Published online May 18, 2022. doi: 10.5312/wjo.v13.i5.503
Peer-review started: July 4, 2021
First decision: October 18, 2021
Revised: November 7, 2021
Accepted: April 21, 2022
Article in press: April 21, 2022
Published online: May 18, 2022
Processing time: 312 Days and 16.6 Hours
Mycobacterium species (Mycobacterium sp) is an emerging cause of hip and knee prosthetic joint infection (PJI), and different species of this organism may be responsible for the same.
To evaluate the profile of hip and knee Mycobacterium PJI cases as published in the past 30 years.
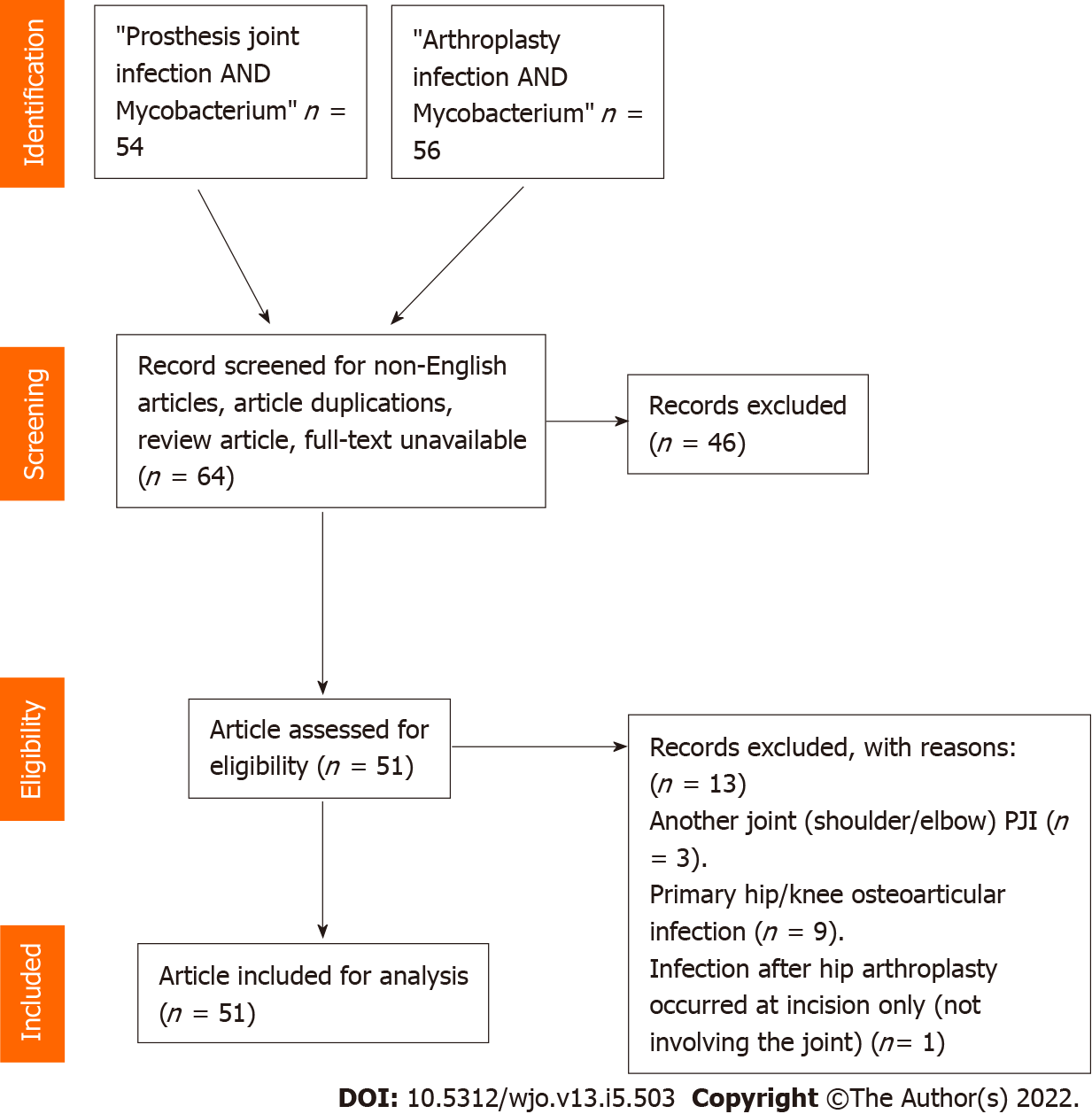
A literature search was performed in PubMed using the MeSH terms “Prosthesis joint infection” AND “Mycobacterium” for studies with publication dates from January 1, 1990, to May 30, 2021. To avoid missing any study, another search was performed with the terms “Arthroplasty infection” AND “Mycobacterium” in the same period as the previous search. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses chart was used to evaluate the included studies for further review. In total, 51 studies were included for further evaluation of the cases, type of pathogen, and treatment of PJI caused by Mycobacterium sp.
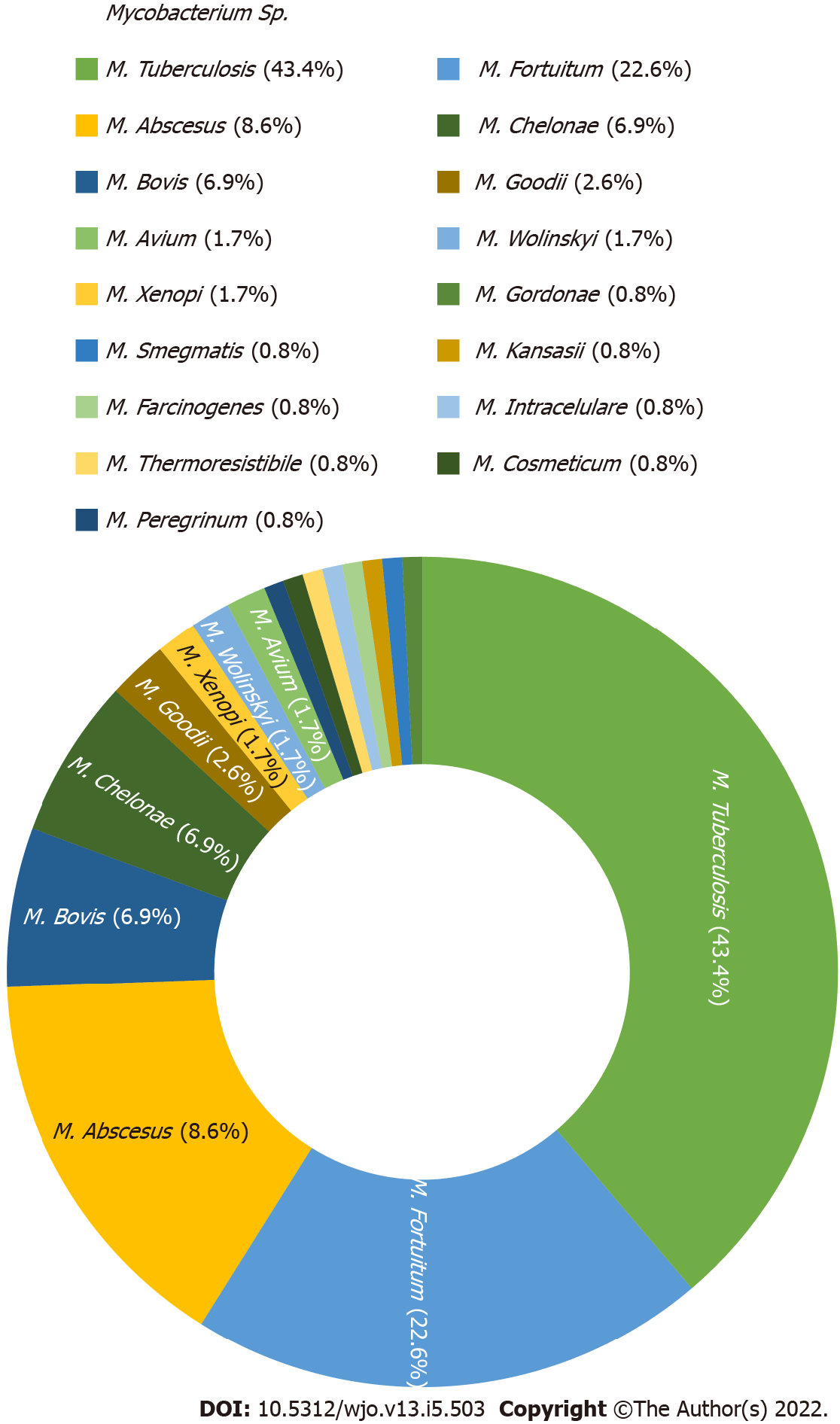
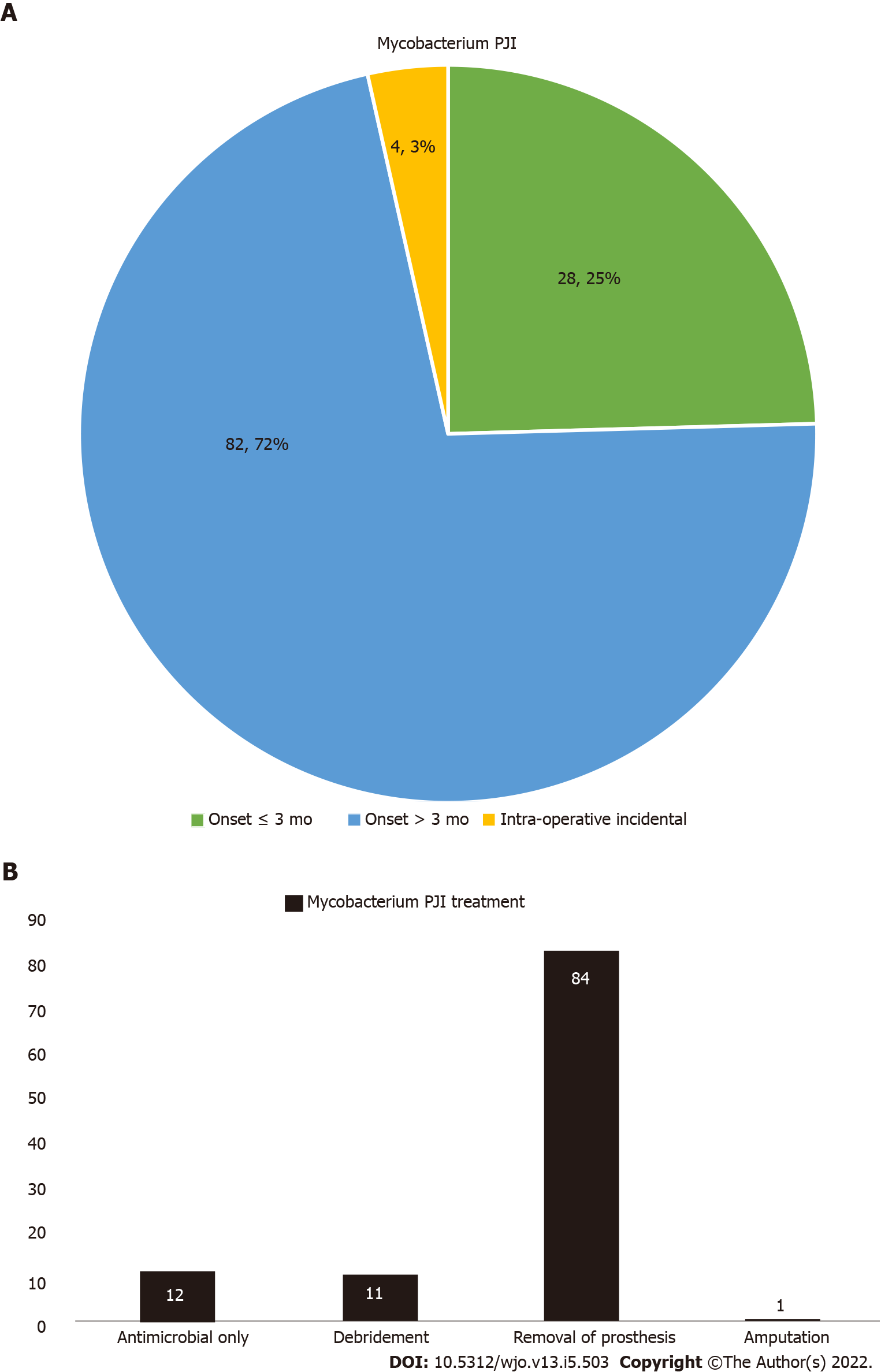
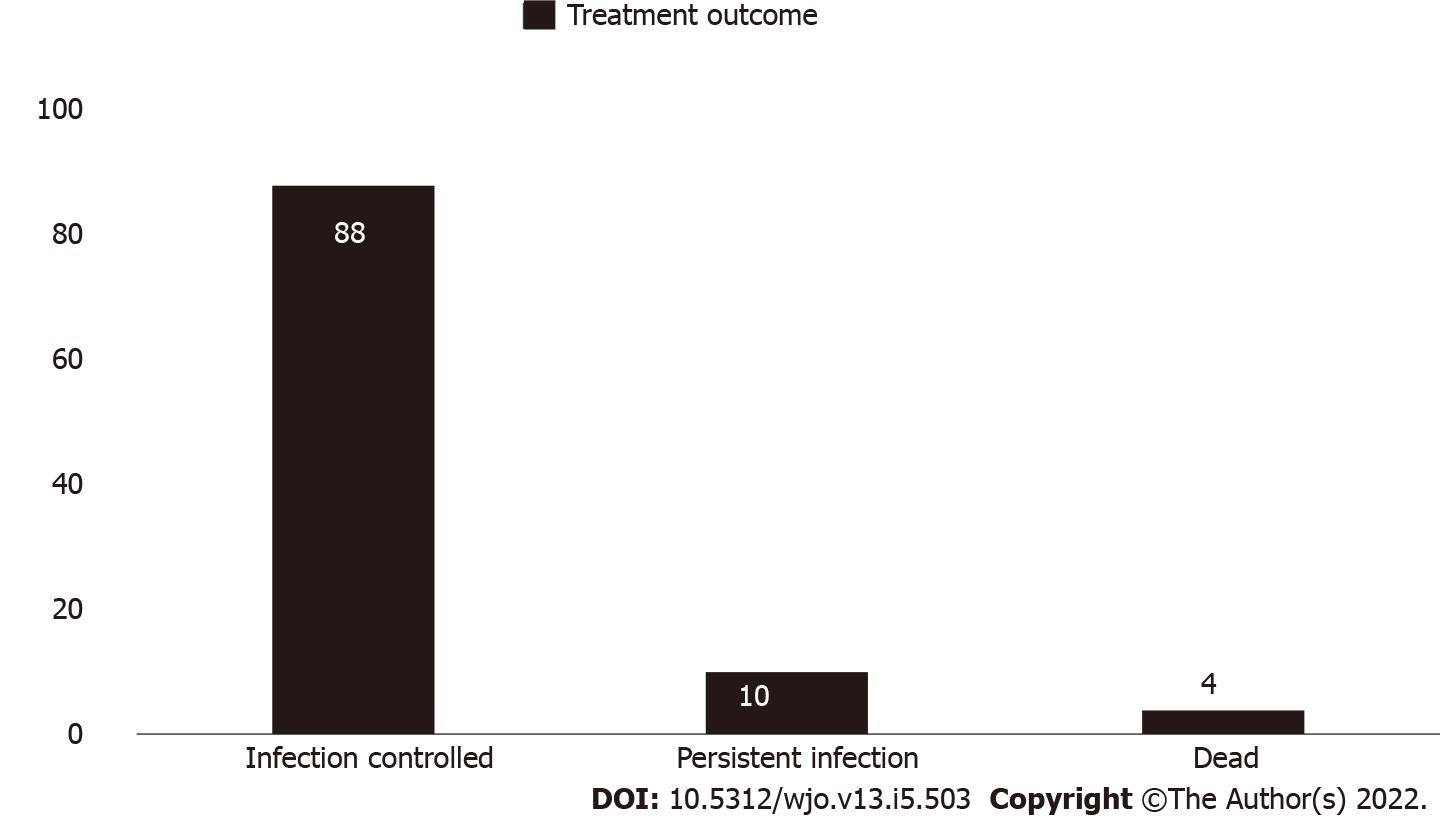
Seventeen identified Mycobacterium sp were reportedly responsible for hip/knee PJI in 115 hip/knee PJI cases, whereas in two cases there was no mention of any specific Mycobacterium sp. Mycobacterium tuberculosis (M. tuberculosis) was detected in 50/115 (43.3%) of the cases. Nontuberculous mycobacteria (NTM) included M. fortuitum (26/115, 22.6%), M. abscessus (10/115, 8.6%), M. chelonae (8/115, 6.9%), and M. bovis (8/115, 6.9%). Majority of the cases (82/114, 71.9%) had an onset of infection > 3 mo after the index surgery, while in 24.6% (28/114) the disease had an onset in ≤ 3 mo. Incidental intraoperative PJI diagnosis was made in 4 cases (3.5%). Overall, prosthesis removal was needed in 77.8% (84/108) of the cases to treat the infection. Overall infection rate was controlled in 88/102 (86.3%) patients with Mycobacterium PJI. Persistent infection occurred in 10/108 (9.8%) patients, while 4/108 (3.9%) patients died due to the infection.
At least 17 Mycobacterium sp can be responsible for hip/knee PJI. Although M. tuberculosis is the most common causal pathogen, NTM should be considered as an emerging cause of hip/knee PJI.
Core Tip: Prosthetic joint infection (PJI) is a difficult complication after total hip/knee arthroplasty. Mycobacterium species (Mycobacterium sp) is one of the emerging causes of hip and knee PJI, and various species could be responsible for it. This study aimed to evaluate the profile of hip and knee Mycobacterium PJI cases published in the past 30 years. This study resulted the information regarding the distribution of Mycobacterium sp that related to PJI hip/knee. This paper also evaluated the disease course, treatment and outcome of Mycobacterium PJI.
- Citation: Santoso A, Phatama KY, Rhatomy S, Budhiparama NC. Prosthetic joint infection of the hip and knee due to Mycobacterium species: A systematic review. World J Orthop 2022; 13(5): 503-514
- URL: https://www.wjgnet.com/2218-5836/full/v13/i5/503.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i5.503
The incidence of prosthetic joint infection (PJI) has increased with an increase in the number of patients undergoing total joint arthroplasty, particularly hip and knee arthroplasties[1]. The cumulative incidence of PJI after total hip arthroplasty (THA) and total knee arthroplasty remains unclear; however, it is believed to range between 2.05% and 2.18%. The majority of PJI cases are caused by gram-positive cocci such as Staphylococcus aureus and coagulase-negative Staphylococci (60%); however, sometimes they can also be caused by gram-negative bacteria, such as Mycobacteria or fungi[2,3]. Mycobacterial infections account for approximately 2% of all PJI cases[4]. Mycobacterium tuberculosis (M. tuberculosis) is an infrequent cause of PJI, accounting for only 7 cases (0.3%) as reported during a 22-year period at one center[5]. However, in tuberculosis-endemic countries, patients undergoing joint arthroplasty with previous tuberculous septic arthritis are at an increased risk of developing M. tuberculosis complex PJI[1]. Some other Mycobacteria (rapidly growing Mycobacteria) are reported to grow rapidly, and they spread in various environments worldwide[4].
Appropriate management is mandatory to prevent complications that arise from PJI. Successful management of PJI is achieved by a combination of surgical intervention and appropriate medical therapeutic strategies to eradicate infection, reduce pain, restore function, and prevent prolonged antimicrobial therapy in patients[1,2,6]. The diagnosis of mycobacterial infections is often delayed due to the low index of suspicion, clinical and laboratory presentation that mimics bacterial infections, and low yield of smears and culture for acid-fast bacilli. Moreover, mycobacterial infections are often known to occur together with other bacteria, such as coinfection or superinfection[2,6]. Delayed diagnosis and prevention of PJI can lead to prolonged illness with various dangerous manifestations that can threaten the patient’s life. Although Mycobacteria are not among the common causative agents of PJI, it is important to recognize and treat them differently from non-mycobacterial infections. The aim of this study was to identify and evaluate the profile of PJI cases due to mycobacterial infection in the hip and knee as published over the past 30 years.
A literature search was performed using MeSH terms on PubMed from January 1, 1990, to May 30, 2021. The following two search scenarios were used accordingly: “Prosthesis joint infection AND Mycobacterium” and “Arthroplasty infection AND Mycobacterium”. The articles were screened based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.
The following inclusion criteria were used in our systematic review: (1) Clinical studies; (2) All levels of evidence; and (3) PJI of the hip or knee due to any Mycobacterium species (Mycobacterium sp). Studies were excluded if they met any of the following criteria: (1) Non-English articles; (2) PJI not involving the hip or knee joint; (3) Primary Mycobacterium hip/knee osteoarticular infection prior to arthroplasty; (4) Articles published in abstract form only; (5) Review articles; and (6) Technique articles.
Three authors (Santoso A, Phatama KY, and Rhatomy S) independently screened the titles and abstracts of the included studies. The first search with the terms “Prosthetic joint infection AND Mycobacterium” revealed 54 records. Of these, 6 records were excluded for not being in English, 5 for presenting primary osteoarticular hip/knee infection, 2 for presenting shoulder/elbow PJI, 1 for presenting wound infection after THA without involvement of the joint, and 3 for unavailability of the full-text articles. The remaining 37 records were included in the further analysis. The second search method was performed with the words “Arthroplasty infection AND Mycobacterium”, which revealed 56 records. Of these, 33 records were excluded for duplicating previous search results, 4 for presenting primary hip/knee osteoarticular infection, 1 for presenting shoulder PJI, 1 for being a non-English article, 2 for being review articles, and 1 for unavailability of the full-text article. Thus, 14 records were finally included from the second search in the analysis. Considering the 37 records from the first search and 14 from the second search, a total of 51 records were included in the final analysis (Figure 1). The analysis included type of study, demographics, number of patients, hip or knee PJI cases, Mycobacterium sp strain, treatment, and outcomes of the mycobacterial PJI cases (Table 1). Furthermore, we performed a descriptive comparison between PJI caused by M. tuberculous (n = 43) and nontuberculous mycobacteria (NTM) (n = 63). This comparative evaluation excluded all cases of mixed infections of M. tuberculous and NTM (n = 1), NTM and Staphylococcus species (Staphylococcus sp) (n = 2), and M. tuberculous and Staphylococcus sp (n = 6). Two cases with no data 5 regarding the specific species of Mycobacteria were also excluded at this stage (Table 2). Comparative analysis of categorical data was performed using the chi-square test.
| No | Ref. | Joint involvement (No. of cases) | Pathogens | Onset of disease (early: ≤ 3 mo; late: > 3 mo) | Treatment | Outcome |
| 1 | Ribeiro et al[7], 2020 | Hip (1) | M. tuberculosis | Early | Removal of prosthesis | Controlled |
| 2 | Patel et al[8], 2019 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 3 | Sixt et al[9], 2020 | Hip (1) | M. avium | Late | Removal of prosthesis | Controlled |
| 4 | Barry et al[10], 2019 | Knee (1) | M. tuberculosis | Late | Antimicrobials only | Controlled |
| 5 | Goldstein et al[11], 2019 | Hip (2), knee (4) | M. intracellulare (1), M. abscessus (1), M. fortuitum (1), M. gordonae (1), NA (2) | Early (1), kate (4), NA (1) | Removal prosthesis (5), amputation (1) | Controlled |
| 6 | Buser et al[12], 2019 | Hip (5), knee (4) | M. fortuitum (7), M. goodii (2) | Early (1), late (8) | NA | NA |
| 7 | Spanyer et al[13], 2018 | Knee (1) | M. abscesus | NA | Removal of prosthesis | Controlled |
| 8 | Meyssonnier et al[14], 2019 | Hip (9) | M. tuberculosis (9) | Late (5), intraoperative (4) | Antimicrobials only (5), removal of prosthesis (4) | Controlled |
| 9 | Chang et al[15], 2018 | Hip (7), knee (6) | M. tuberculosis (13), mixed infection (6) | Early (2), late (11) | Removal of prosthesis (11), debridement (2) | Controlled (8), persistent (3), dead (2) |
| 10 | Metayer et al[16], 2018 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 11 | Elzein et al[5], 2017 | Knee (1) | M. tuberculosis | Late | Removal of prosthesis | Controlled |
| 12 | Kim et al[17], 2017 | Knee (2) | M. abscessus | Early (1), late (1) | Removal of prosthesis (2) | Controlled |
| 13 | Henry et al[18], 2016 | Hip (1), knee (1) | M. abscessus | Late | Removal of prosthesis (2) | Controlled |
| 14 | Jeong et al[19], 2012 | Knee (1) | M. wolinskyi | NA | Debridement | NA |
| 15 | Lee et al[20], 2012 | Knee (1) | M. chelonae | Late | Removal of prosthesis | Controlled |
| 16 | Wang et al[21], 2011 | Knee (1) | M. abscessus, M. fortuitum | Early | Removal of prosthesis | NA |
| 17 | Ahmad et al[22], 2010 | Knee (1) | M. goodii | Early | Removal of prosthesis | Controlled |
| 18 | Gupta et al[23], 2009 | Hip (1) | M. avium complex | Late | Removal of prosthesis | Controlled |
| 19 | Porat et al[24], 2008 | Knee (2) bilateral | M. fortuitum | Late | Antimicrobials only | Persistent |
| 20 | Reigstad et al[25], 2008 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 21 | Brown et al[26], 2008 | Hip (1) | M. tuberculosis, M. chelonae | Late | Removal of prosthesis | Controlled |
| 22 | Cheung et al[27], 2008 | Knee (1) | M. fortuitum | Early | Removal of prosthesis | Controlled |
| 23 | Eid et al[28], 2007 | Knee (7), hip (1) | M. chelonae (3), M. abscessus (2), M. fortuitum (3), M. smegmatis (1) | Early (3), late (5) | Removal of prosthesis | Controlled (7), persistent (1) |
| 24 | Segal et al[29], 2007 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 25 | Khater et al[30], 2007 | Knee (1) | M. tuberculosis | Early | Removal of prosthesis | Controlled |
| 26 | Pulcini et al[31], 2006 | Hip (1) | M. wolinskyi | Late | Removal of prosthesis | Controlled |
| 27 | Neuberger et al[32], 2006 | Knee (1) | M. kansasii | Late | Removal of prosthesis | Controlled |
| 28 | Wong et al[33], 2005 | Hip (1) | M. farcinogenes | Late | Removal of prosthesis | Controlled |
| 29 | Yim et al[34], 2004 | Hip (10) | M. xenopi | Late | Removal of prosthesis | Controlled |
| 30 | Spinner et al[35], 1996 | Knee (1) | M. tuberculosis | Early | Debridement | Controlled |
| 31 | Pring et al[36], 1996 | Knee (1) | M. chelonae | Early | Removal of prosthesis | Controlled |
| 32 | Kreder et al[37], 1996 | Hip (1) | M. tuberculosis | Late | Removal of prosthesis | Controlled |
| 33 | Lusk et al[38], 1995 | Knee (1) | M. tuberculosis | Late | Removal of prosthesis | Dead |
| 34 | Tokumoto et al[39], 1995 | Knee (2), hip (1) | M. tuberculosis | Late | Removal of prosthesis (3) | Controlled |
| 35 | Ueng et al[40], 1995 | Hip (2) | M. tuberculosis | Late | Removal of prosthesis (2) | Controlled |
| 36 | Heathcock et al[41], 1994 | Hip (1) | M. chelonae | Late | Removal of prosthesis | Controlled |
| 37 | Leach et al[42], 1993 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 38 | Guerra et al[43], 1998 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 39 | LaBombardi et al[44], 2005 | Knee (1) | M. thermoresistibile | Early | Removal of prosthesis | Controlled |
| 40 | Saccente[45], 2006 | Knee (1) | M. fortuitum | Early | Removal of prosthesis | Controlled |
| 41 | Wang et al[46], 2007 | Knee (1) | M. tuberculosis | Late | Debridement | Dead |
| 42 | Klein et al[47], 2012 | Knee (1) | M. tuberculosis | Late | Removal of prosthesis | Controlled |
| 43 | Srivastava et al[48], 2011 | Hip (1) | M. bovis | Late | Removal of prosthesis | Controlled |
| 44 | Rispler et al[49], 2015 | Knee (1) | M. bovis | Late | Debridement | Controlled |
| 45 | Vutescu and Koenig[50], 2017 | Knee (1) | M. cosmeticum | Late | Removal of prosthesis | Controlled |
| 46 | Jitmuang et al[4], 2017 | Knee (10), hip (1) | M. fortuitum (9), M. abscessus (1), M. peregrinum (1) (mixed cases 2) | Early (9), late (2) | Removal of prosthesis (10), debridement (1) | Controlled (6), persistent (1), NA (4) |
| 47 | Mannelli et al[51], 2018 | Hip (1) | M. chelonae | Late | Antimicrobials only | Persistent |
| 48 | Uhel et al[52], 2019 | Hip (6), knee (6) | M. tuberculosis | Late (12) | Antimicrobials only (4), removal of prosthesis (5), debridement (3) | Controlled (8), persistent (3), dead (1) |
| 49 | Rodari et al[53], 2020 | Hip (1) | M. xenopi | Late | Removal prosthesis | Controlled |
| 50 | Congia et al[54], 2020 | Knee (1) | M. tuberculosis | Early | Debridement | Controlled |
| 51 | Fix et al[55], 2020 | Hip (1) | M. fortuitum | Early | Removal prosthesis | Controlled |
| Tuberculous PJI (n = 43) | Nontuberculous PJI (n = 63) | P value | |
| Joint involvement | |||
| Hip | 22/43 (55.1%) | 22/63 (34.9%) | 0.096 |
| Knee | 21/43 (44.9%) | 41/63 (65.1%) | |
| Onset of disease after index surgery | |||
| ≤ 3 mo | 5/43 (11.6%) | 22/60 (36.7%) | 0.002 |
| > 3 mo | 34/43 (79.1%) | 38/60 (63.3%) | |
| Intraoperative | 4/43 (9.3%) | 0 | |
| NA | 0 | 3 | |
| Treatment | |||
| Antimicrobial therapy only | 10/43 (23.3%) | 2/54 (3.7%) | 0.002 |
| Debridement | 8 /43(18.6%) | 3/54 (5.5%) | |
| Removal of prosthesis | 25/43 (58.1%) | 48/54 (88.9%) | |
| Amputation | 0 | 1/54 (1.8%) | |
| NA | 0 | 9 | |
| Outcome | |||
| Infection controlled | 35/43 (81.4%) | 44/48 (91.7%) | 0.092 |
| Persistent infection | 4/43 (9.3%) | 4/48 (8.3%) | |
| Dead | 4/43 (9.3%) | 0 | |
| NA | 0 | 15 | |
Of the 51 included studies, 40 (80.3%) were case reports and 11 (19.6%) studies were of the retrospective series type. There were studies from America (27/51, 52.9%), Europe (12/51, 23.5%), and Asia-Pacific (12/51, 23.5%) included in the analysis. In total, 117 Mycobacterium hip/knee PJI cases were reported across 51 studies. There were 46.15% (54/117) cases of knee PJI and 53.85% (63/117) of hip PJI, and the age range of the patients was 17-101 years. In total, 17 types of Mycobacteria sp recorded in this review were responsible for PJI in 115 hip/knee PJI cases, whereas in 2 cases there was no mention of any specific Mycobacterium sp. M. tuberculosis was detected in 50/115 (43.3%) of the cases. The NTM included M. fortuitum (26/115, 22.6%), M. abscessus (10/115, 8.6%), M. chelonae (8/115, 6.9%), and M. bovis (8/115, 6.9%). Other strains with a smaller number of cases were also isolated as the causes of hip/knee PJI (Figure 2). Mixed infections in mycobacterial PJI cases were noted in 8 cases caused by M. abscessus and M. fortuitum (all NTM) in 1 case and by M. tuberculosis and M. chelonae in another. The other six cases showed co infection with Staphylococcus sp. The majority of the cases (82/114, 71.9%) showed an onset of infection > 3 mo after the index surgery, whereas 24.6% (28/114) of patients showed disease onset in ≤ 3 mo. Incidental intraoperative PJI diagnosis was reported in 4 cases (3.5%) (Figure 3A), and it was not specified in 9 cases. Removal of the prosthesis (with or without revision) was needed in 77.8% (84/108) of cases to treat the infection (Figure 3B). While debridement was needed in 11/108 (10.2%) cases, antimicrobial therapy was needed in 12/108 (11.1%), and amputation was performed in 1 case. The overall infection rate was controlled in 88/102 (86.3%) mycobacterial PJI cases. Persistent infection occurred in 10/102 (9.8%) patients, and 4/102 (3.9%) patients died due to the infection (Figure 4). Comparative analysis showed no difference in the rate of hip or knee involvement in PJI with M. tuberculous or NTM (P > 0.05). Both tuberculous and nontuberculous PJI cases predominantly showed disease onset of > 3 mo (79.1% and 63.3%, respectively). However, nontuberculous PJI cases showed a higher rate of early onset (< 3 mo) of disease than those cases with tuberculous PJI (36.7% vs 11.6%). Removal of the prosthesis was needed in more cases of nontuberculous PJI than in cases of tuberculous PJI (88.9% vs 58.1%). The infection control rates were comparable between the tuberculous and nontuberculous PJI cases (81.4% and 91.7%, respectively) (Table 2).
More than 150 Mycobacterium sp have been officially recognized until now, in literature which consist of tuberculous mycobacteria and NTM[56]. One of the purposes of this systematic review was to evaluate the various Mycobacteria sp that can cause hip/knee PJI, and at least 17 Mycobacterium sp were identified accordingly. They comprised of M. tuberculosis and 16 NTM. The NTM was further divided into rapidly growing and slowly growing mycobacteria[56]. Several studies have reported rapidly growing NTM as the cause of early hip/knee PJI[4,17,18,28]. Early PJI (≤ 3 mo) was noted in 36% of the NTM cases in this review, which was higher than that in tuberculous PJI cases (11%). The rapidly growing NTM hence needs to be considered as a differential diagnosis in cases of early hip/knee PJI. The diagnosis of Mycobacterium PJI is sometimes delayed, leading to delays in appropriate management[6,8]. Several treatment options were noted in this review. Removal of the prosthesis was the most commonly performed procedure, which was required in > 75% of cases. Additionally, a greater number of NTM PJI cases required removal of the prosthesis compared to the tuberculous PJI cases (88.9% vs 58.1%). There were no data regarding specific procedures, such as revision surgery, resection arthroplasty, or arthrodesis after the prosthesis removal procedure due to incomplete data in every published article. Another interesting finding was that conservative treatment with only antimicrobial therapy successfully controlled tuberculous hip/knee PJI in approximately 23% of the cases. This indicates that early recognition of sensitive antimicrobial agents is highly important in treating Mycobacterium PJI. However, the isolation of Mycobacterium with standard culture procedures may be sometimes difficult and more advanced techniques with gene sequencing are hence needed to isolate the Mycobacterium sp[19]. This could be a hindrance, especially in developing countries. Based on the pooled case analyses reported from the studies included in this systematic review, the outcome of the treatment of Mycobacterium PJI reportedly had an infection control rate of approximately 86%. Among the mycobacterial PJI cases, the infection control rate of nontuberculous PJI was comparable to that of tuberculous PJI (91.7% vs 81.4%, P = 0.092). This was comparable to that of PJI hip/knee associated with non-mycobacterial pathogens or even a negative-culture PJI that showed an infection control rate of 70%-90%[3,57]. Mycobacterium PJI has also been correlated with culture-negative PJI. A study by Palan et al[58] reported that fungi and mycobacteria are responsible for over 85% of negative-culture PJI. Arthroplasty surgeons need to consider Mycobacterium as the causal pathogen of PJI when negative culture results are obtained in clinical practice. Further diagnosis using histopathology or polymerase chain reaction assay is needed accordingly.
This study had a few limitations. First, the systematic review only included studies indexed in PubMed; therefore, some other studies may have been missed in this review. However, the wider search period (30 years) of this systematic review ensured the inclusion of several important studies from literature. Second, the studies included in this systematic review were mostly retrospective case reports or case series, which had their own limitations. It is difficult to obtain a higher level of evidence from relatively rare cases, such as those of Mycobacterium PJI. Third, some bias of treatment and outcome evaluation may have occurred, as every author may have used a different standard. This study also could not suggest any advisable best treatment for Mycobacterium PJI due to the lack of available data for evaluation. Despite these limitations, we believe that this systematic review could provide some insights into the profile of Mycobacterium hip/knee PJI, including its treatment options and outcomes.
At least 17 Mycobacterium sp can be responsible for PJI of the hip and knee. Although M. tuberculosis is the most common causal pathogen, NTM should be considered as an emerging cause of hip/knee PJI.
There were many species of Mycobacterium that may be associated as a causal pathogens for prosthetic joint infection (PJI) of the hip and knee. However, no available literature which provides compilation data regarding this issue.
To do compilation data of Mycobacterium species (Mycobacterium sp) which may cause hip and knee PJI.
This study aimed to evaluate PJI associated with Mycobacterium sp.
Systematic review of PubMed article.
Among reviewed 51 articles. We found several species of Mycobacterium may be associated with hip and knee PJI.
We found at least 17 species of Mycobacterium could be responsible for hip and knee PJI.
This study may open the knowledge of various species of Myscobacterium that can be associated with hip and knee PJI.
We highly thank Denny Adriansyah, MD for his assistance in data collection and analysis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Luo ZW, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27:302-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1215] [Cited by in RCA: 1284] [Article Influence: 116.7] [Reference Citation Analysis (0)] |
| 2. | Aggarwal VK, Rasouli MR, Parvizi J. Periprosthetic joint infection: Current concept. Indian J Orthop. 2013;47:10-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 100] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Santoso A, Park KS, Shin YR, Yang HY, Choi IS, Yoon TR. Two-stage revision for periprosthetic joint infection of the hip: Culture-negative versus culture-positive infection. J Orthop. 2018;15:391-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Jitmuang A, Yuenyongviwat V, Charoencholvanich K, Chayakulkeeree M. Rapidly-growing mycobacterial infection: a recognized cause of early-onset prosthetic joint infection. BMC Infect Dis. 2017;17:802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Elzein FE, Haris M, Alolayan SS, Al Sherbini N. Total knee prosthesis infected with Mycobacterium tuberculosis. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR; Infectious Diseases Society of America. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 556] [Cited by in RCA: 699] [Article Influence: 58.3] [Reference Citation Analysis (0)] |
| 7. | Ribeiro AF, Inacio Oliveira M, Jordão P, Tavares D, Varandas L, Gouveia C. Mycobacterium tuberculosis prosthesis joint infection. Pediatr Int. 2020;62:97-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Patel A, Elzweig J. Mycobacterium bovis prosthetic joint infection following intravesical instillation of BCG for bladder cancer. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Sixt T, Bador J, Amoureux L, Piroth L, Blot M. Prosthetic joint infection caused by Mycobacterium avium complex. QJM. 2020;113:278-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Barry M, Akkielah L, Askar MA, Bin Nasser AS. Miliary tuberculosis with delayed-onset total knee arthroplasty Mycobacteria tuberculosis infection successfully treated with medical therapy alone: A case report and literature review. Knee. 2019;26:1152-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Goldstein N, St Clair JB, Kasperbauer SH, Daley CL, Lindeque B. Nontuberculous Mycobacterial Musculoskeletal Infection Cases from a Tertiary Referral Center, Colorado, USA. Emerg Infect Dis. 2019;25:1075-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Buser GL, Laidler MR, Cassidy PM, Moulton-Meissner H, Beldavs ZG, Cieslak PR. Outbreak of Nontuberculous Mycobacteria Joint Prosthesis Infections, Oregon, USA, 2010-2016. Emerg Infect Dis. 2019;25:849-855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Spanyer JM, Foster S, Thum-DiCesare JA, Kwon YM, Burke DW, Nelson SB. Mycobacterium abscessus: A Rare Cause of Periprosthetic Knee Joint Infection. Am J Orthop (Belle Mead NJ). 2018;47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Meyssonnier V, Zeller V, Malbos S, Heym B, Lhotellier L, Desplaces N, Marmor S, Ziza JM. Prosthetic joint infections due to Mycobacterium tuberculosis: A retrospective study. Joint Bone Spine. 2019;86:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Chang CH, Hu CC, Chang Y, Hsieh PH, Shih HN, Ueng SW. Two-stage revision arthroplasty for Mycobacterium Tuberculosis periprosthetic joint infection: An outcome analysis. PLoS One. 2018;13:e0203585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Metayer B, Menu P, Khatchatourian L, Preuss P, Dauty M, Fouasson-Chailloux A. Prosthetic joint infection with pseudo-tumoral aspect due to Mycobacterium bovis infection after Bacillus-Calmette-Guerin therapy. Ann Phys Rehabil Med. 2018;61:62-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Kim M, Ha CW, Jang JW, Park YB. Rapidly growing non-tuberculous mycobacteria infection of prosthetic knee joints: A report of two cases. Knee. 2017;24:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Henry MW, Miller AO, Kahn B, Windsor RE, Brause BD. Prosthetic joint infections secondary to rapidly growing mycobacteria: Two case reports and a review of the literature. Infect Dis (Lond). 2016;48:453-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Jeong JH, Seo YH, Kim KH, Ahn JY, Park PH, Park YK. Mycobacterium wolinskyi infection confirmed by rpoB gene sequencing. J Clin Lab Anal. 2012;26:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Lee RP, Cheung KW, Chiu KH, Tsang ML. Mycobacterium chelonae infection after total knee arthroplasty: a case report. J Orthop Surg (Hong Kong). 2012;20:134-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Wang SX, Yang CJ, Chen YC, Lay CJ, Tsai CC. Septic arthritis caused by Mycobacterium fortuitum and Mycobacterium abscessus in a prosthetic knee joint: case report and review of literature. Intern Med. 2011;50:2227-2232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Ahmad S, Khakoo RA. Left knee prosthesis-related Mycobacterium goodii infection. Int J Infect Dis. 2010;14:e1115-e1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Gupta A, Clauss H. Prosthetic joint infection with Mycobacterium avium complex in a solid organ transplant recipient. Transpl Infect Dis. 2009;11:537-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Porat MD, Austin MS. Bilateral knee periprosthetic infection with Mycobacterium fortuitum. J Arthroplasty. 2008;23:787-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Reigstad O, Siewers P. A total hip replacement infected with mycobacterium bovis after intravesicular treatment with Bacille-Calmette-Guérin for bladder cancer. J Bone Joint Surg Br. 2008;90:225-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Brown A, Grubbs P, Mongey AB. Infection of total hip prosthesis by Mycobacterium tuberculosis and Mycobacterium chelonae in a patient with rheumatoid arthritis. Clin Rheumatol. 2008;27:543-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Cheung I, Wilson A. Mycobacterium fortuitum infection following total knee arthroplasty: a case report and literature review. Knee. 2008;15:61-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Eid AJ, Berbari EF, Sia IG, Wengenack NL, Osmon DR, Razonable RR. Prosthetic joint infection due to rapidly growing mycobacteria: report of 8 cases and review of the literature. Clin Infect Dis. 2007;45:687-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Segal A, Krauss ES. Infected total hip arthroplasty after intravesical bacillus Calmette-Guérin therapy. J Arthroplasty. 2007;22:759-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Khater FJ, Samnani IQ, Mehta JB, Moorman JP, Myers JW. Prosthetic joint infection by Mycobacterium tuberculosis: an unusual case report with literature review. South Med J. 2007;100:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Pulcini C, Vandenbussche E, Podglajen I, Sougakoff W, Truffot-Pernot C, Buu-Hoï A, Varon E, Mainardi JL. Hip prosthesis infection due to Mycobacterium wolinskyi. J Clin Microbiol. 2006;44:3463-3464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Neuberger A, Sprecher H, Oren I. Septic arthritis caused by Mycobacterium kansasii in a prosthetic knee joint. J Clin Microbiol. 2006;44:2648-2649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Wong TC, Chan WF, Tsang WL, Yeung SH, Ip FK. Mycobacterium farcinogenes infection after total hip arthroplasty. J Arthroplasty. 2005;20:684-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Yim K, Nazeer SH, Kiska D, Rose FB, Brown D, Cynamon MH. Recurrent Mycobacterium xenopi infection in a patient with rheumatoid arthritis receiving etanercept. Scand J Infect Dis. 2004;36:150-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Spinner RJ, Sexton DJ, Goldner RD, Levin LS. Periprosthetic infections due to Mycobacterium tuberculosis in patients with no prior history of tuberculosis. J Arthroplasty. 1996;11:217-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 36. | Pring M, Eckhoff DG. Mycobacterium chelonae infection following a total knee arthroplasty. J Arthroplasty. 1996;11:115-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 37. | Kreder HJ, Davey JR. Total hip arthroplasty complicated by tuberculous infection. J Arthroplasty. 1996;11:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Lusk RH, Wienke EC, Milligan TW, Albus TE. Tuberculous and foreign-body granulomatous reactions involving a total knee prosthesis. Arthritis Rheum. 1995;38:1325-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 39. | Tokumoto JI, Follansbee SE, Jacobs RA. Prosthetic joint infection due to Mycobacterium tuberculosis: report of three cases. Clin Infect Dis. 1995;21:134-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Ueng WN, Shih CH, Hseuh S. Pulmonary tuberculosis as a source of infection after total hip arthroplasty. A report of two cases. Int Orthop. 1995;19:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Heathcock R, Dave J, Yates MD. Mycobacterium chelonae hip infection. J Infect. 1994;28:104-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Leach WJ, Halpin DS. Mycobacterium bovis infection of a total hip arthroplasty: a case report. J Bone Joint Surg Br. 1993;75:661-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Guerra CE, Betts RF, O'Keefe RJ, Shilling JW. Mycobacterium bovis osteomyelitis involving a hip arthroplasty after intravesicular bacille Calmette-Guérin for bladder cancer. Clin Infect Dis. 1998;27:639-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 44. | LaBombardi VJ, Shastry L, Tischler H. Mycobacterium thermoresistibile infection following knee-replacement surgery. J Clin Microbiol. 2005;43:5393-5394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Saccente M. Mycobacterium fortuitum group periprosthetic joint infection. Scand J Infect Dis. 2006;38:737-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 46. | Wang PH, Shih KS, Tsai CC, Wang HC. Pulmonary tuberculosis with delayed tuberculosis infection of total knee arthroplasty. J Formos Med Assoc. 2007;106:82-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 47. | Klein GR, Jacquette GM. Prosthetic knee infection in the young immigrant patient--do not forget tuberculosis! J Arthroplasty. 2012;27:1414.e1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 48. | Srivastava A, Ostrander J, Martin S, Walter N. Mycobacterium bovis infection of total hip arthroplasty after intravesicular bacille Calmette-Guérin therapy. Am J Orthop (Belle Mead NJ). 2011;40:E226-E228. [PubMed] |
| 49. | Rispler DT, Stirton JW, Gilde AK, Kane KR. Mycobacterium bovid infection of total knee arthroplasty after bacille Calmette-Guérin therapy for bladder cancer. Am J Orthop (Belle Mead NJ). 2015;44:E46-E48. [PubMed] |
| 50. | Vutescu ES, Koenig KM. Mycobacterium cosmeticum Infection After Total Knee Arthroplasty: A Case Report. JBJS Case Connect. 2017;7:e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 51. | Mannelli VK, Rai MP, Nemakayala DR, Kadiri NP. Mycobacterium ChelonaeDeveloping Multidrug Resistance. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 52. | Uhel F, Corvaisier G, Poinsignon Y, Chirouze C, Beraud G, Grossi O, Varache N, Arvieux C, Berre RL, Tattevin P; Groupe d'Epidémiologie et Recherche en Infectiologie Clinique Centre-Ouest (GERICCO). Mycobacterium tuberculosis prosthetic joint infections: A case series and literature review. J Infect. 2019;78:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 53. | Rodari P, Marocco S, Buonfrate D, Beltrame A, Piubelli C, Orza P, Fittipaldo VA, Bisoffi Z. Prosthetic joint infection due to Mycobacterium xenopi: a review of the literature with a new case report. Infection. 2020;48:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 54. | Congia S, Puddu G, Sorrentino G, Dessì G, Marongiu G. Conservative treatment of early-onset tubercular periprosthetic joint infection following total knee arthroplasty. J Infect Dev Ctries. 2020;14:223-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 55. | Fix WC, Sheth NP, Braffman MN. Mycobacterium fortuitum Prosthetic Joint Infection After Total Hip Arthroplasty: A Case Report. JBJS Case Connect. 2020;10:e0343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 56. | Tortoli E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev. 2014;27:727-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 224] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 57. | Santoso A, Yoon TR, Park KS, Anwar IB, Utomo P, Soetjahjo B, Sibarani T. The Results of Two-stage Revision for Methicillin-resistant Periprosthetic Joint Infection (PJI) of the Hip. Malays Orthop J. 2020;14:18-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 58. | Palan J, Nolan C, Sarantos K, Westerman R, King R, Foguet P. Culture-negative periprosthetic joint infections. EFORT Open Rev. 2019;4:585-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |