Published online Aug 18, 2022. doi: 10.5312/wjo.v13.i8.725
Peer-review started: February 23, 2022
First decision: April 13, 2022
Revised: April 23, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 18, 2022
Processing time: 174 Days and 9.2 Hours
In 2016 Centers for Medicare and Medicaid Services proposed bundled payments for hip fractures to improve the quality and decrease costs of care. Patients transferred from other facilities may be imposing a financial risk on the hospitals that accept these patients.
To determine the costs associated with patients that either presented to the emergency department or were transferred from another hospital or skilled nursing facility (SNF) with the diagnosis of a hip fracture requiring operative intervention.
A retrospective single institution review was conducted for all arthroplasty patients from 2010 to 2015. Inclusion criteria included a total or partial hip replacement for a hip fracture. Exclusion criteria included pathologic, periprosthetic, and fracture non-union. Data was collected to compare total observed costs for patients from the emergency department, patients from skilled nursing facilities, and patients from an outside hospital.
A total of 223 patients met the inclusion criteria. 135 (60.54%) of these patients presented primarily to the emergency department, 58 patients (26.01%) were transferred from an outside hospital, and 30 patients (13.43%) were transferred from a SNF. Cost data analysis showed that outside hospital patients demonstrated significantly greater total cost for their hospitalization ($43302) compared to emergency department patients ($28875, P = 0.000) and SNF patients ($28282, P = 0.000).
Patients transferred from an outside hospital incurred greater costs for their hospitalization than patients presenting from an emergency department or SNF. This is a strong argument for risk-adjustment models when bundling payments for the care of hip fracture patients.
Core Tip: Transfers to regional tertiary care centers of critically ill and severely injured patients have been shown to decrease morbidity and mortality. Many of these patients have increased morbidity, length of stay, blood transfusion requirements, and intensive care utilization has been previously documented in transferred patients. To our knowledge, this study is the first to document this phenomenon in patients with femoral neck fractures being treated with arthroplasty. With the nationwide implementation of bundled payments looming, determining the additional risks and costs associated with providing referral services for community and regional hospitals is essential. It is clear from our data that patients transferred from an outside hospital more significantly strain the resources of the receiving tertiary care hospital compared to those patients who present primarily to the emergency department. This is a strong argument for robust risk-adjustment models that potentially even include patient point of origin.
- Citation: Haug EC, Pehlivan H, Macdonell JR, Novicoff W, Browne J, Brown T, Cui Q. Higher cost of arthroplasty for hip fractures in patients transferred from outside hospitals vs primary emergency department presentation. World J Orthop 2022; 13(8): 725-732
- URL: https://www.wjgnet.com/2218-5836/full/v13/i8/725.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i8.725
The Centers for Medicare and Medicaid Services (CMS) began the Comprehensive Care for Joint Replacement (CJR) model in 2016, which aims to hold hospitals accountable for the quality of care delivered from surgery until 90 d after discharge. As has already been reported, episode-of-care payments for elective Total Joint Arthroplasty (TJA) can vary widely and depend on a number of factors. These factors may include the type of procedure, patient comorbidities, discharge disposition, and readmission rates[1,2]. In July 2016, the CMS proposed implementing bundled payments for hip fracture care in order to control costs and improve quality[3]. This has led to concern that patients with multiple comorbidities or surgically complex patients may either be denied necessary care or transferred to other facilities to prevent financial loss at the initial institution. Transfer to a tertiary care facility is necessary in medically complex or critically ill patients and is protected by the Emergency Medical Treatment and Active Labor Act of 1986 (EMTALA). Furthermore, while EMTALA requires hospitals with special capabilities to accept transfers from less specialized facilities, there are no guidelines defining appropriateness of transfers. The implementation of this bundled care model may result in an increase in unnecessary transfers of high-risk patients to tertiary care centers and safety-net hospitals[4,5]. As a result, it is important to understand not only the greater financial risk associated with accepting these patients, but also, the potential for increased morbidity and mortality of patients who are transferred.
Transfers to tertiary care centers, in general, can reduce mortality associated with critically ill and complex patients[6,7]. However, several studies in the orthopaedic literature demonstrate that transfers can be influenced by factors such as insurance status and time of the week with inappropriate transfers rates ranging between 16%-52%[8-13]. Other studies have shown that the transfer of medically and surgically complex patients can negatively impact the receiving hospitals’ outcome measures and mortality rates[4,14]. These hospital quality metrics are available to the public. If these metrics are negatively influenced by inappropriate transfers, this may deter a patient from undergoing an elective procedure at these institutions. However, this has not been demonstrated in the literature as of yet.
The goal of this study was to examine financial and clinical outcomes in hospitalizations for unplanned arthroplasty in hip fractures between patients transferred from outside hospitals, patients presenting to the emergency department, and patients transferred from skilled nursing facilities. This study will help to further characterize the differences in cost and outcomes between these subsets of unplanned arthroplasty patients, which has not been previously documented to the best of our knowledge. This information is useful to physicians, hospital administrators, and payers as it may identify patient groups that utilize increased resources and suffer increased morbidity and/or mortality.
Between 2010 and 2015, demographic, financial, and outcomes data were collected on all arthroplasty patients at our institution, a tertiary care center, as part of an Institutional Review Board-approved patient safety initiative. All patients underwent either total hip arthroplasty or proximal femoral hemiarthroplasty by one of three fellowship trained arthroplasty surgeons at this institution. In all cases, the procedural billing code for the arthroplasty procedure was the primary code submitted to the patient’s insurance or medicare. For the purposes of this study, we included all patients with a diagnosis of basicervical, midcervical, or transcervical femoral neck fractures. Exclusion criteria included pathologic fractures, periprosthetic fractures, and fracture non-unions.
The data collected for the patient safety initiative included age, sex, race, diagnosis, facility of origin, secondary diagnoses, American Society of Anaesthesiologists (ASA) score, length of stay, length of intensive care unit stay, total observed cost, charges, mortality, discharge disposition, and procedure codes. Total observed cost include all costs related to the arthroplasty procedure and subsequent inpatient care of the patient. The patient’s point of origin was determined to be our own institution’s emergency department (ED), outside skilled nursing facility (SNF) or intermediate care facility, and outside hospital (OSH). These locations were verified by reviewing the patient’s individual medical record. Patients who were transferred from an outside hospital or nursing facility to the emergency department were considered as transfers from an outside hospital or SNF, respectively. Patients who were transported to the emergency department from a physician’s office or urgent care were considered emergency department patients. Finally, two patients that were directly admitted from clinic with a diagnosis of femoral neck fracture were not included in the study as they were previously known to and followed by the treating team and could be a potential source of bias in the analysis.
The data was utilized to examine differences in morbidity, mortality, cost, length of stay, and discharge disposition between hip fracture patients based on the individual point of origin prior to presenting to our institution. Each diagnosis, ASA score, Charlson comorbidity index, and surgical procedure performed were confirmed with individual chart review. For categorical variables, a Pearson chi-square analysis was performed.
A total of 223 patients met the inclusion criteria and were included in the study. The number of patients that presented primary to the ED at our institution, typically by EMS or medical transport, was 135 (60.54%). The number of patients that were transferred from an outside hospital to an inpatient unit or to the emergency department was 58 (26.01%). Lastly, the number of patients transferred from a SNF or intermediate care facility was 30 patients (13.43%). Patient cohorts and demographics are presented in Table 1.
| Variable | Emergency department patients (n = 135) | Outside hospital transfer patients (n = 58) | Skilled nursing facility and intermediate care facility patients |
| Average age | 79.53 | 72.25 (P = 0.001) | 83.25 |
| Sex | 80.00% female (P = 0.0000) | 53.45% female | 53.33% female |
| ASA score | |||
| ASA 1 or 2 | 25.92% (P = 0.0007) | 17.24% | 3.33% |
| ASA 3 | 62.22% | 56.90% | 70.00% |
| ASA 4 | 11.85% | 25.86% (P = 0.0007) | 26.67% (P = 0.0007) |
| Average Charlson comorbidity index | 5.17 | 5.51 | 6.07 |
| Percentage hemiarthroplasty (vs THA) | 71.11% | 68.97% | 90.00% |
| Race | 88.14% white | 93.10% white | 90.00% white |
ED patients and SNF patients were significantly older than OSH patients (P = 0.001). ED and SNF patients were not significantly different from each other in age.
There was a larger percentage of ASA 4 patients amongst OSH and SNF patients and significantly lower percentage of ASA 1 and ASA 2 patients compared to the ED patients (P = 0.001). There was no significant difference in average age-adjusted Charlson comorbidity index across all three groups. There was a significantly higher number of female patients (80.00%) who presented to the ED compared to transfers from OSHs (53.45%) and SNFs (53.33%) (P = 0.000). There was a trend toward increased utilization of hemiarthroplasty in SNF patients compared to ED and OSH patients that did not reach statistical significance (P = 0.070). Finally, there was no significant difference in race (white vs non-white) between the three groups (P = 0.583).
Cost data analysis showed that OSH patients demonstrated significantly greater total cost for their hospitalization ($43302) compared to ED patients ($28875, P = 0.000) and SNF patients ($28282, P = 0.000). OSH patients’ costs per hospitalization average 149% and 153% of the cost per hospitalization of ED patients and SNF patients, respectively. There was no significant difference in total cost between ED patient and SNF patients (P = 0.805). This data is summarized in Figure 1. For reference purposes, the average total inpatient cost for the 1540 elective total hip arthroplasties performed at our institution during the same time period as our study population is $22,182. Therefore, the non-elective hip arthroplasty patients’ costs per hospitalization average 193%, 130%, and 127% of the cost per hospitalization of elective total hip patients for OSH, ED, and SNF patients, respectively.
Average LOS was significantly greater in the OSH patients (8.38 d) compared to ED patients (5.89 d, P = 0.003) and SNF patients (6.27 d, P = 0.027). No significant difference was found between ED patients and SNF patients in average LOS (P = 0.599). This data is also summarized in Figure 1.
Of the 135 ED patients, there were 3 in-hospital deaths (2.22%). There were 2 in-hospital deaths among the 58 patients transferred from outside hospitals (3.45%) and 3 in-hospital deaths among the 30 patients transferred from SNFs or intermediate care facilities (10.00%). Owing to the low number of mortalities, these differences did not reach statistical significance.
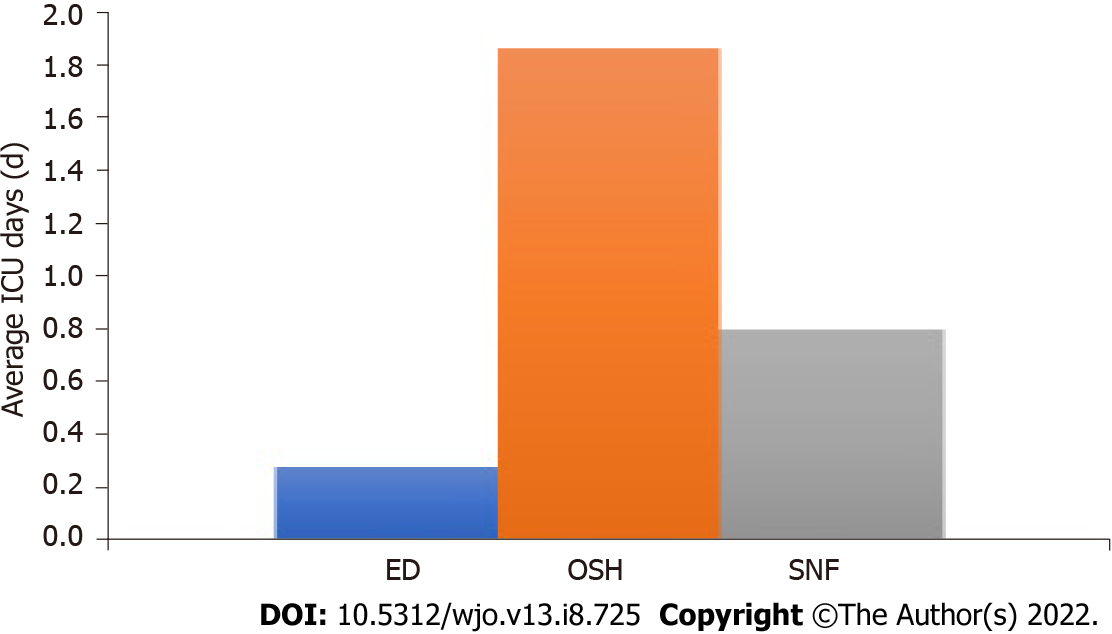
Average intensive care unit (ICU) days per hospitalization was significantly greater in the OSH patients (1.86 d) compared to ED patients (0.28 d, P = 0.001) and SNF patients (0.80 d, P = 0.002). There was no significant difference in ICU days per hospitalization between SNF and ED patients. This data is summarized in Figure 2.
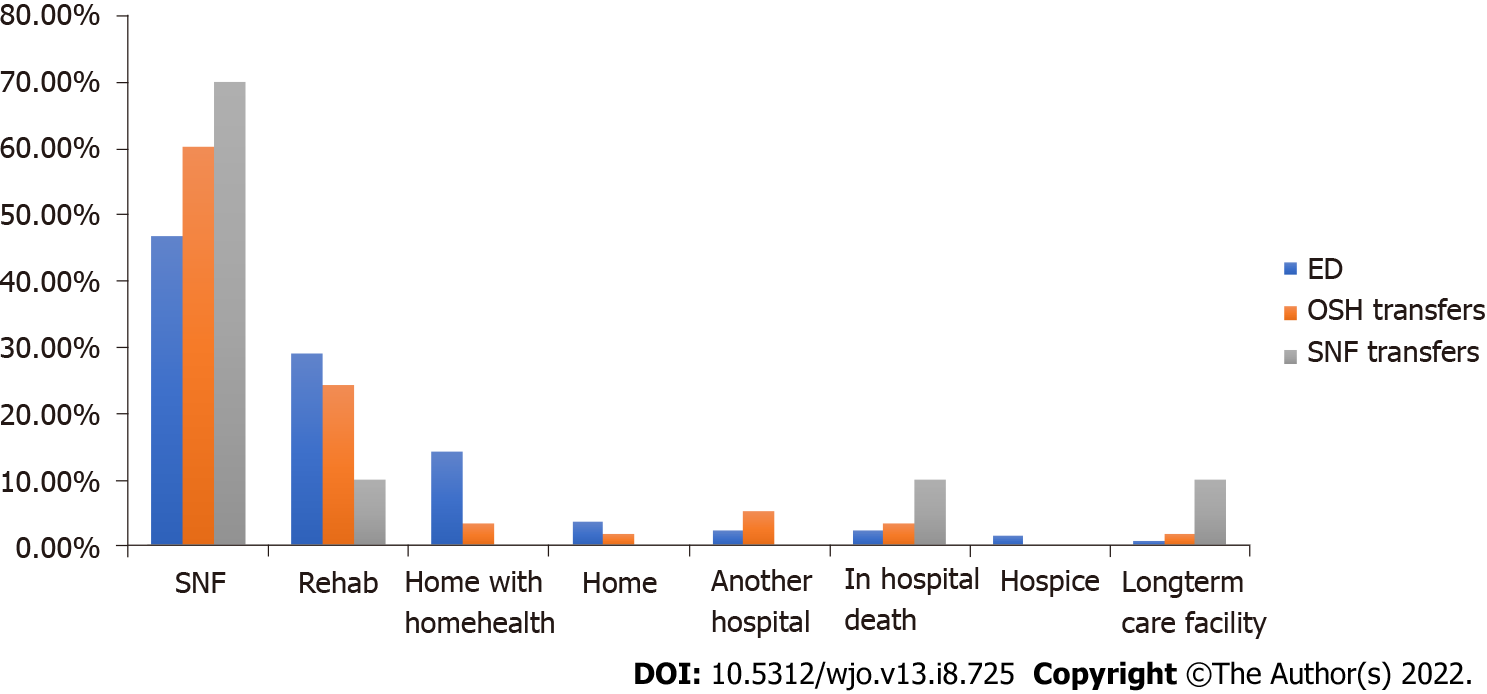
Analysis of patient discharge destination showed that ED patients were more likely to be discharged home than OSH and SNF patients. There were no other statistically significant differences in discharge destination based on point of origin. This data is summarized in Figure 3.
Transfers to regional trauma centers and tertiary care centers of critically ill and severely injured patients have been shown to decrease morbidity and mortality[15,16]. As one might expect given the illness severity seen in many of these transferred patients, increased morbidity, length of stay, blood transfusion requirements, and intensive care utilization has been previously documented in transferred patients[8,11,17]. To our knowledge, this study is the first to document this phenomenon in patients with femoral neck fractures being treated with arthroplasty.
The aim of this study was to compare demographic information, procedure utilization, cost differences, morbidity, and mortality in non-elective hip arthroplasty performed for fracture at an academic medical center based upon patient point of origin. With the nationwide implementation of bundled payments looming, determining the additional risks and costs associated with providing referral services for community and regional hospitals is essential. It is not surprising that patients transferred from an OSH incurred greater costs for their hospitalization than ED and SNF patients. Medically complex patients with significant comorbidities, associated injuries, or critical illness are often difficult for community hospitals to manage and are frequently transferred to tertiary care centers. Previous studies have also found increased cost with non-elective hip arthroplasty compared to elective total hip replacement[4,5].
Our study showed increased length of stay and increased number of average ICU stays per hospitalization for transfered patients from an OSH compared to those patients presenting to our ED. These results are not surprising but demonstrate the greater burden OSH patients place on facilities, staffing, and healthcare providers. It may also reflect that a delay in getting the patient to the operating room can lead to medical complications and morbidity. Our study also found that ED patients were more likely to have ASA 1 or ASA 2 scores compared to SNF and OSH patients. Patients transferred from an OSH also incurred greater costs than those who presented primarily to our ED.
It is clear from our data that patients transferred from an OSH more significantly strain the resources of the receiving tertiary care hospital compared to those patients who present primarily to the ED. This is an important finding in light of proposed bundled care programs. Bundled care programs, which can disincentive hospitals and providers from taking care of sick and costly patients, may increase the number of hip fracture patients being transferred to tertiary care centers especially with clear appropriate transfer guidelines lacking. This would further strain the resources of the receiving hospital and could potentially penalize those centers that are willing to provide care for these vulnerable patients. This is a strong argument for robust risk-adjustment models that potentially even include patient point of origin.
One obvious strength of our study is that it is the first to specifically look at cost and morbidity of hip fracture patients undergoing arthroplasty based on their point of origin. We were able to include a large number of patients over nearly a five year period. All total hip arthroplasty and hemiarthroplasty procedures were performed by three fellowship trained arthroplasty surgeons and therefore, variation in surgeon skill and experience is minimal. The data from our initial database was able to be corroborated through our electronic medical records and any disparities or omissions corrected. Finally, our study was able to determine differences in cost for hospitalizations, not charges, a more accurate representation of reimbursement from Medicare, Medicaid, or private insurance.
This study is not without its limitations. We did not examine the reason for transfer to our facility. This analysis may have allowed us to subcategorize patients based on the indication for the transfer and further determine which specific patient groups or which comorbidities are most likely to lead to increased cost, prolonged hospitalization, increased morbidity, or mortality. Additionally, we did not examine surgical complications, readmissions, or transfusion requirements which are further indicators of morbidity. Another limitation is that this is a retrospective analysis of prospectively collected data. Finally, our entire study was limited to a single institution and is subject to institution specific policies and biases that may limit the generalizability of our conclusions. However, we feel that any tertiary medical center with a large referral basis is likely to find similar results.
Patients transferred from an outside hospital incurred greater costs for their hospitalization than patients presenting from an emergency department or SNF. This is a strong argument for risk-adjustment models when bundling payments for the care of hip fracture patients.
Rising healthcare expenditure, especially with the projected rise in total joint arthroplasty has lead the Center for Medicare Services to propose bundled payments.
Possible effects of bundle payments on tertiary hospital systems have not been evaluated.
This study aims to evaluate potential effects of bundled payment systems on a large tertiary hospital system.
This is a retrospective study of a single hospital system evaluating the observed cost of care for patients presenting with hip fractures from the emergency department, skilled nursing facilities and outside hospital transfers.
Cost data analysis showed that patient transferred from an outside hospital demonstrate significantly higher costs compared to patients from a skilled nursing facility or the emergency department.
Given the increased costs associated with patients transferred from outside hospitals this may call for a risk adjustment models when bundling for the care of hip fracture patients.
Future research will have to further evaluate cost originators to adjust payment models appropriately.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Buckley RE, Canada; Hussain J, Oman S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Altman SH. The lessons of Medicare's prospective payment system show that the bundled payment program faces challenges. Health Aff (Millwood). 2012;31:1923-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472:188-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 358] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 3. | US Centers for Medicare and Medicaid Services. Notice of proposed rulemaking for bundled payments for high-quality coordinated cardiac and hip fracture care. July 25, 2016. Available from: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-07-25.html. |
| 4. | Kamath AF, Austin DC, Derman PB, Israelite CL. Unplanned hip arthroplasty imposes clinical and cost burdens on treating institutions. Clin Orthop Relat Res. 2013;471:4012-4019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Sams JD, Milbrandt JC, Froelich JM, Rainville AD, Allan DG. Hospital outcome after emergent vs elective revision total hip arthroplasty. J Arthroplasty. 2010;25:826-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, Flint L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371-8; discussion 378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 477] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 7. | MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1809] [Cited by in RCA: 1868] [Article Influence: 98.3] [Reference Citation Analysis (0)] |
| 8. | Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a level-I trauma center. J Bone Joint Surg Am. 2007;89:2625-2631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Thakur NA, Plante MJ, Kayiaros S, Reinert SE, Ehrlich MG. Inappropriate transfer of patients with orthopaedic injuries to a Level I trauma center: a prospective study. J Orthop Trauma. 2010;24:336-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Crichlow RJ, Zeni A, Reveal G, Kuhl M, Heisler J, Kaehr D, Vijay P, Musapatika DL. Appropriateness of patient transfer with associated orthopaedic injuries to a Level I trauma center. J Orthop Trauma. 2010;24:331-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Nathens AB, Maier RV, Copass MK, Jurkovich GJ. Payer status: the unspoken triage criterion. J Trauma. 2001;50:776-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 120] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Koval KJ, Tingey CW, Spratt KF. Are patients being transferred to level-I trauma centers for reasons other than medical necessity? J Bone Joint Surg Am. 2006;88:2124-2132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | O'Connell RS, Haug EC, Malasitt P, Mallu S, Satpathy J, Isaacs J, Mounasamy V. Appropriateness of patients transferred with orthopedic injuries: experience of a level I trauma center. Eur J Orthop Surg Traumatol. 2018;28:551-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA. Accepting critically ill transfer patients: adverse effect on a referral center's outcome and benchmark measures. Ann Intern Med. 2003;138:882-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 171] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1153] [Cited by in RCA: 1212] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 16. | Sampalis JS, Denis R, Lavoie A, Fréchette P, Boukas S, Nikolis A, Benoit D, Fleiszer D, Brown R, Churchill-Smith M, Mulder D. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565-79; discussion 579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 286] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 17. | Spain DA, Bellino M, Kopelman A, Chang J, Park J, Gregg DL, Brundage SI. Requests for 692 transfers to an academic level I trauma center: implications of the emergency medical treatment and active labor act. J Trauma. 2007;62:63-7; discussion 67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |