Published online Apr 18, 2020. doi: 10.5312/wjo.v11.i4.232
Peer-review started: October 29, 2019
First decision: December 12, 2019
Revised: December 19, 2019
Accepted: March 12, 2020
Article in press: March 12, 2020
Published online: April 18, 2020
Processing time: 167 Days and 6.5 Hours
Total hip replacement has become one of the most successful orthopaedic procedures. The length of the femoral stem constitutes one of the most important geometrical and mechanical features of the prosthesis. Several different implants are currently available but data are limited concerning the clinical results for some of these implants.
To report the short-term clinical and radiological results of a novel squared section, tapered design – with four conicity - short stem in total hip replacement.
This is a retrospective study of a prospectively collected data using of MINIMA® short stem in 61 consecutive patients with at least 1 year follow-up. The collected data included patients’ demographics, type of arthritis, bone morphology, perioperative data, clinical results using Harris Hip Score, EuroQol (EQ-5D), pain score and satisfaction rate, complications and radiological results.
Total 61 patients were included in our study with a mean age of 56 years of age (range 25-73 years). The majority of them (68.6%) were women, thirty seven patients (56.9%) were less than 60 years of age and almost half of patients (45.1%) suffered from secondary osteoarthritis (hip dysplasia, osteonecrosis, etc.). The mean time of follow-up examination was 33.4 mo (2.8 years) with a range of 12-57 months (1-4.8 years). In 35 patients (56.9%) the follow-up examination was more than 3 years. No major complications such as revision, periprosthetic fracture, dislocation or infection were presented. Re-admission 90 d postoperatively or laterwas deemed unnecessary for any reason regarding the operation. Respectively, the mean pain score, mean Harris hip score, and mean EQ-5D were improved from 6.3, 58.7 and 77.3 preoperatively to 0.1, 95.1, and 79.8 postoperatively. The Satisfaction rate at the final follow-up was 9.9 (SD 0.3, range 8.0-10.0). All stems were classified as stable bone ingrowth and no radiolucent lineswere revealed in any of the modified Gruens’ zone at the postoperative X-rays. Stem subsidence was within acceptable limits and the incidence of distal cortical hypertrophy was relatively low.
The clinical and radiological results concerning the MINIMA® short stem are excellent according to this first report of this specific design of the short femoral stems. Because of the small number of cases and short-term follow-up of this study, a longer follow up time and more patients’ enrollment is required.
Core tip: Total hip replacement has become one of the most successful orthopaedic procedures. The length of the femoral stem constitutes one of the most important geometrical and mechanical features of the prosthesis. Several different implants are currently available but data are limited concerning the clinical results for some of these implants. Our objective is to report the short-term results of a novel squared section, tapered design –with four conicity- short stem. According to our findings the clinical and radiological results were excellent in the short-term follow-up using the MINIMA® short stem in total hip replacement.
- Citation: Drosos GI, Tottas S, Kougioumtzis I, Tilkeridis K, Chatzipapas C, Ververidis A. Total hip replacement using MINIMA® short stem: A short-term follow-up study. World J Orthop 2020; 11(4): 232-242
- URL: https://www.wjgnet.com/2218-5836/full/v11/i4/232.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i4.232
Total hip replacement (THR) is considered as one of the most successful procedures in orthopaedic surgery[1,2]. The length of the femoral stem is one of the most important geometrical and mechanical characteristics of the prosthesis. Nevertheless, there is no clear scientific evidence concerning the ideal stem length and no consensus regarding the definition of the standard or conventional stems as well as the short stems (SS)[3]. Many authors met the conclusion that SS are those with a length of less than 120 mm[4], while other definitions have also been proposed[3].
The use of SS started more than 30 years ago[5,6]. Clinical studies, meta-analysis as well as comparative studies have shown survival rate similar to conventional stems but for most SS the available data is controversial regarding short or medium term results[7-9]. Several different implants have been currently available[10], classified in different categories[3,11]. Yet, the existing literature regarding clinical results is limited to some of these implants.
Our aim is to report the short-term results of a novel squared section, tapered design –with four conicity- short stem. To the best of our knowledge, this is the first report concerning the clinical use of this particular SS.
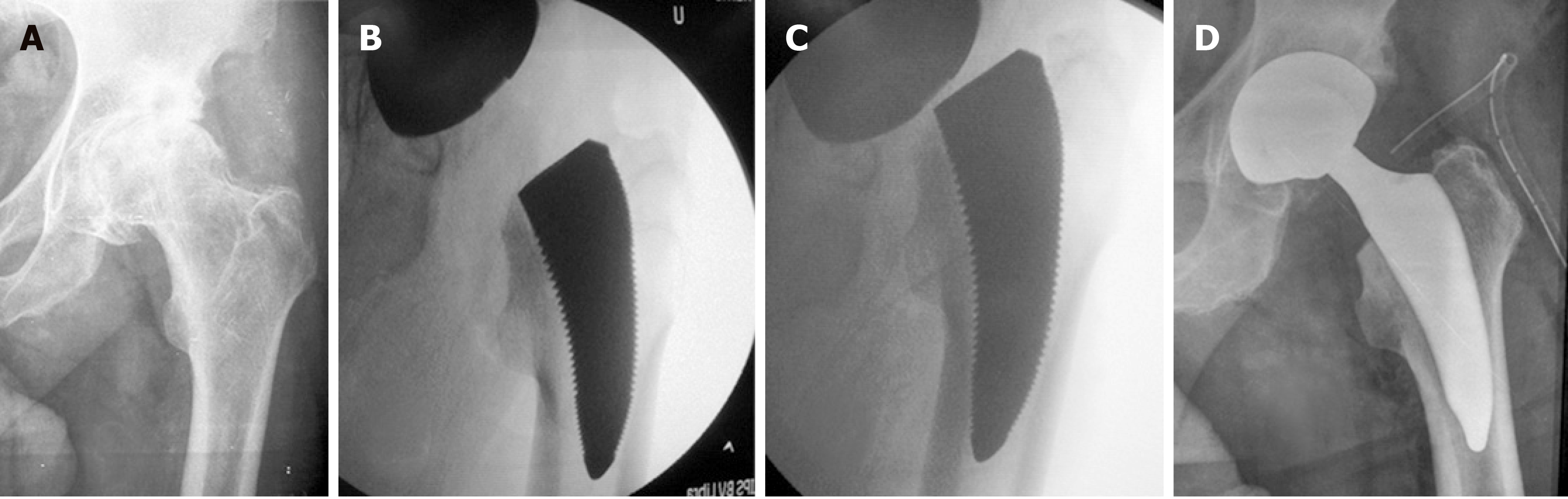
This is a report of a prospectively collected data of 61 consecutive patients undergone THR using the MINIMA® short stem (Lima Corporate, Udine, Italy) (Figure 1) with a minimum follow-up time of 1 year. The study was approved by Ethics committee/Scientific Council of our hospital (SC6/Item 109/28-09-2017).
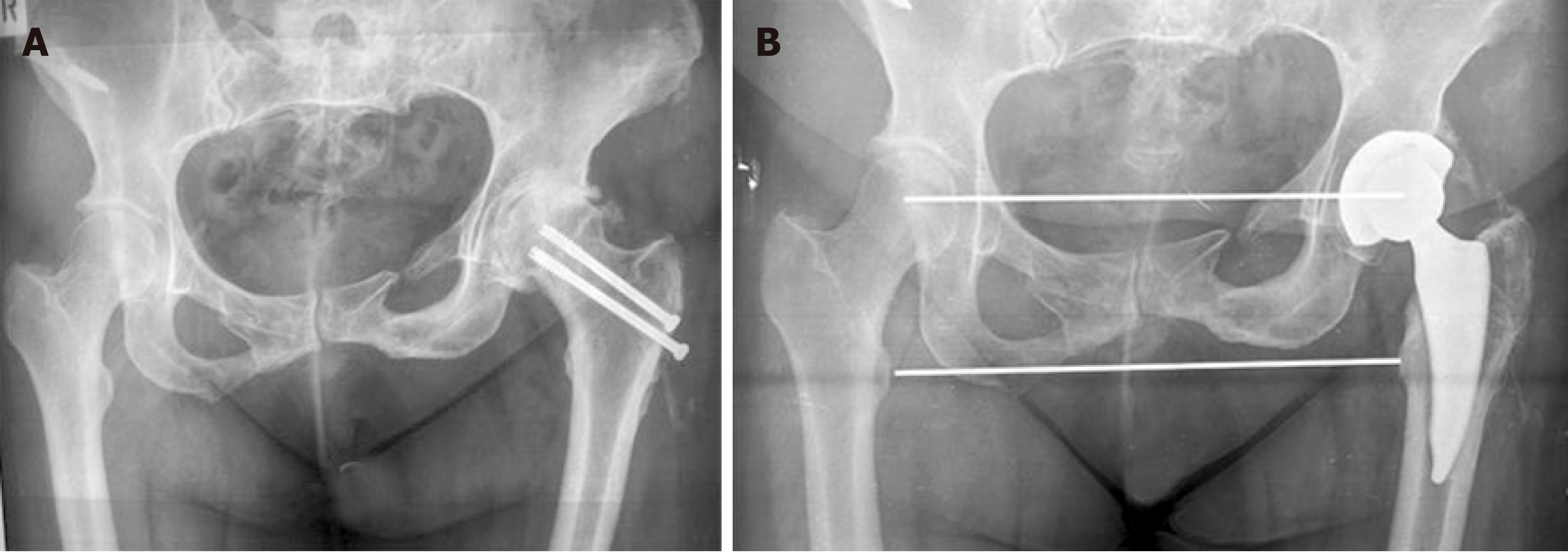
Operations were performed under either general or spinal anesthesia (chosen by the attending anesthesiologists), using a lateral approach (modified Hardinge). Peri-operative antibiotic prophylaxis with a second generation cephalosporin (cefoxitin sodium) for 24 h and anticoagulation protocol with low-weight molecular heparin were applied. The appropriate size and orientation of the femoral component were ensured with fluoroscopy after the trial reduction in all cases (Figure 2).
All patients’ data including demographics, American Society of Anesthesiology physical status classification system[12], Charlson index[13], diagnosis (arthritis type), hip dysplasia according to Hartophylakidis classification[14] femoral morphology according to Dorr’s classification[15], perioperative data including operation time, blood loss, and transfusion rate, length of stay, 90-d re-admissions and complications, were collected prospectively.
The standard postoperative follow-up protocol (at 6 wk, 3 mo, 6 mo, 1 year and every year thereafter) was the same for all patients.
Complications were categorized according to Parvizi et al[16] as systemic (major or minor) and local (major or local).
Clinical results were assessed using Harris hip score[17], EuroQol (EQ-5D) 0-100 scale[18], pain score and satisfaction rate using the VAS/NRS scale[19] (Table 1).
| Characters | Values |
| Number of patients1 | 61 |
| Gender female2 | 42 (68.6%) |
| Gender male2 | 19 (31.4%) |
| Age (yr)3 | 56 ± 11.1 (25-73) |
| BMI3 | 31.2 ± 4.9 (22.8-50.0) |
| ASA3 | 1.8 ± 0.6 (1.0-3.0) |
| Charlson index3 | 1.2 ± 0.5 (0.0-3.0) |
| LOS (d)3 | 3.3 ± 1.1 (2.0-8.0) |
| Operating time (min)3 | 89.9 ± 17.2 (60.0-120.0) |
| Blood loss (mL)3 | 1.154 ± 0.213 (0.735-1.631) |
| Transfusion rate2 | 2 (3.9%) |
| Follow-up (mo)3 | 33.4 ± 15.8 (12-57) |
| Follow-up (yr)3 | 2.8 ± 1.3 (1-4.8) |
| Follow-up more than 3 yr2 | 35 (56.9%) |
| Painpre-operative3 | 6.3 ± 1.9 (2.8-8.0) |
| Pain final follow-up3 | 0.1 ± 0.4 (0.0-2.0) |
| HHS pre- operative3 | 58.7 ± 13.5 (33.0-78.0) |
| HHS final follow-up3 | 95.1 ± 4.9 (83.0-100.0) |
| EQ-5D pre- operative3 | 77.3 ± 16.7 (50.0-95.0) |
| EQ-5D final follow-up3 | 79.6 ± 12.1 (50.0-100.0) |
| Satisfaction final follow-up3 | 9.9 ± 0.3 (8.0-10.0) |
| Complications | |
| Deep vein thrombosis2 | 1 |
The MINIMA® short stem (Lima Corporate, Udine, Italy) is a cementless, squared section, tapered design stem. It is available in 12 sizes and its length varies between 82 mm and 118 mm. This is a type 3 –standard neck osteotomy, trochanteric spearing- stem[11].
Two different uncemented acetabular components were used (1) a Porous Titanium coating - Titanium plasma spray (SPH-Contact® cup, Lima Corp. Udine, Italy); and (2) a Porous Titanium with HA coating (Delta-PF® cup, Lima Corp. Udine, Italy).
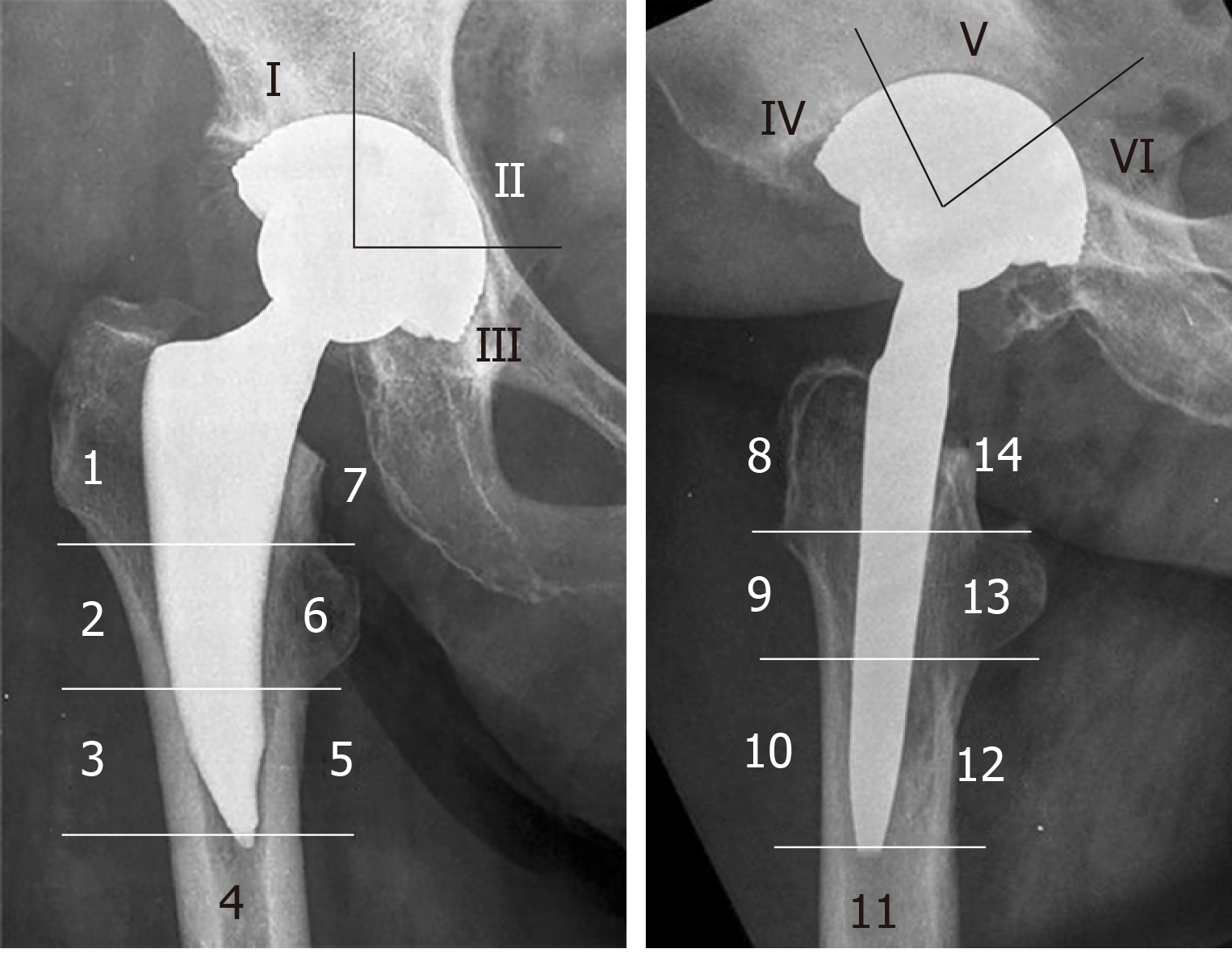
Radiological results were assessed using digital radiographs and a standard system[20]. The modified seven zones of Gruen in anteroposterior and seven zones in lateral radiograph view were evaluated in order to discover any potential (1) radiolucent lines; (2) reactive lines; and (3) cortical hypertrophy[21] (Figure 3).
The femoral stem fixation was classified as stable bone ingrowth, stable fibrous fixation or unstable fibrous fixation[22]. Femoral stem subsidence was measured as the distance between the summit of the lesser trochanter and bottom edge of the stem at 6 wk postoperatively in comparison to the latest follow-up imaging[23].
Leg length discrepancy was measured as the difference between the distances from the inter-teardrop line and the summit of the lesser trochanter of both hips.
Ectopic ossification was probed, according to the classification of Brooker[24].
Proximal femoral stress shielding and bone resorption were investigated, as described by Engh CA[25,26].
Acetabular component evaluation included (1) the presence of radiolucent lines at the bone-prosthesis interface according to DeLee et al[27], 1976; and (2) the cup stability according to Manley et al[28] criteria.
Manual measurements were performed using IMPAX software (Version 6.3, Agfa IMPAX, AGFA-Gevaert N.V, Mortsel, Belgium). The implanted acetabular shell was used for calibration.
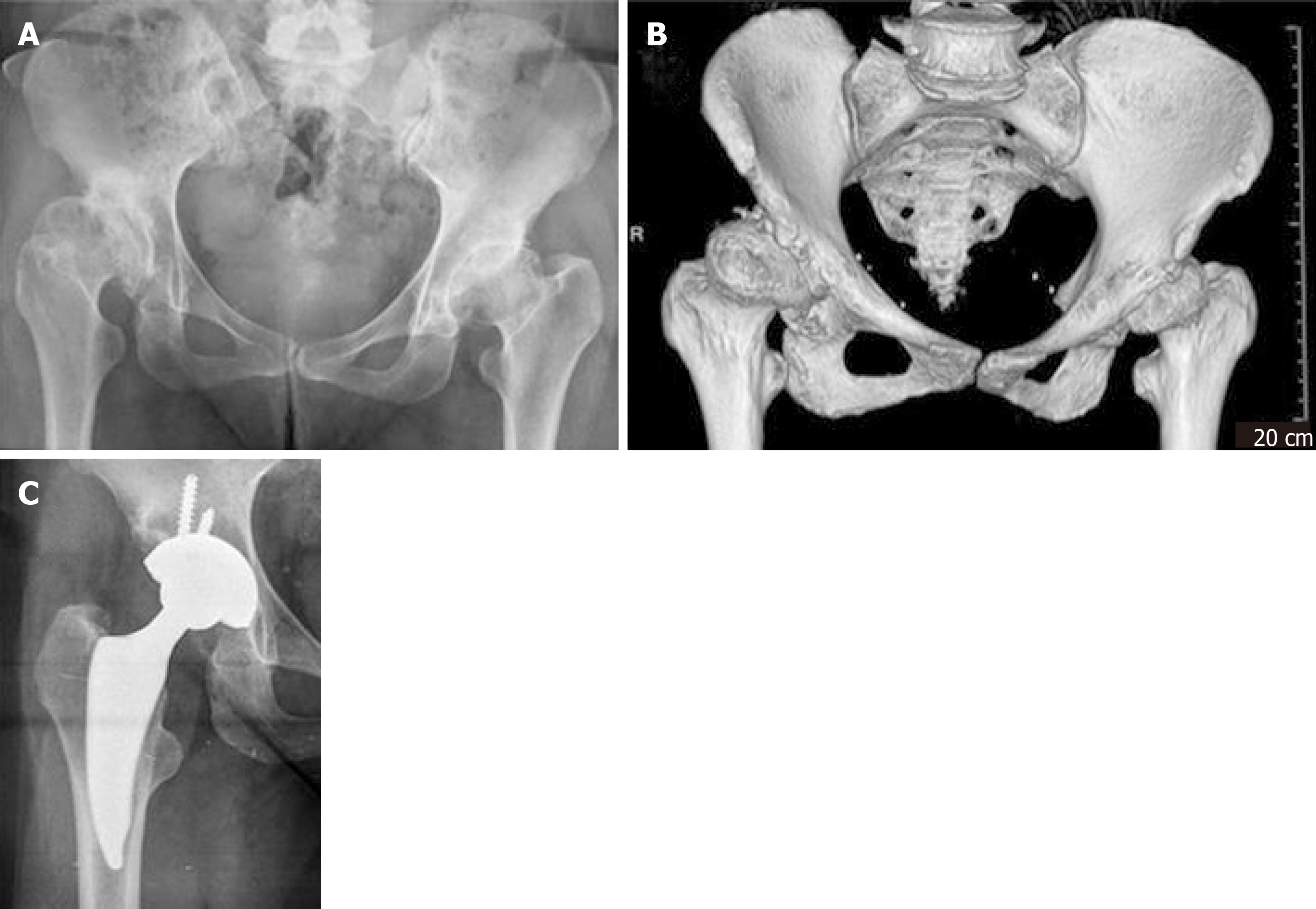
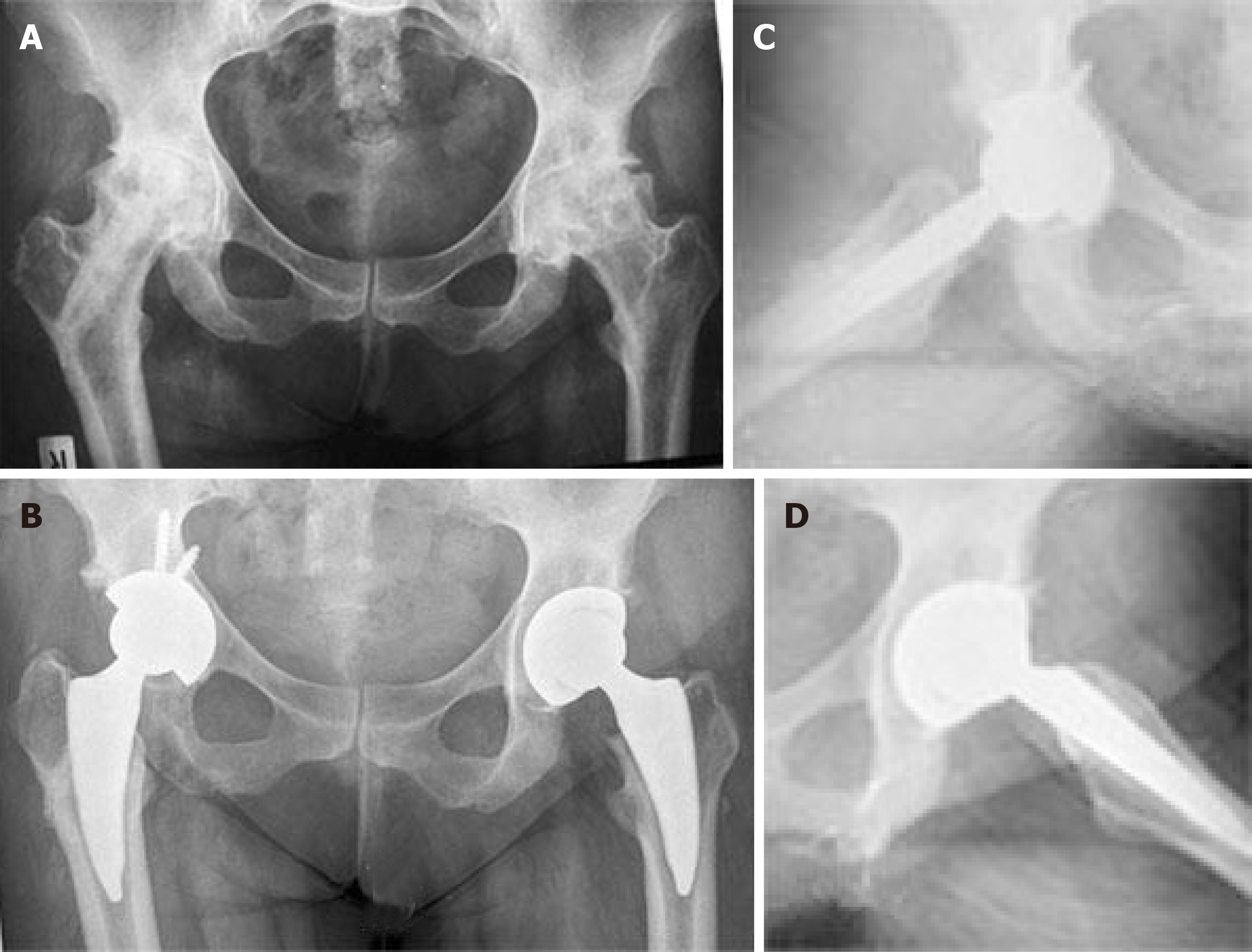
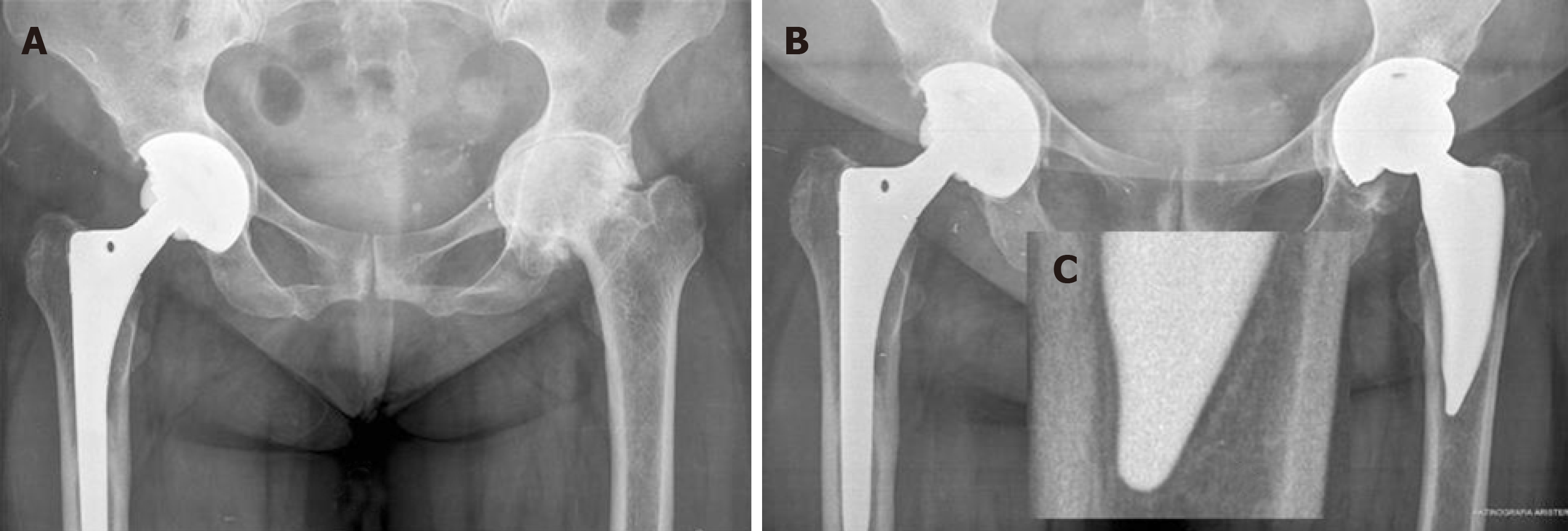
Sixty one patients were included in this study, with a mean age of 56 years of age (range 25-73 years). Thirty seven of our patients (56.9%) were less than 60 years of age and 42 (68.6%) of the patients were women (Table 1). About half of the patients suffered from primary osteoarthritis (n: 33%-54.9%), and the rest of them from secondary osteoarthritis (osteonecrosis, hip dysplasia or other deformities) (Figure 4 and Figure 5), while in 6 patients (9.8%) a previous operation had been performed (femoral osteotomy, vascularized fibular graft, internal fixation for hip fracture) (Figure 5, Figure 6, and Table 2).
| n (%) | |
| Arthritistype | |
| Primaryosteoarthritis | 33 (54.9) |
| Dysplasia (type A)1 | 13 (21.6) |
| Low dislocation (type B)1 | 2 (3.9) |
| Osteonecrosis | 7 (11.8) |
| Post traumaticarthrtis | 4 (5.9) |
| Other | 1 (2.0) |
| Previous operation (osteotomy, Fracture fixation) | 6 (9.8) |
| Proximal femoral morphology (Dorr type) | |
| A | 11 (17.6) |
| B | 48 (78.4) |
| C | 2 (3.9) |
| Ectopic ossification (Brooker classification) | |
| All | 11 (17.6) |
| Class 1 | 6 (9.8) |
| Class 2 | 5 (7.8) |
| Modified Gruen zones | |
| Radiolucent lines | 0 |
| Reactive lines (zones 3, 4, 5) | 2 (3.3) |
| Cortical hypertrophy (zones 3, 5) | 4 (6.6) |
| Subsidencein mm2 | 1.8 ± 0.9 (0.0-3.9) |
| Leg length discrepancy in mm2 | 1.7 ± 5.4 (-17-19) |
The mean time of follow-up was of 33.4 mo (2.8 years) with a range of 12-57 mo (1-4.8 years). In 35 (56.9%) of our patients the follow-up was more than 3 years (Table 1).
Apart from a deep vein thrombosis in one patient at 6 weeks postoperatively, no other complications such us revision, infection, hip dislocation, peri-prosthetic fracture were appeared. Anterior thigh pain was not reported by any of our patients.
Respectively, the mean Pain score, mean HHS, and mean EQ-5D were improved from 6.3, 58.7 and 77.3 preoperatively to 0.1, 95.1, and 79.8 postoperatively (Table 1). The Satisfaction rate at the final follow-up was 9.9 (SD 0.3, range 8.0-10.0).
No patient was re-admitted during the first 90-d nor later for any reason related to the operation.
Femoral stem: The femoral stem was classified as stable bone ingrowth in all patients[22]. No radiolucent lines were observed in any of the modified seven zones of Gruen in anteroosterior and lateral views[21]. Cortical hypertrophy was observed in 4 patients (6.6%) (Figure 7). In 2 patients reactive lines were observed in zones 3, 4 and 5 (Figure 8). The calculated mean stem subsidence was 1.8 mm (SD 0.9, range 0.0-3.9 mm).
Proximal femoral stress shielding and bone resorption were graded radiologically as grade 1 in all patients[25].
The mean leg length discrepancy was 1.7 mm (SD 5.4) with a wide range (from -17 to 19 mm) due to the relatively high prevalence of patients with a secondary osteoarthritis (45.1%), -dysplastic hips, bilateral in most cases.
Acetabular component: No radiolucent lines were observed in any zones according to DeLee et al[27] (1976). All cups were classified as stable according to Manley et al[28] (1998) criteria.
According to the findings of the present study the clinical and radiological results were excellent in the short-term follow-up using the MINIMA® short stem in THR. Despite the short follow-up time and the small number of cases, no revision for any cause was performed, no radiological signs for loosening or impending loosening were observed, no periprosthetic fractures were presented and clinical scores and patients’ satisfaction were excellent.
Comparing our results to those of the existing literature, it is difficult to draw safe conclusion, because there are no other report concerning the use of this particular stem in THR. A recent review of the literature has shown that the calculated overall median revision rate is comparable to those of conventional stems of National Registries, but the survival rate of SS depends on the type of the stem[9]. The best results have been reported for type 2 stems followed by the type 3 stems, while the revision rate for type 1 has been disappointing. The MINIMA® short stem belongs to the type 3 category – a standard femoral neck osteotomy stem.
Furthermore, the available comparative studies and a subsequent meta-analysis have shown no significant differences between SS and conventional stems in the short-term follow-up[8].
However, the available clinical results (either observational or comparative studies) are limited to some of the several different implants that have been currently used.
Despite their theoretical advantages and the reported encouraging results the use of SS has not gained yet a wide acceptance among the orthopaedic surgeons.
The advantages of using short stems in THR’s include (1) the removal of less bone in the proximal femur; (2) a subsequent “easier” stem revision as less bone is expected to be “violated”; (3) less bone remodeling or bone mineral changes of the proximal femur (proximal stress-shielding); and (4) less anterior thigh pain. Finally, another important benefit of short stems is that enables surgeons to overcome the problem of the proximal-distal mismatch due to Dorr type A femur, femoral shape or femoral deformity.
In our series, no cases with stem revision were required, therefore we cannot confirm the “easiness” of revision. The future will show the benefit for our patients since 37 (56.9%) of these patients were less than 60 years of age and some or most of them are going to undergo a revision surgery in the future.
No cases with postoperative thigh pain were observed. The MINIMA® short stem was used in 11 (17.6%) patients with Dorr type A femur.
Proximal bone remodeling or bone mineral changes were not estimated in our study. Bone remodeling seems to be less for short stems according to a recent literature review, although the results are not the same for all SS designs[29]. Furthermore, according to a recent report based on data from the existing literature, the bone mineral changes around femoral stems (cemented, cementless, conventional and short stems) are not predictive for the level the satisfaction of long term clinical outcomes regarding total hip arthroplasty[30]. Therefore, the authors suggested that studies with a follow up shorter than 5-10 years are perhaps clinically irrelevant[30].
The three main concerns for short stems are (1) the possible stem malposition (and stem undersizing) due to lack of distal extension to guide position within the canal and subsequent stem subsidence; (2) possible inadequate early stability, stem micromotion and subsequent fibrous ingrowth instead of bone ingrowth; and (3) the long-term clinical results.
We believe that the routine use of intra-operative fluoroscopy guaranteed proper implant orientation and correct sizing in our series. This fact eliminated the influence of the surgical technique as a confounding factor in stems’ survivorship.
As far as the early stem stability is a concern, our clinical impression is that it is provided by the design of this particular stem. Specifically, it is (1) the taper design -with four taper conicity- to avoid sinking; and (2) the squared section providing torsional stability.
The long-term results concerning the use of MINIMA® short stem cannot be predicted from the results of this study.
Roentgen stereophotogrammetric analysis is generally accepted as the most accurate method of femoral stem subsidence (distal migration),as well as Einzel-Bild-Roentgen-Analyse femoral component analysis, which also allows accurate measurement of femoral stem subsidence[31-33]. The IMPAX software, which was used in the present study, has been used before[34], although we are not aware of its accuracy in measuring the stems’ distal migration.
Stem subsidence was within acceptable limits in our series. It was calculated more than 3 mm only in 3 patients, but no other radiological signs or symptoms of stem loosening were recorded.
Femoral stem subsidence is usually measured using as reference points the tip of the greater trochanter and the proximal end of the femoral stem[35].
We noticed, that radiographic changes of the tip of the greater trochanter –heterotopic ossification- in 11 (17.6%) of our patients were presented. This fact made the measurement less reliable in some cases in our study. Therefore, we used as reference points the summit of the lesser trochanter and the bottom edge of the stem for measurement of the femoral stem subsidence[23].
The incidence of distal cortical hypertrophy varies among different studies. Despite the different hypotheses for its development and the excellent short-term clinical results, the exact cause or pathogenesis and the long-term clinical results in patients with this radiological finding remains unknown[36].
The incidence in our study was relatively low, since in 4 (6.6%) of our patients a cortical hypertrophy was observed in Gruen’s modified ones 3 and 5. Nevertheless, a careful follow-up of these patients is required.
The main limitation of this study is the fact that it is a clinical and radiological report with a small number of cases and short-term follow-up. Future studies with large number of patients and longer follow-up time are required in order to ensure the safety and efficacy of using this particular short stem in THR patients.
Nevertheless the clinical and radiological results are excellent, without major complications and the follow-up in 56.9% of our patients is more than 3 years.
Total hip replacement is considered as one of the most successful procedures in orthopedic surgery. The length of the femoral stem is one of the most important geometrical and mechanical characteristics of the prosthesis. The use of short stems started more than 30 years ago.
Clinical studies, meta-analysis as well as comparative studies have shown similar survival rate between conventional and short stems. However, for most short stems the available data is controversial regarding short or medium term results. Several different implants have been currently available, classified in different categories. Yet, the existing literature regarding clinical results is limited to some of these implants.
Our aim is to report the short-term clinical and radiological results of a novel squared section, tapered design –with four conicity- short stem in total hip replacement.
This is a report of a prospectively collected data of 61 consecutive patients undergone total hip replacement using the MINIMA® short stem (Lima Corporate, Udine, Italy) with a minimum follow-up time of 1 year.
The mean time of follow-up was of 33.4 mo (2.8 years) with a range of 12-57 months (1-4.8 years). Apart from a deep vein thrombosis in one patient at 6 weeks postoperatively, no other complications such us revision, infection, hip dislocation, peri-prosthetic fracture were appeared. Additionally, the functional outcomes, pain score and satisfaction rate were significantly improved at the postoperative follow- up period. The femoral stem was classified as stable bone ingrowth in all patients. No radiolucent lines were observed in any of the modified seven zones of Gruen in anteroposterior and lateral views. Regarding the femoral component, no radiolucent lines were observed in any zones according to DeLee and Charnley.
The clinical and radiological results of our study are considered as excellent, without major complications and the follow-up in 56.9% of our patients is more than 3 years.
Further research based on well designed studies with longer follow-up examination need to be performed, in order to elucidate the efficacy of short stems.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Anand A, Cui Q S-Editor: Wang JL L-Editor: A E-Editor: Liu MY
| 1. | Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1270] [Cited by in RCA: 1340] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 2. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1786] [Article Influence: 99.2] [Reference Citation Analysis (0)] |
| 3. | Feyen H, Shimmin AJ. Is the length of the femoral component important in primary total hip replacement? Bone Joint J. 2014;96-B:442-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Stulberg SD, Patel RM. The short stem: promises and pitfalls. Bone Joint J. 2013;95-B:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Pipino F, Keller A. Tissue-sparing surgery: 25 years’ experience with femoral neck preserving hip arthroplasty. J Orthopaed Traumatol. 2006;7:36–41. [RCA] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Morrey BF. Short-stemmed uncemented femoral component for primary hip arthroplasty. Clin Orthop Relat Res. 1989;169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | van Oldenrijk J, Molleman J, Klaver M, Poolman RW, Haverkamp D. Revision rate after short-stem total hip arthroplasty: a systematic review of 49 studies. Acta Orthop. 2014;85:250-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Huo SC, Wang F, Dong LJ, Wei W, Zeng JQ, Huang HX, Han QM, Duan RQ. Short-stem prostheses in primary total hip arthroplasty: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016;95:e5215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Hauer G, Vielgut I, Amerstorfer F, Maurer-Ertl W, Leithner A, Sadoghi P. Survival Rate of Short-Stem Hip Prostheses: A Comparative Analysis of Clinical Studies and National Arthroplasty Registers. J Arthroplasty. 2018;33:1800-1805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Gómez-García F, Fernández-Fairen M, Espinosa-Mendoza RL. A proposal for the study of cementless short-stem hip prostheses. Acta Ortop Mex. 2016;30:204-215. [PubMed] |
| 11. | Drosos GI, Touzopoulos P. Short stems in total hip replacement: evidence on primary stability according to the stem type. Hip Int. 2019;29:118-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Owens WD, Felts JA, Spitznagel EL. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1437] [Cited by in RCA: 1471] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 13. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 38208] [Article Influence: 1005.5] [Reference Citation Analysis (0)] |
| 14. | Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70:182-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 132] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 579] [Cited by in RCA: 663] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 16. | Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: When do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 143] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 17. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4722] [Cited by in RCA: 4633] [Article Influence: 82.7] [Reference Citation Analysis (0)] |
| 18. | Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3986] [Cited by in RCA: 4402] [Article Influence: 151.8] [Reference Citation Analysis (0)] |
| 19. | Chapman CR, Casey KL, Dubner R, Foley KM, Gracely RH, Reading AE. Pain measurement: an overview. Pain. 1985;22:1-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 744] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 20. | Johnston RC, Fitzgerald RH, Harris WH, Poss R, Müller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg Am. 1990;72:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 559] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 21. | Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;17-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 258] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 22. | Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;107-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 280] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 23. | Albers A, Aoude AA, Zukor DJ, Huk OL, Antoniou J, Tanzer M. Favorable Results of a Short, Tapered, Highly Porous, Proximally Coated Cementless Femoral Stem at a Minimum 4-Year Follow-Up. J Arthroplasty. 2016;31:824-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2419] [Cited by in RCA: 2227] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 25. | Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1214] [Cited by in RCA: 1122] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 26. | Engh CA Jr, Claus AM, Hopper RH, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res. 2001;137-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 101] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;20-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 212] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Manley MT, Capello WN, D'Antonio JA, Edidin AA, Geesink RG. Fixation of acetabular cups without cement in total hip arthroplasty. A comparison of three different implant surfaces at a minimum duration of follow-up of five years. J Bone Joint Surg Am. 1998;80:1175-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 105] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Yan SG, Weber P, Steinbrück A, Hua X, Jansson V, Schmidutz F. Periprosthetic bone remodelling of short-stem total hip arthroplasty: a systematic review. Int Orthop. 2018;42:2077-2086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 30. | Karachalios T, Palaiochorlidis E, Komnos G. Clinical relevance of bone remodelling around conventional and conservative (short-stem) total hip arthroplasty implants. Hip Int. 2019;29:4-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Kärrholm J, Borssén B, Löwenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br. 1994;76:912-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 412] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 32. | Biedermann R, Krismer M, Stöckl B, Mayrhofer P, Ornstein E, Franzén H. Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Röntgen-Analyse-femoral component analysis. J Bone Joint Surg Br. 1999;81:266-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | Wilkinson JM, Hamer AJ, Elson RA, Stockley I, Eastell R. Precision of EBRA-Digital software for monitoring implant migration after total hip arthroplasty. J Arthroplasty. 2002;17:910-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Boese CK, Bredow J, Ettinger M, Eysel P, Thorey F, Lechler P, Budde S. The Influence of Hip Rotation on Femoral Offset Following Short Stem Total Hip Arthroplasty. J Arthroplasty. 2016;31:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Kim YH, Kim VE. Early migration of uncemented porous coated anatomic femoral component related to aseptic loosening. Clin Orthop Relat Res. 1993;146-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 36. | Thalmann C, Horn Lang T, Bereiter H, Clauss M, Acklin YP, Stoffel K. An excellent 5-year survival rate despite a high incidence of distal femoral cortical hypertrophy in a short hip stem. Hip Int. 2020;30:152-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |