL) in DMD patients. These results support surgical correction of spinal deformity to improve long-term QoL in DMD patients with spinal deformity.
- Citation: Roberts S, Arshad A, Tsirikos AI. Surgical and long-term functional outcomes of patients with Duchenne muscular dystrophy following spinal deformity correction. World J Orthop 2023; 14(6): 411-426
- URL: https://www.wjgnet.com/2218-5836/full/v14/i6/411.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i6.411
Duchenne muscular dystrophy (DMD) is an inherited X-linked disease. Mutations in the Xp21 region of the X chromosome leads to absence of dystrophin resulting in skeletal, respiratory, and cardiac muscle weakness[1,2]. The natural history of untreated DMD is progressive muscle weakness with loss of independent ambulation by 9-10 years of age, as well as progressive cardiomyopathy and respiratory failure[3]. The mean survival in the absence of ventilatory support is 19.5 years[4]. Advances in medical therapy have improved the life expectancy for patients with DMD into their third and fourth decades of life[5]. Patients with DMD develop scoliosis after loss of ambulatory capacity and onset of wheelchair dependence for mobility[6]. The scoliosis is typically a long thoracolumbar C-shaped curve, with at least 85% of DMD patients experiencing a progression of deformity at a mean rate of 2.1o per month[7,8]. Respiratory function, measured by forced vital capacity (FVC), declines after loss of ambulation, and the rate of decline increases with progression of scoliosis[9]. Progressive spinal deformity also results in pelvic obliquity which impairs wheelchair sitting ability[10].
Bracing is ineffective in controlling progression of scoliosis in patients with DMD[10]. Surgical correction of scoliosis is indicated when scoliosis develops; surgical correction of scoliosis aims to correct spinal deformity, pelvic obliquity, and to prevent further curve progression with the aim to improve sitting balance, wheelchair mobility, and quality of life (QoL)[6,10-12]. DMD patients undergoing surgical correction of spinal deformity are at high risk of perioperative morbidity and mortality due to cardiomyopathy, respiratory dysfunction, reactions to anaesthetic agents, soft tissue compromise, osteoporosis, risk of instrumentation failure and prolonged intensive care unit (ICU) admission[6].
There is limited published data on the effect of surgical correction of spinal deformity on long-term functional outcomes, QoL and satisfaction in patients with DMD[13-15]. The aim of this study was to investigate the clinical, surgical and long-term functional results following surgical correction of scoliosis in patients with DMD, and to investigate clinical and radiological factors that predict long-term functional outcomes following surgery.
We retrospectively reviewed prospectively-collected data of 113 consecutive patients with DMD who were seen in a National Spinal Deformity Service (NSDS) between January 2000 and August 2022; forty-three of these patients (38%) who were wheelchair-dependent underwent correction of spinal deformity by posterior instrumented spinal fusion. All patients had an established diagnosis of DMD prior to referral to the NSDS and were receiving treatment. Indications for surgical correction of spinal deformity included progressive spinal deformity associated with deteriorating pain, sitting ability, function, and ability to provide nursing care. All patients had minimum data available including pre-operative clinical and demographic details, comorbidities, operative details including complications, pre- and post-operative radiographic parameters, and minimum post-surgical follow-up of two years. Exclusion criteria were patients diagnosed with a non-DMD myopathy, patients managed non-operatively, and patients without clinical, demographic, or operative details available for minimum follow-up of two years. Functional outcomes were assessed by the Muscular Dystrophy Spine Questionnaire (MDSQ)[16]. Cause of death was recorded for patients deceased at follow-up. This study was approved by the institutional review board and the requirement for a signed informed consent was waived.
All patients were regularly reviewed in multidisciplinary medical clinics at our institution before and after surgery and assessed in dedicated multidisciplinary pre-assessment anaesthetic-led clinics to optimise their co-morbidities and provide preparation for spinal surgery. Preoperative assessments included overnight sleep studies, as well as anaesthetic, cardiology, dietician, gastroenterology, neurology, physiotherapy, and respiratory team reviews. All patients were wheelchair dependent at the time of referral to the NSDS.
All patients underwent correction of spinal deformity with posterior instrumented spinal fusion with use of hybrid (pedicle hooks/screws, sublaminar wires) or all pedicle screw instrumentation with local autograft and supplemental allograft bone. Pelvic fixation was performed with use of bilateral iliac screws. Intraoperative spinal cord monitoring was performed recording cortical/cervical somatosensory evoked potentials, which remained stable in all patients; transcranial motor evoked potentials were not recorded as none of the patients in the cohort were able to ambulate. Surgical technique also included use of arterial and central venous lines, prophylactic IV antibiotics, cell salvage, urinary catheter, and placement of a nasogastric tube.
Patients were transferred to the ICU for postoperative care, including haemodynamic support, non-invasive ventilation (NIV), chest physiotherapy, early mobilisation into their wheelchair, and administration of nasogastric feeds. Patients were transferred to a normal ward when medically stable, and discharged to home when oral nutrition, pain control, pulmonary function and wound healing were stable and well-established.
The radiological parameters of scoliosis were measured on spinal radiographs by two authors using digital software (Vue PACS, Carestream Health, United Kingdom) based on consensus agreement on the anatomical landmarks; the mean of the two values was used in the data set for analyses. The same landmarks were used for measurement of the curves on consecutive radiographs. Spinal radiographs were performed including posteroanterior and lateral sitting scoliosis views, and preoperative supine traction views. The following parameters were measured preoperatively and at follow-up: Scoliosis (Cobb angle), scoliosis flexibility index (%): [(Preoperative Cobb angle – supine traction Cobb angle)/(preoperative Cobb angle) × 100], pelvic obliquity (o), pelvic obliquity flexibility index (%): [(Preoperative pelvic obliquity angle – supine traction pelvic obliquity angle)/(preoperative pelvic obliquity angle) × 100], pre- and post-operative lumbar lordosis (T12-S1, o), pre- and post-operative thoracic kyphosis (T1-T12, o), pre- and postoperative sagittal balance (C7 plumb line, cm), pre- and post-operative coronal balance (C7 plumb line, cm), correction of scoliosis (%): [(Preoperative Cobb angle – postoperative Cobb angle)/(preoperative Cobb angle) × 100)], and correction of pelvic obliquity (%): [(Preoperative pelvic obliquity angle – postoperative pelvic obliquity angle)/(preoperative pelvic obliquity angle) × 100)].
All data were entered into Microsoft Excel and analysed using XLSTAT (Microsoft Corporation, Washington, United States). Clinical, operative, and both preoperative and postoperative radiographic variables for the patient cohort were analysed for their correlation with MDSQ total scores. Stepwise multiple linear regression analysis was performed to determine which individual quantitative variables correlated with MDSQ total scores. Quantitative variables included postoperative follow-up (years), age at final follow-up (years), age at loss of independent ambulation (years), age at surgery (years), duration of surgery (minutes), intraoperative blood loss (mLs), length of ICU stay postoperatively, total length of hospital stay (days) and radiographic measurements. Qualitative variables were analysed for their association with MDSQ total scores using ANOVA; qualitative variables included preoperative gastrostomy for nutrition, preoperative NIV, instrumented fusion to the pelvis, and occurrence of postoperative complications.
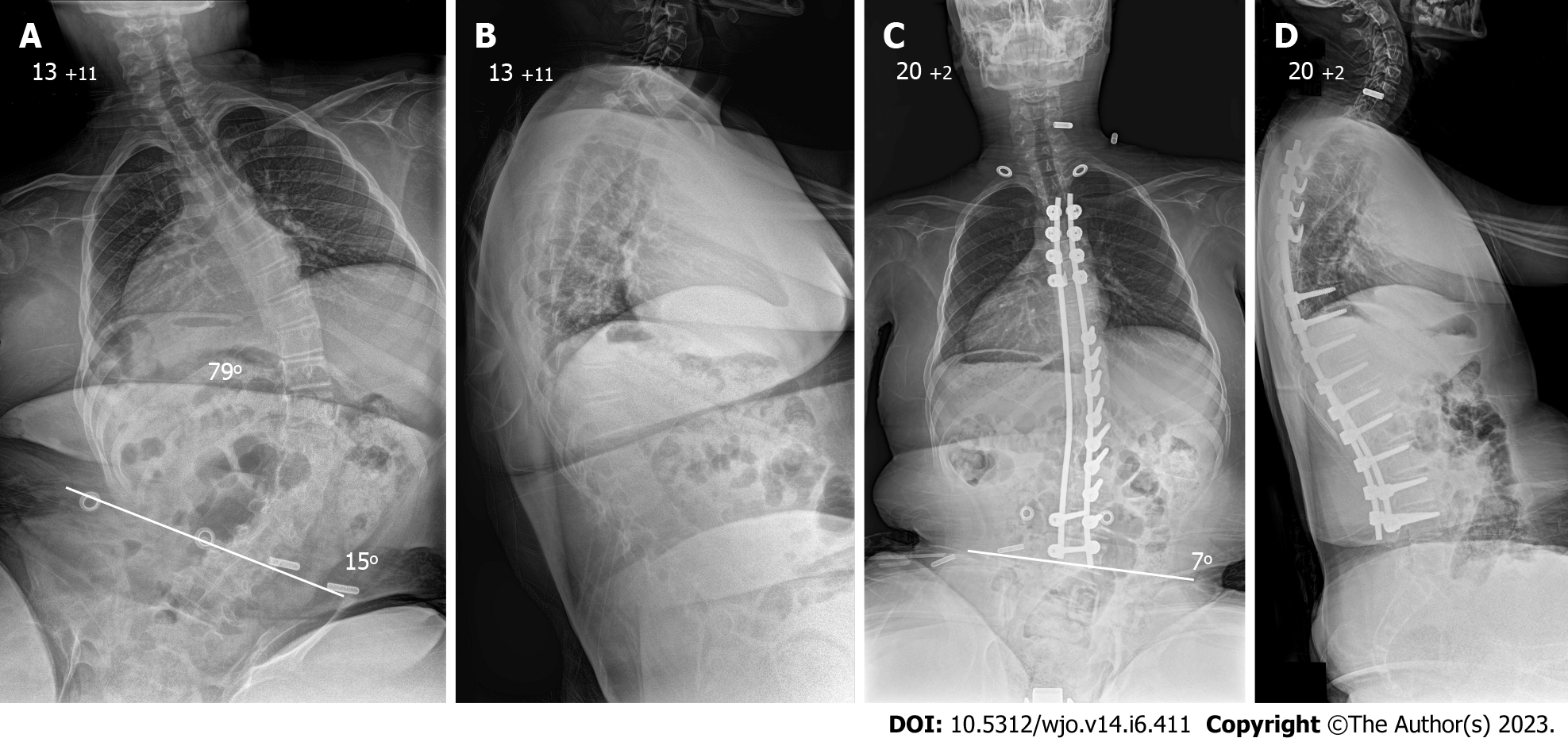
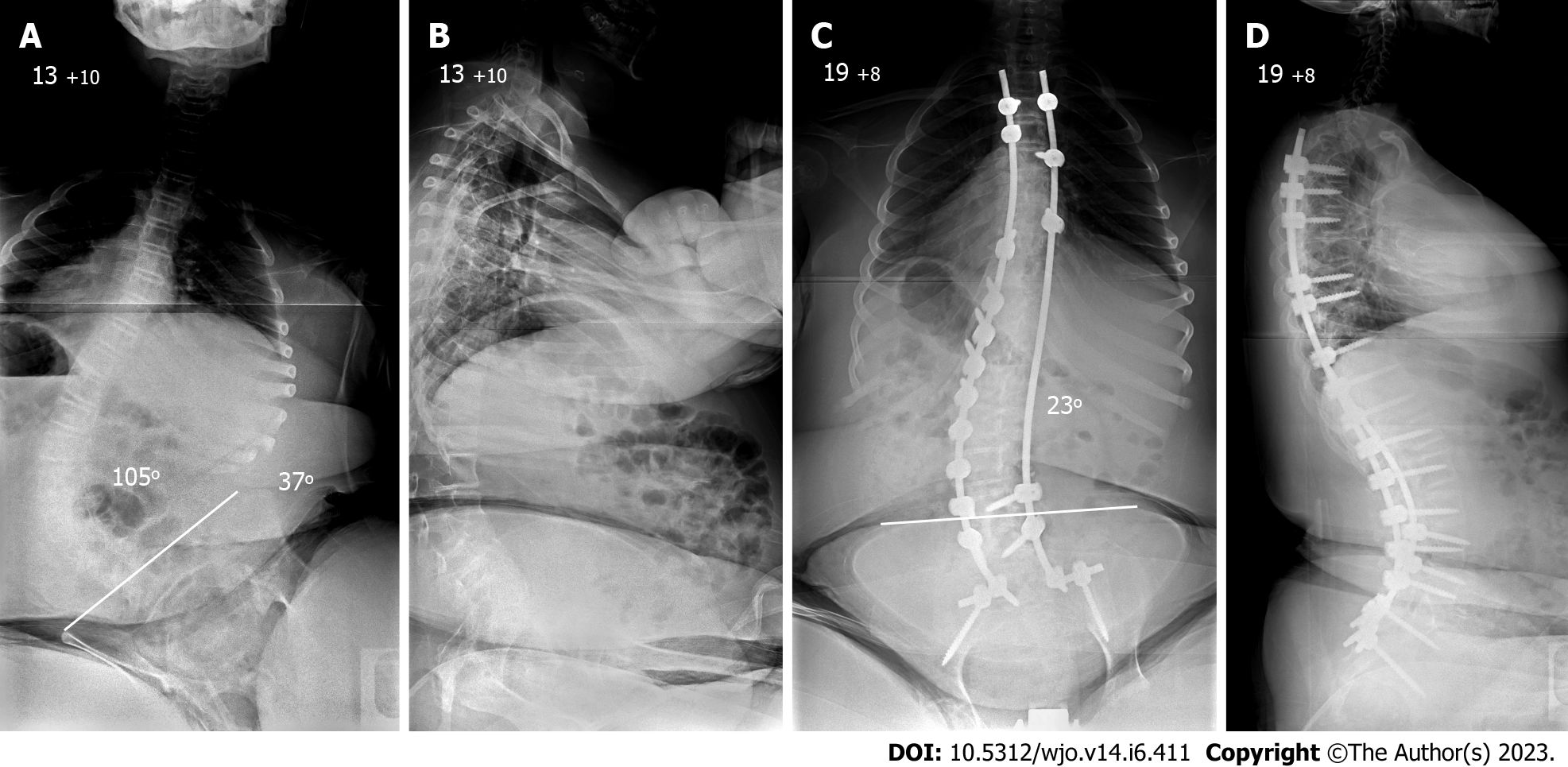
A total of 43 patients with DMD underwent posterior correction of scoliosis with use of instrumentation and bone graft. The mean age at surgery was 14.4 years (SD: ± 1.6; range: 10.8-18.2). The clinical, operative, and pre- and post-operative radiographic details of the patient cohort are shown in Table 1. Four patients (9.3%) required gastrostomy placement for nutrition preoperatively, five patients (11.6%) required NIV preoperatively, and five patients had moderate left ventricular systolic dysfunction. The distal extent of spinal fusion was L4 in four patients (9.3%, Figure 1), L5 in 21 patients (48.8%), and the pelvis in 18 patients (41.9%, Figure 2).
| Parameter (units) | Patient cohort |
| Number of patients (n) | 43 |
| Clinical/operative | |
| Age at surgery (yr) | 14.4 (± 1.6; 10.8-18.2) |
| Spinal deformity, n (%) | |
| Scoliosis | 33 (76.7) |
| Kyphoscoliosis | 10 (23.3) |
| Single thoracolumbar curve | 40 (93) |
| Double thoracic and lumbar curve | 3 (7) |
| Gastrostomy for nutrition pre-operatively, n (%) | 4 (9.3) |
| NIV pre-operatively, n (%) | 5 (11.6) |
| Moderate left ventricular systolic dysfunction, n (%) | 2 (4.6) |
| Operative time (minutes) | 352.1 (± 72.7; 150-490) |
| Intraoperative blood loss (%; TBV) | 36 (± 23.5; 12-150) |
| Distal fusion extent, n (%) | |
| L4 | 4 (9.3) |
| L5 | 21 (48.8) |
| Pelvis | 18 (41.9) |
| Length of stay in ICU (days) | 6.5 (± 3.1; 3-17) |
| Length of stay in hospital (days) | 14.1 (± 7.2; 7-30) |
| Postoperative complications, n (%) | 11 (25.6) |
| Early wound infections | 4 (9.3) |
| Removal of instrumentation (pelvic fixation) | 1 (2.3) |
| Hepatotoxicity | 4 (9.3) |
| Pneumonia | 2 (4.6) |
| Preoperative radiographs | |
| Scoliosis (Cobb angle; o) | 57.5 (± 31; 10-120) |
| Scoliosis on traction radiographs (o) | 32 (± 24; 0-92) |
| Scoliosis flexibility index (%) | 52 (± 27.5; 7-100) |
| Pelvic obliquity (o) | 16.3 (± 13.2; 0-46) |
| Pelvic obliquity on traction radiographs (o) | 9.2 (± 9.3; 0-35) |
| Pelvic obliquity flexibility index (%) | 58 (± 31; 0-100) |
| Thoracic kyphosis (T5-T12; o) | 55.8 (± 28.1; 0-98) |
| Lumbar lordosis (T12-S1; o) | 11.1 (± 20.3; 0-79) |
| Coronal balance (C7PL, cm) | 3.8 (± 2.7; 0-12) |
| Sagittal balance (C7PL, cm) | 6.1 (± 6.4; -11.4-1) |
| Postoperative radiographs | |
| Scoliosis (Cobb angle; o) | 15.6 (± 16.4; 0-60) |
| Scoliosis correction (%) | 79.2 (± 18.6; 40-100) |
| Pelvic obliquity (o) | 4.6 (± 6.4; 0-23) |
| Pelvic obliquity correction (%) | 80.8 (± 25; 19-100) |
| Thoracic kyphosis (T5-T12; o) | 33.7 (± 7.3; 20-55) |
| Lumbar lordosis (T12-S1; o) | 35.8 (± 8.7; 20-55) |
| Coronal balance (C7PL, cm) | 0.68 (± 1.1; 0-4.5) |
| Sagittal balance (C7PL, cm) | -0.18 (± 1.6; -4 to 5.4) |
The mean length of stay in ICU and in hospital are shown in Table 1. Patients requiring hospital stay greater than two weeks after surgery had ongoing nutritional or respiratory difficulties, including the establishment of NIV which required patient familiarisation and carer training before discharge. Postoperative complications included early deep wound infection treated by debridement, antibiotics and retention of instrumentation (four patients; 9.3%), removal of prominent pelvic screws and lateral connectors with trimming of the distal end of the rods while the spine was fused (one patient; 2.3%), pneumonia (two patients, 4.6%), and hepatotoxicity related to paracetamol administration (four patients; 9.3%). During the postoperative follow-up period, 24 patients (55.8%) died; the cause of death for these patients is shown in Table 2. The mean time between surgical correction of spinal deformity and death for these patients was 8.9 years (SD: ± 3.8 years; range 3.9-16.1 years). The incidence of surgical correction of scoliosis in patients with DMD has reduced over the two decades of the study period (32 patients underwent surgical correction of scoliosis from 2000-2010; 11 patients underwent surgical correction from 2011-2022).
| Cause of death | Number of patients |
| Respiratory failure | 10 (41.6) |
| Pneumonia | 7 (29.2) |
| Severe left ventricular systolic dysfunction | 6 (25) |
| Tracheostomy bleeding | 1 (4.2) |
Preoperative and postoperative radiographic parameters of spinal deformity for the cohort are shown in Table 1. The mean preoperative scoliosis was 57.5° (SD: ± 31.4°; range: 10°-120°), which was corrected to mean 15.9° postoperatively (SD: ± 16.6°; range: 0°-60°); resulting in mean scoliosis correction of 79.2% (SD: ± 18.7%; range: 40%-100%). The mean preoperative pelvic obliquity was 16.3° (SD: ± 13.2°; range: 0°-46°), which was corrected to mean 4.6° postoperatively (SD: ± 6.4°; range: 0°-23°), resulting in mean pelvic obliquity correction of 80.8% (SD: ± 25.2%; range: 19%-100%).
Thoracic kyphosis improved from mean 55.8° (SD: ± 28.7°; range: 0°-98°) preoperatively to mean 33.3° (SD: ± 7.7°; range: 20°-55°) postoperatively. Lumbar lordosis improved from mean 11.1° (SD: ± 20.7°; range: 0°-79°) preoperatively to mean 35.6° (SD: ± 8.9°; range: 20°-55°) postoperatively. Coronal balance was 3.8 cm (SD: ± 2.7 cm; range: 0-12 cm) preoperatively, improving to mean 0.68 cm (SD: ± 1.1 cm; range: 0-4.5 cm) postoperatively. Sagittal balance was 6.1 cm (SD: ± 6.4 cm; range: -11.4 to 1 cm) preoperatively, improving to mean -0.18 cm (SD: ± 1.6 cm; range -4 to 5.4 cm) postoperatively (Table 1).
Nineteen patients were alive and invited to complete the MDSQ to assess their functional outcome at long-term follow-up; two patients refused, and one patient was unable to report their outcomes. Sixteen patients completed the MDSQ at a mean postoperative follow-up of 10.9 years (SD: ± 4.7; range: 2-22.5 years); their mean age at completion of the MDSQ was 25.4 years (SD: ± 5.4; range: 15.2-37.3 years). Two (12.5%) of these patients were bed-ridden and 7 (43.75%) were on home ventilatory support. The mean MDSQ total score for these 16 patients was 38.1 (SD: ± 25.9; range: 1-100). All 16 patients were satisfied with the results of scoliosis surgery and reported that they would choose surgical correction of scoliosis again if offered. Fourteen patients (87.5%) reported no significant back or hip pain at long-term follow-up (Table 3).
| Item | Question | Item mean score | SD | Range |
| “Last week how difficult was it to…” | ||||
| 1 | Get dressed | 0 | 0 | 0 |
| 2 | Go to the toilet | 0 | 0 | 0 |
| 3 | Lean forward and reach out in front of me | 1.06 | 1.34 | 0-4 |
| 4 | Move myself around in bed | 0.5 | 0.8 | 0-2 |
| 5 | Write (e.g., a short note and sign it) | 1.06 | 1.69 | 0-4 |
| 6 | Do up my zipper | 0 | 0 | 0 |
| 7 | Sit up in bed | 1.93 | 1.52 | 0-4 |
| 8 | Lift my arms to reach | 0.8 | 1.25 | 0-4 |
| 9 | Lift my head when lying down | 0.9 | 1.18 | 0-4 |
| 10 | Transfer or move from one position to other | 0.4 | 0.89 | 0-3 |
| 11 | Use both hands (e.g., put toothpaste on my toothbrush) | 0.8 | 1.16 | 0-4 |
| 12 | Use 1 arm and hand for balance while reaching in front with the other hand | 0.75 | 1.12 | 0-4 |
| 13 | Hold a spoon or fork by myself as part of a meal | 0.8 | 1.47 | 0-4 |
| 14 | Lift a cup/glass to my mouth by myself to drink | 0.68 | 1.25 | 0-4 |
| 15 | Sit comfortably in a good position, in my wheelchair all day | 2.06 | 1.61 | 0-4 |
| 16 | Shift weight or change my hip position in my wheelchair | 0.68 | 1.01 | 0-3 |
| 17 | Use the computer | 2 | 1.46 | 0-4 |
| 18 | Finish brushing my teeth | 0.56 | 1.15 | 0-4 |
| 19 | Change my arm position in my arm rests | 1.18 | 1.51 | 0-4 |
| 20 | Turn to reach for something | 0.5 | 1.09 | 0-4 |
| 21 | Bend forwards to eat | 1 | 1.36 | 0-4 |
| 22 | Sit in my chair all day without breaks | 2 | 1.86 | 0-4 |
| 23 | Sleep comfortably in bed | 2.375 | 1.6 | 0-4 |
| 24 | Sit at the table for meals | 3 | 1.3 | 0-4 |
| 25 | Bend forward to drink from a straw | 1.43 | 1.67 | 1-4 |
| 26 | Keep balance while sitting in my wheelchair | 3 | 1.31 | 0-4 |
| 27 | Look good while sitting in my wheelchair | 3 | 1.46 | 0-4 |
| “Last week, how bad was…” | ||||
| 28 | Pain in my hips or back last week | 3.125 | 1.2 | 0-4 |
| 29 | Me being out of breath last week | 2.43 | 1.8 | 0-4 |
| Total score | 38.1 | 25.9 | 1-100 |
The relationship between clinical and radiographic parameters and the functional outcomes (MDSQ total score) was assessed (Table 4). Greater duration of postoperative follow-up, increased patient age, higher degree of scoliosis postoperatively, lesser correction of scoliosis, and increased lumbar lordosis postoperatively were significantly associated with lower MDSQ total scores. Greater age at loss of independent ambulation was significantly associated with higher MDSQ total scores.
| Clinical/radiological variable | Value/coefficient estimate (95%CI) | P value |
| Clinical/Operative parameters | ||
| Postoperative follow-up (yr) | -0.766 (-1.138, -0.394) | 0.001a |
| Age (yr) | -0.651 (-1.086, -0.216) | 0.006a |
| Age at loss of independent ambulation (yr) | 0.496 (0.127, 0.865) | 0.013a |
| Age at surgery (yr) | -0.146 (-0.519, 0.227) | 0.410 |
| Preoperative gastrostomy (Y/N)1 | -0.036 (-1.072, 1.001) | 0.941 |
| Preoperative NIV use (Y/N)1 | 0.110 (-0.731, 0.951) | 0.777 |
| Duration of surgery (minutes) | -0.030 (-0.603, 0.543) | 0.911 |
| Intraoperative blood loss (%, TBV) | -0.297 (-0.841, 0.247) | 0.257 |
| Instrumented fused to pelvis (Y/N)1 | 0.542 (-0.221, 1.306) | 0.145 |
| Length of ICU stay (days) | 0.123 (-1.010, 1.255) | 0.817 |
| Length of stay in hospital (days) | -0.535 (-1.663, 0.593) | 0.322 |
| Postoperative complications (Y/N)1 | 0.010 (-0.703, 0.723) | 0.975 |
| Preoperative radiographic parameters | ||
| Scoliosis (Cobb angle) (°) | 0.268 (-5.330, 5.867) | 0.907 |
| Scoliosis on traction radiographs (Cobb angle) | -2.771 (-9.706, 4.164) | 0.351 |
| Scoliosis flexibility index (%) | -2.797 (-6.952, 1.359) | 0.144 |
| Pelvic obliquity (°) | -0.531 (-4.784, 3.723) | 0.761 |
| Pelvic obliquity on traction radiographs (°) | 1.036 (-4.511, 6.582) | 0.651 |
| Pelvic obliquity flexibility index (%) | 1.368 (-2.465, 5.200) | 0.401 |
| Lumbar lordosis (T12-S1; °) | 0.346 (-1.880, 2.571) | 0.706 |
| Thoracic kyphosis (T5-T12; °) | 0.153 (-2.283, 2.589) | 0.878 |
| Sagittal balance (C7PL, cm) | 0.533 (-1.041, 2.106) | 0.424 |
| Coronal balance (C7PL, cm) | 0.213 (-1.401, 1.828) | 0.748 |
| Postoperative radiographic parameters | ||
| Scoliosis (Cobb angle) (°) | -3.005 (-4.718, -1.292) | 0.004a |
| Correction of scoliosis (%) | 2.167 (1.053, 3.282) | 0.002a |
| Pelvic obliquity (°) | 0.367 (-0.765, 1.499) | 0.468 |
| Correction of pelvic obliquity (%) | 0.433 (-0.263, 1.129) | 0.185 |
| Lumbar lordosis (T12-S1; °) | -0.642 (-1.184, -0.100) | 0.027a |
| Thoracic kyphosis (T5-T12; °) | 0.043 (-0.345, 0.430) | 0.802 |
| Sagittal balance (C7PL, cm) | -0.190 (-0.768, 0.389) | 0.464 |
| Coronal balance (C7PL, cm) | 0.886 (-0.215, 1.987) | 0.099 |
The demographic details, surgical techniques, radiographic and functional outcomes in our cohort of DMD patients managed by surgical correction of scoliosis are compared with previously published series in Table 5. Our cohort is one of a few published studies reporting both surgical and functional outcomes at long-term follow-up using a validated disease-specific patient-reported outcome measure, the MDSQ. The mean MDSQ total score reported by our cohort at long-term follow-up (completed at mean age 25.4 years) following surgical correction of scoliosis compared favourably with previous published studies, despite greater duration of follow-up (Table 5). The follow-up (mean 10.9 years) for the assessment of functional outcomes in our cohort was the longest among published studies. The complications and hospital stay outcomes in our cohort of patients are compared with previously published series in Table 6. In our cohort of DMD patients, there was a low overall incidence of postoperative complications (25.6%), and no perioperative deaths (Table 6).
| Study | Current | Heller | Sengupta | Marsh | Cervellati | Hahn | Mehta | Modi | Takaso | Debnath | Alexander | Duckworth | Suk | Nedelcu | Scannell | Takaso | Yang | |||
| Year | 2022 | 2001 | 2002 | 2003 | 2004 | 2008 | 2009 | 2010 | 2010 | 2011 | 2013 | 2014 | 2014 | 2016 | 2017 | 2018 | 2020 | |||
| Patients (n) | 43 | 31 | 50 | 30 | 20 | 20 | 36 | 18 | 28 | 22 | 18 | 28 | 26 | 40 | 13 | 47 | 13 | 271 | 99 | |
| Instrumentation (n) | PH/PS/SL or PS | I | L/G or L-rod | L/G or L-rod | C/HL/USS/S | L/CD | PS/G | PS | PS | PS | SL | PS | L/G and/or PS | SL or PS | CD | UR | L | PS | PS | CD |
| Distal instrumented level [n = (if subset)] | L4 (21), L5 (4), P (18) | SP | P (31) | L5 (19) | P | SP | P | L5 (26); P (10) | L5 (7); SP (11) | L5 | P | L5 | NA | L4/5 (14); SP (12) | LL (5); P (40) | SP | P | P | L5 | LL (5); P (94) |
| Age at surgery (yr) | 14.4 | 14.1 | 14 | 11.7 | 14.7 | 13 | 14 | 13.5 | 14.4 | 13 | 12.5 | 11.8 | 14.2 | 14.2 | 14.9 | 12.7 | 13 | 14 | 13.5 | 15.1 |
| Pre-op FVC% | NA | 54.3 | 44 | 58 | 33 | NA | 55 | NA | NA | NA | 57 | 53 | NA | NA | NA | NA | 59 | 48 | NA | NA |
| Post-op FVC% | NA | NA | NA | NA | NA | NA | 54 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| FVC% at final F/U | NA | 52.7 | NA | NA | NA | NA | 47 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Pre-op scoliosis (°) | 57.5 | 48.6 | 48.4 | 19.8 | 61 | 48 | 44 | 71 | 76.4 | 74 | 45.3 | 42.8 | 56.4 | 59 | 65.5 | 30 | 31 | 43 | 70 | 65.8 |
| Scoliosis (initial post-op) (°) | NA | 12.5 | 16.7 | 3.2 | 24.2 | 22 | 10 | 25.5 | 30.1 | 14 | NA | NA | 21.6 | 13 | NA | 2 | 16 | 12 | 15 | NA |
| Correction of scoliosis (%) | 79.2 | 74.3 | 66 | 80 | 60.3 | 54.2 | 77 | 65 | 63.3 | 81 | NA | NA | 61.7 | 78 | NA | 93.3 | NA | NA | 78.6 | 50.6 |
| Scoliosis at final F/U (°) | 15.6 | 12.5 | 22 | 5.2 | NA | 28 | 9 | 28.5 | 31.3 | 17 | 17.7 | 7.3 | NA | NA | 36.2 | 4.2 | 21 | 12 | 17 | 32.5 |
| Scoliosis loss of correction (°) | NA | 0 | 5.2 | 2 | NA | 6 | 1 | 3 | 1.2 | 3 | NA | NA | NA | NA | NA | 2.2 | 5 | 0 | 2 | NA |
| Pre-op pelvic obliquity (°) | 16.3 | 18.2 | 19.8 | 8.9 | 18.1 | 19.8 | 14 | 14.8 | 18.1 | 9 | 14.5 | 11.2 | NA | 21 | 20.7 | 7.7 | 7 | 6 | 15 | 21 |
| Pelvic obliquity (initial post-op) (°) | NA | 3.8 | 7.2 | 2.2 | NA | 10 | 3 | 6.7 | 8.6 | 3 | NA | NA | NA | 3 | NA | 0.6 | 5 | 3 | 5 | NA |
| Correction of pelvic obliquity (%) | 80.8 | 79.1 | 63.6 | 76 | NA | 49.5 | 65 | 54.7 | 52 | 66.7 | NA | NA | NA | 85.7 | NA | 92.2 | 66.7 | 53.8 | ||
| Pelvic obliquity at final F/U (°) | 4.6 | 5.1 | 11.6 | 2.9 | NA | NA | 3 | 9.3 | 8.8 | 6 | 5.6 | 2 | NA | NA | 11.4 | 1.5 | 5 | 2 | 6 | 9.7 |
| Fusion to sacropelvis (%) | 41.9 | 100 | 100 | 0 | 100 | 100 | 100 | 27.8 | 66.7 | 0 | 100 | 0 | NA | 46.2 | 89.9 | 100 | 100 | 100 | 0 | 94.9 |
| Duration of surgery (min) | 352.1 | 363 | 310 | 240 | 212 | 180 | 307 | 332 | 348 | 282 | 260 | 216 | NA | 260 | NA | 170 | 227 | 332 | 270 | NA |
| Blood loss (mL or % TBV) | 36% | 3373 | 4100 | 3300 | 4900 | 1200 | 2642 | 2955 | 2561 | 950 | 3400 | 2000 | NA | 1882 | NA | 2553 | 1327 | 1596 | 910 | NA |
| F/U (yr) | 10.9 | 1.8 | 4.6 | 3.5 | Until discharge | 5 | 5.2 | 1.6 | 1.4 | 3.3 | 4.5 | 2.3 | 1 | 2 | 3.86 | 6.9 | 4 | 4 | 3 | 6.6 |
| MDSQ score at F/U | 38.1 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | 35.1 | NA | NA | NA | NA | NA |
| Study | Current | Heller | Sengupta | Marsh | Cervellati | Hahn | Mehta | Modi | Takaso | Debnath | Alexander | Duckworth | Suk | Nedelcu | Scannell | |||
| Year | 2022 | 2001 | 2002 | 2003 | 2004 | 2008 | 2009 | 2010 | 2010 | 2011 | 2013 | 2014 | 2014 | 2016 | 2017 | |||
| Patients (n) | 43 | 31 | 50 | 30 | 20 | 20 | 36 | 18 | 28 | 22 | 18 | 28 | 26 | 40 | 13 | 47 | 13 | |
| Instrumentation (n) | PH/PS/SL or PS | I | L/G or L-rod | L/G or L-rod | C/HL/USS/S | L/CD | PS/G | PS | PS | PS | SL | PS | L/G and/or PS | SL or PS | CD | UR | L | PS |
| Distal instrumented level (n) | L4 (21), L5 (4), P (18) | SP (31) | P (31) | L5 (19) | P (30) | SP (n = 20) | P (n = 20) | L5 (26), P (10) | L5 (7), SP (11) | L5 (28) | P (22) | L5 (18) | NA | L4/5 (14), SP (12) | LL (5), P (40) | SP (13) | P (47) | P (13) |
| ICU stay (days) (patient, n) | 6.5 | 3 | NA | NA | NA | 2 | 3.2 | 0.4 (n = 10) | 0.45 (n = 4) | NA | 2.3 | 1.8 | NA | 4.5 | NA | NA | 2 | 4 |
| Hospital stay (days) | 14.1 | 21 | 16.7 | 7.7 | 22 | NA | 19 | 17.9 | 19 | NA | 8.5 | 7 | NA | 13 | NA | NA | 7 | 7 |
| Complications (%; n) | 25.6%; WIRI (4), ROPI (1), pn (2), hep (4) | D (5%), pu (24%), instr 10%, WHP (28%), GI (23%), Thr (5%), Bl (5%) | 16%; DIAR (1), RI (4) | 10.5%; DIARI (1); RI (1) | 30%; PE (1), REI (4), CA (1), TR (2), LFT (1), Pn (2), WI (2) | 30%; CA (1), NB (1), SPS (1), Instr (3) | 20%; D (1), PO (1), WHP (1), DIARI (1) | 47%; D (1), Instr (3), Co (7), PI (6) | 48.1%; D (CA; 1), UTI (2), Co (6), HT (3), TIL (1), AT (2), CBP (2), Instr (1) | 17.9%; I (5) | 54.5%; Bl (2), WI (5), PRS (3), Instr (2) | 16.7%; WI (2), Instr (1) | 17.8%; WI (3), An (2) | 38.5%; WI (6), Hep (4), GI (2), Pn (2) | 52.5%; Pu (20), WI (1) | 53.8%; WHP (3), WI (2), Instr (2), | 68%; Instr (12), Inf (2) | 54%; PJK (1), WI (3) |
Surgical correction of spinal deformity in patients with DMD aims to prevent curve deterioration, correct spinal balance and pelvic obliquity in order to permit more comfortable positioning, sitting in wheelchair, day-to-day activities and QoL[10]. There is limited published literature reporting surgical and functional results at long-term follow-up after surgical correction of spinal deformity in patients with DMD. This retrospective cohort study describes validated patient-reported functional outcomes at the longest available follow-up and surgical outcomes following correction of scoliosis in DMD patients.
Posterior instrumented spinal fusion is indicated for treatment of progressive scoliosis in patients with DMD[12,17,18]. Surgical correction of spinal deformity is recommended before respiratory and cardiac function deteriorate to the extent that general anaesthesia and complex major surgery are unsafe and whilst spinal deformity remains flexible[19-21]. Early surgery may lead to potential sitting height loss, but this is not perceived as a problem[22]. Luque instrumentation and sublaminar wiring for spinal stabilisation in patients with DMD resulted in high patient satisfaction[23]. Results of surgical correction with hybrid constructs utilising pedicle-based anchors and/or instrumentation to the pelvis indicated improved radiographic correction of spinal deformity[24]. Subsequent comparison of sublaminar instrumentation, hybrid instrumentation, and pedicle screw constructs demonstrated that pedicle screw constructs provided a marginally better correction and maintained coronal deformity correction better at follow-up[25]. Pedicle screw instrumentation in patients with DMD achieves better correction of both spinal deformity and pelvic obliquity[10,26]. The patients in our cohort were treated by hybrid or all pedicle screw instrumentation. This resulted in a satisfactory correction of scoliosis from 57.5° to 15.6° at final follow-up (mean 79.2% correction), compared to other reported cohorts of DMD patients managed by hybrid and all pedicle screw constructs (Table 5).
The distal extent of spinal instrumentation to correct spinal deformity and pelvic obliquity remains controversial in the published literature. Traditional management principles include fixation to the sacrum or pelvis to correct pelvic obliquity and improve sitting balance[27]. Distal fixation to the lower lumbar spine with Luque instrumentation has been associated with progression of pelvic obliquity postoperatively, whereas no progression occurred after fixation to the pelvis[28]. Distal instrumentation to the lower lumbar spine using pedicle screws may produce satisfactory results when surgery is performed at a younger age and with milder curves without significant pelvic obliquity (< 15°)[27]. Pedicle screw fixation in multiple levels of the thoracic and lumbar spine provides sufficient stability for spinal correction and mild pelvic obliquity correction. In the presence of significant pelvic obliquity, a combination of L5 pedicle screws and iliac screws provides a stable foundation to correct spinal and pelvic deformity[10]. Segmental pedicle screw instrumentation and fusion to lower lumbar spine may be sufficient if the curve apex is at L2 or higher and if the L5 tilt is less than 15°[29]. It is important to balance this, with avoidance of progression of pelvic obliquity and the potential for further surgery in patients with DMD whose cardiopulmonary health will predictably deteriorate[24]. In our cohort of DMD patients treated with hybrid and all pedicle screw constructs, satisfactory correction of pelvic obliquity was achieved from mean 16.4o preoperatively to 4.6o postoperatively (mean correction of 80.8%) (Table 5).
Hybrid constructs have been associated with a high incidence of instrumentation-related complications (21%), pseudarthrosis (10%), junctional and thoracic kyphosis[30-32]. All pedicle screw constructs provide better maintenance of coronal correction, with loss of correction only 1°-3° over follow-up (Table 5). Rigid pedicle screw instrumentation also allows immediate postoperative mobilisation which is critical for patients with DMD to avoid respiratory complications[10]. Pelvic fixation has been associated with a higher complication rate compared to distal fixation to the lower lumbar spine, including increased blood loss and length of hospital stay[27]. A higher incidence of deep wound infections postoperatively has been reported in patients with DMD, but no increased risk of blood loss, compared to other neuromuscular conditions[33].
Risk factors for prolonged postoperative ICU stay for DMD patients after spinal surgery have been reported, including greater preoperative scoliosis angle, greater estimated blood loss during surgery, and cardiopulmonary complications[34]. Preoperative forced expiratory volume < 40% has been associated with development of respiratory complications postoperatively[34]. DMD patients in our cohort had a low incidence of complications (25.6%), similar total hospital stay (mean 14.1 d) but greater ICU stay (mean 6.5 d) after spinal surgery compared to other cohorts in the published literature (Table 6); this may be due to availability and selection of patients for postoperative care in ICU. All patients in our cohort were routinely transferred to ICU for postoperative care, whereas this was reserved for selected patients in previous cohorts.
Respiratory function declines most rapidly in patients with DMD during the accelerated growth spurt in adolescence[35]. FVC in patients with DMD reduces at a rate of 4% per year after loss of ambulation, and an additional 4% decline is associated with each 10° progression of scoliosis[9]. Spinal surgery improves postoperative respiratory muscle strength; respiratory muscle training can reduce perioperative complications and effectively maintain pulmonary function perioperatively[36]. Following surgical correction of spinal deformity, FVC decline improved from 4% per year preoperatively to 1.75% per year postoperatively[37]. Spinal deformity correction is associated with a lesser rate of decrease in FVC, reduced need for NIV, and patients reporting that they can breathe more easily postoperatively[15]. DMD patients with high-risk pulmonary dysfunction (FVC < 30%) and severe scoliosis can undergo spinal surgery with all pedicle screw instrumentation and general anaesthesia after respiratory muscle training. Surgical correction was maintained at follow-up, while patients and parents were highly satisfied and believed scoliosis surgery improved their function, sitting balance and QoL despite high rates for significant complications[38].
Surgical treatment for DMD patients with scoliosis delays the decline in pulmonary function and is correlated with improved survival[13]. The combination of surgical correction of spinal deformity and provision of home nocturnal ventilation has an additive effect on survival for patients with DMD; the presence of severe cardiomyopathy is also a determining factor in life expectancy in patients with DMD[3]. Surgical management of scoliosis in DMD patients has been associated with a significantly lower mortality rate at 6.4 years follow-up, compared to those managed without surgery (8.1% vs 22%)[13].
There is limited evidence in the literature reporting validated patient-reported outcome measures following surgical correction of spinal deformity in patients with DMD. Previous studies have described patients and their carers reporting improved sitting balance, wheelchair mobility, appearance, functional freedom of their arms, nursing care, satisfaction and respiratory function following surgery compared to their preoperative status[39]. The MDSQ is a validated patient-reported questionnaire assessing symptoms and functional abilities important to children with scoliosis and muscular dystrophy[16]. A single study previously reported MDSQ scores in DMD patients with scoliosis treated surgically or nonoperatively at mean 3.8 years follow-up; significantly higher scores were reported by patients after spinal surgery compared to those managed nonoperatively. Better scores were reported by patients managed surgically regarding sitting in wheelchair or chairs, mobility and positioning in wheelchair, appearance, pain, and respiratory symptoms when sitting, compared to patients treated conservatively[15].
This study is the first to describe functional outcomes for DMD patients following surgical correction of scoliosis at long-term follow-up (mean 10.9 years). The MDSQ total score was 38.1, similar to previously reported postoperative scores at follow-up (Table 5), with higher scores for sitting comfortably in wheelchair, sleeping comfortably in bed, pain in my hips and back, and being out of breath (Table 3). Factors significantly associated with lower MDSQ total score, and therefore predictive of worse long-term function, included greater duration of post-operative follow-up, increased patient age, greater residual scoliosis postoperatively, lesser degree of scoliosis correction, and increased lumbar lordosis postoperatively (Table 5). Greater age at loss of independent ambulation was significantly associated with higher MDSQ total scores. Due to the natural history of progressive muscular weakness causing gradual functional decline in patients with DMD, it follows that greater duration of postoperative follow-up and higher age at last assessment are associated with worse function as indicated by the MDSQ. Greater residual scoliosis and lesser scoliosis correction at follow-up suggest a more severe preoperative spinal deformity probably due to a more severe underlying disease and therefore were also associated with worse function assessed by the MDSQ. Conversely, greater age at loss of independent ambulation may indicate a less severe disease course and be related to higher MDSQ total scores (Table 5).
The relationship between increased lumbar lordosis postoperatively and worse functional scores is unclear. Five patterns of sagittal plane spinal deformity have been described in DMD patients[40]; greater number of patients will need to be assessed with clinical, radiological, and functional outcomes to determine optimal restoration of lumbar lordosis and sagittal profile for non-ambulatory DMD patients. Patients in our cohort reported high satisfaction at long-term follow-up after surgery and all replied that they would choose surgical correction of spinal deformity again if offered. These results indicate that surgical correction of spinal deformity can improve QoL in DMD patients and is, therefore, indicated in the presence of a severe/progressive deformity despite an increased risk of complications compared to patients with no underlying neuro-disability.
This study has strengths and limitations. This is a single-centre retrospective cohort review assessing surgical results and validated patient-reported functional outcomes using the MDSQ following surgical correction of spinal deformity in DMD patients at the longest reported postoperative follow-up (mean 10.9 years). This provided a standardised approach for the treatment and management of these patients. Increased number of patients completing MDSQ at long-term follow-up may help to investigate the relationship between sagittal spinal balance and functional scores. Further tests of function have been reported and may help to provide a comprehensive functional assessment in patients with DMD. The manual muscle test is a quantitative muscle test. The modified Rancho scale and Swinyard scale assess mobility and function in neuromuscular patients. However, these tests of function may not be useful in the evaluation of function in patients with advanced DMD and scoliosis[15].
This study reports surgical and validated patient-reported functional outcomes at long-term follow-up after surgical correction of scoliosis in DMD patients. Posterior instrumented spinal fusion is associated with satisfactory correction of spinal deformity and pelvic obliquity which is maintained at follow-up. All patients were satisfied with surgical results at long-term follow-up. Long-term functional outcomes were predicted by patient age, age at loss of ambulation, duration of follow-up, severity of residual scoliosis postoperatively, degree of scoliosis correction and lumbar lordosis. Surgical correction of spinal deformity can have positive long-term effects on QoL and is recommended in DMD patients with spinal deformity.
Life expectancy in patients with Duchenne muscular dystrophy (DMD) has improved due to advances in medical care. DMD patients developed progressive spinal deformity after loss of ambulatory function and onset of wheelchair dependence for mobility. Surgical correction of scoliosis in patients with DMD aims to improve sitting balance, wheelchair mobility and quality of life (QoL). DMD patients undergoing surgical correction of spinal deformity are at high risk of perioperative morbidity and mortality.
There is limited published data on the effect of spinal deformity correction on long-term functional outcomes, QoL, and satisfaction in DMD patients.
The aim of this study was to investigate the clinical, surgical, and long-term functional results following surgical correction of scoliosis in patients with DMD, and to investigate clinical and radiological factors that predict long-term functional outcomes following surgery.
This was a retrospective cohort study, reviewing data from 113 consecutive patients with DMD who were seen in a National Spinal Deformity Service between January 2000 and August 2022. Data were collected from hospital records and radiographs. All patients had minimum data available including pre-operative clinical and demographic details, comorbidities, operative details including complications, pre- and post-operative radiographic parameters, and minimum post-surgical follow-up of two years. Functional outcomes were assessed by the muscular dystrophy spine questionnaire (MDSQ).
Forty-three patients underwent correction of spinal deformity by posterior instrumented fusion, comprising 38% of the whole cohort (43/113 patients); spinopelvic fusion was performed in 41.9% of patients, the mean surgical time was 351 min, mean blood loss was 36% of estimated total blood volume, mean hospital stay was 14.1 d, and postoperative complications occurred in 25.6% of patients. The mean correction of scoliosis was 79.2%, mean correction of pelvic obliquity was 80.8%, and mean post-surgical follow-up was 10.9 years. Mean MDSQ total score at follow-up was 38.1; all 16 patients completing the MDSQ were satisfied with the results of spinal surgery and would choose surgery again if offered, and most patients (87.5%) reported no severe back pain at follow-up. Factors significantly associated with functional outcomes (MDSQ total score) included greater duration of post-operative follow-up, age, scoliosis postoperatively, correction of scoliosis, increased lumbar lordosis postoperatively, and greater age at loss of independent ambulation.
Spinal deformity correction in DMD patients leads to positive long-term effects on QoL, and high patient satisfaction. These results support spinal deformity correction to improve long-term QoL in DMD patients.
Posterior instrumented spinal fusion is indicated for treatment of progressive scoliosis in patients with DMD; surgical correction of spinal deformity is recommended before respiratory and cardiac function deteriorate to the extent that general anaesthesia and complex major surgery are unsafe and whilst spinal deformity remains flexible. DMD patients in our cohort had a low incidence of complications compared to other cohorts in the published literature. Surgical management of scoliosis in DMD patients has been associated with a significantly lower mortality rate at 6.4 years compared to those managed without surgery, and patients and parents were highly satisfied and believed scoliosis surgery improved their function, sitting balance, and QoL. Surgical correction of spinal deformity can improve QoL in DMD patients and is, therefore, indicated in the presence of a severe/progressive deformity despite an increased risk of complications compared to patients with no underlying neurodisability.
The authors would like to thank Mrs. Silvia Garcia Martinez, Data Coordinator for the Spinal Service, who recorded all patients’ information on the British Spine Registry and assisted in data collection.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: British Orthopaedics Association.
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mohey NM, Egypt; Wang G, China S-Editor: Liu XF L-Editor: A P-Editor: Cai YX
| 1. | Hoffman EP, Fischbeck KH, Brown RH, Johnson M, Medori R, Loike JD, Harris JB, Waterston R, Brooke M, Specht L. Characterization of dystrophin in muscle-biopsy specimens from patients with Duchenne's or Becker's muscular dystrophy. N Engl J Med. 1988;318:1363-1368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 677] [Cited by in RCA: 657] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 2. | Alexander WM, Smith M, Freeman BJ, Sutherland LM, Kennedy JD, Cundy PJ. The effect of posterior spinal fusion on respiratory function in Duchenne muscular dystrophy. Eur Spine J. 2013;22:411-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Eagle M, Bourke J, Bullock R, Gibson M, Mehta J, Giddings D, Straub V, Bushby K. Managing Duchenne muscular dystrophy--the additive effect of spinal surgery and home nocturnal ventilation in improving survival. Neuromuscul Disord. 2007;17:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 215] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 4. | Cheuk DK, Wong V, Wraige E, Baxter P, Cole A. Surgery for scoliosis in Duchenne muscular dystrophy. Cochrane Database Syst Rev. 2015;2015:CD005375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Landfeldt E, Thompson R, Sejersen T, McMillan HJ, Kirschner J, Lochmüller H. Life expectancy at birth in Duchenne muscular dystrophy: a systematic review and meta-analysis. Eur J Epidemiol. 2020;35:643-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 6. | Marsh A, Edge G, Lehovsky J. Spinal fusion in patients with Duchenne's muscular dystrophy and a low forced vital capacity. Eur Spine J. 2003;12:507-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Smith AD, Koreska J, Moseley CF. Progression of scoliosis in Duchenne muscular dystrophy. J Bone Joint Surg Am. 1989;71:1066-1074. [PubMed] |
| 8. | Oda T, Shimizu N, Yonenobu K, Ono K, Nabeshima T, Kyoh S. Longitudinal study of spinal deformity in Duchenne muscular dystrophy. J Pediatr Orthop. 1993;13:478-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 56] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Kurz LT, Mubarak SJ, Schultz P, Park SM, Leach J. Correlation of scoliosis and pulmonary function in Duchenne muscular dystrophy. J Pediatr Orthop. 1983;3:347-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 98] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J. 2008;17:255-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Heller KD, Wirtz DC, Siebert CH, Forst R. Spinal stabilization in Duchenne muscular dystrophy: principles of treatment and record of 31 operative treated cases. J Pediatr Orthop B. 2001;10:18-24. [PubMed] |
| 12. | Sussman MD. Advantage of early spinal stabilization and fusion in patients with Duchenne muscular dystrophy. J Pediatr Orthop. 1984;4:532-537. [PubMed] |
| 13. | Yang JH, Kim KS, Lee GH, Kim HS. Comparison of survival analysis between surgical and non-surgical treatments in Duchenne muscular dystrophy scoliosis. Spine J. 2020;20:1840-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Nedelcu T, Georgescu I. Evaluation of the Unit Rod surgical instrumentation in Duchenne scoliosis. A retrospective study. J Med Life. 2016;9:437-443. [PubMed] |
| 15. | Suk KS, Lee BH, Lee HM, Moon SH, Choi YC, Shin DE, Ha JW, Song KM, Kim HS. Functional outcomes in Duchenne muscular dystrophy scoliosis: comparison of the differences between surgical and nonsurgical treatment. J Bone Joint Surg Am. 2014;96:409-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Wright JG, Smith PL, Owen JL, Fehlings D. Assessing functional outcomes of children with muscular dystrophy and scoliosis: the Muscular Dystrophy Spine Questionnaire. J Pediatr Orthop. 2008;28:840-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Granata C, Merlini L, Cervellati S, Ballestrazzi A, Giannini S, Corbascio M, Lari S. Long-term results of spine surgery in Duchenne muscular dystrophy. Neuromuscul Disord. 1996;6:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Miller RG, Chalmers AC, Dao H, Filler-Katz A, Holman D, Bost F. The effect of spine fusion on respiratory function in Duchenne muscular dystrophy. Neurology. 1991;41:38-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Brook PD, Kennedy JD, Stern LM, Sutherland AD, Foster BK. Spinal fusion in Duchenne's muscular dystrophy. J Pediatr Orthop. 1996;16:324-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Galasko CS, Delaney C, Morris P. Spinal stabilisation in Duchenne muscular dystrophy. J Bone Joint Surg Br. 1992;74:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 81] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Miller F, Moseley CF, Koreska J. Spinal fusion in Duchenne muscular dystrophy. Dev Med Child Neurol. 1992;34:775-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Fox HJ, Thomas CH, Thompson AG. Spinal instrumentation for Duchenne's muscular dystrophy: experience of hypotensive anaesthesia to minimise blood loss. J Pediatr Orthop. 1997;17:750-753. [PubMed] |
| 23. | Van Opstal N, Verlinden C, Myncke J, Goemans N, Moens P. The effect of Luque-Galveston fusion on curve, respiratory function and quality of life in Duchenne muscular dystrophy. Acta Orthop Belg. 2011;77:659-665. [PubMed] |
| 24. | Gaine WJ, Lim J, Stephenson W, Galasko CS. Progression of scoliosis after spinal fusion in Duchenne's muscular dystrophy. J Bone Joint Surg Br. 2004;86:550-555. [PubMed] |
| 25. | Arun R, Srinivas S, Mehdian SM. Scoliosis in Duchenne's muscular dystrophy: a changing trend in surgical management : a historical surgical outcome study comparing sublaminar, hybrid and pedicle screw instrumentation systems. Eur Spine J. 2010;19:376-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Debnath UK, Mehdian SM, Webb JK. Spinal Deformity Correction in Duchenne Muscular Dystrophy (DMD): Comparing the Outcome of Two Instrumentation Techniques. Asian Spine J. 2011;5:43-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK. Pelvic or lumbar fixation for the surgical management of scoliosis in duchenne muscular dystrophy. Spine (Phila Pa 1976). 2002;27:2072-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Alman BA, Kim HK. Pelvic obliquity after fusion of the spine in Duchenne muscular dystrophy. J Bone Joint Surg Br. 1999;81:821-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Takaso M, Nakazawa T, Imura T, Fukuda M, Takahashi K, Ohtori S. Segmental Pedicle Screw Instrumentation and Fusion Only to L5 in the Surgical Treatment of Flaccid Neuromuscular Scoliosis. Spine (Phila Pa 1976). 2018;43:331-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (2)] |
| 30. | Yazici M, Asher MA, Hardacker JW. The safety and efficacy of Isola-Galveston instrumentation and arthrodesis in the treatment of neuromuscular spinal deformities. J Bone Joint Surg Am. 2000;82:524-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Gau YL, Lonstein JE, Winter RB, Koop S, Denis F. Luque-Galveston procedure for correction and stabilization of neuromuscular scoliosis and pelvic obliquity: a review of 68 patients. J Spinal Disord. 1991;4:399-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 106] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Neustadt JB, Shufflebarger HL, Cammisa FP. Spinal fusions to the pelvis augmented by Cotrel-Dubousset instrumentation for neuromuscular scoliosis. J Pediatr Orthop. 1992;12:465-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Duckworth AD, Mitchell MJ, Tsirikos AI. Incidence and risk factors for post-operative complications after scoliosis surgery in patients with Duchenne muscular dystrophy : a comparison with other neuromuscular conditions. Bone Joint J. 2014;96-B:943-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Saito W, Inoue G, Shirasawa E, Imura T, Nakazawa T, Miyagi M, Uchida K, Matsuda H, Akazawa T, Takaso M. Risk factors associated with prolonged intensive care unit stay after posterior spinal fusion for Duchenne muscular dystrophy. J Orthop Sci. 2021;26:332-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Miller F, Moseley CF, Koreska J, Levison H. Pulmonary function and scoliosis in Duchenne dystrophy. J Pediatr Orthop. 1988;8:133-137. [PubMed] |
| 36. | Lee TC, Yang LC, Chen HJ. Effect of patient position and hypotensive anesthesia on inferior vena caval pressure. Spine (Phila Pa 1976). 1998;23:941-7; discussion 947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 37. | Velasco MV, Colin AA, Zurakowski D, Darras BT, Shapiro F. Posterior spinal fusion for scoliosis in duchenne muscular dystrophy diminishes the rate of respiratory decline. Spine (Phila Pa 1976). 2007;32:459-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Takaso M, Nakazawa T, Imura T, Okada T, Fukushima K, Ueno M, Takahira N, Takahashi K, Yamazaki M, Ohtori S, Okamoto H, Okutomi T, Okamoto M, Masaki T, Uchinuma E, Sakagami H. Surgical management of severe scoliosis with high risk pulmonary dysfunction in Duchenne muscular dystrophy: patient function, quality of life and satisfaction. Int Orthop. 2010;34:695-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 39. | Modi HN, Suh SW, Hong JY, Cho JW, Park JH, Yang JH. Treatment and complications in flaccid neuromuscular scoliosis (Duchenne muscular dystrophy and spinal muscular atrophy) with posterior-only pedicle screw instrumentation. Eur Spine J. 2010;19:384-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 40. | Shapiro F, Zurakowski D, Bui T, Darras BT. Progression of spinal deformity in wheelchair-dependent patients with Duchenne muscular dystrophy who are not treated with steroids: coronal plane (scoliosis) and sagittal plane (kyphosis, lordosis) deformity. Bone Joint J. 2014;96-B:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |