Published online Feb 10, 2014. doi: 10.5306/wjco.v5.i1.28
Revised: November 5, 2013
Accepted: November 18, 2013
Published online: February 10, 2014
Processing time: 153 Days and 13 Hours
Leiomyosarcoma is a rare form of cancer commonly found in the retroperitoneum, uterus, stomach, small intestine and vascular tissue. Surgery with a wide margin of resection is the most effective treatment. Nevertheless, metastasis is common and generally occurs within the first 3 years. The liver and lungs are the most common sites of metastasis in leiomyosarcoma. Other sites of metastasis include bone, spleen, soft tissues and brain. Metastatic tumours of the clitoris are extremely rare. As cited in the literature, the most common cancers that metastasize to the clitoris are breast, bladder, renal and gastric. Here, we report a case of a clitoral mass in a 64-year-old woman who received an operation for retroperitoneal leiomyosarcoma 4 years prior. Mass resection was performed. The pathological diagnosis was a leiomyosarcoma metastasis. The patient also presented with brain and lung metastases at the time of the clitoral metastasis. This is the first case of clitoral and brain metastases originating from a retroperitoneal leiomyosarcoma.
Core tip: This is the first case of a clitoral metastasis originating from a retroperitoneal leiomyosarcoma. Furthermore, this report highlights the importance of atypical metastases in leiomyosarcomas.
- Citation: Cokmert S, Demir L, Akyol M, Bayoglu IV, Can A, Unek IT, Bolat FA. Clitoris metastasis from a retroperitoneal leiomyosarcoma: A case report. World J Clin Oncol 2014; 5(1): 28-32
- URL: https://www.wjgnet.com/2218-4333/full/v5/i1/28.htm
- DOI: https://dx.doi.org/10.5306/wjco.v5.i1.28
Leiomyosarcoma is the third most frequently diagnosed soft-tissue sarcoma in adults, after malignant fibrous histiocytoma and liposarcoma[1]. Leiomyosarcomas can arise at any site in the human body where smooth muscles are present; however, the tumours primarily arise in the retroperitoneum, subcutaneous tissue of the extremities, uterus, gastrointestinal tract and large vessels[1,2]. Leiomyosarcomas have a propensity for haematogenous spread and rarely metastasize to the lymph nodes. The liver and lungs are the most common sites of metastasis for leiomyosarcomas[2] and most patients develop distant metastases within long years following primary tumour resection[2-4]. Here, we report a case of a metastasis to the clitoris an unexpected metastasis site, in a 64-year-old woman who received an operation for retroperitoneal leiomyosarcoma 4 years prior.
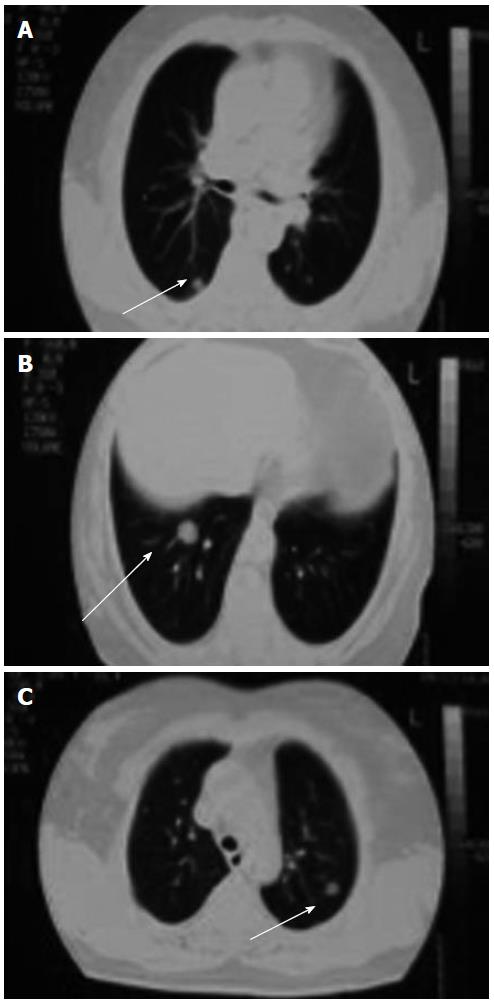
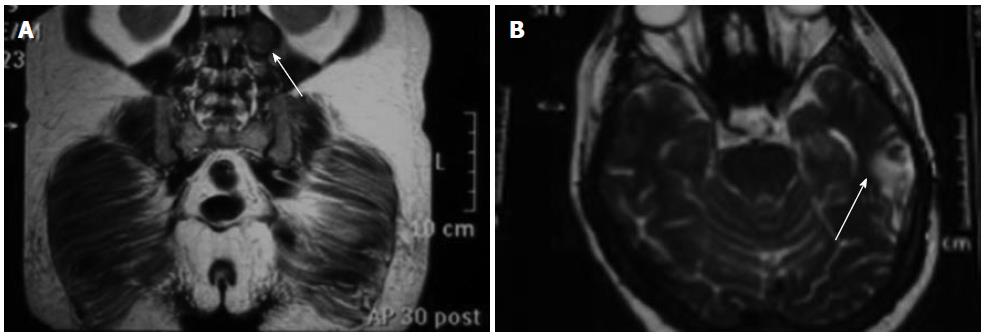
A 64-year-old woman was referred with a 1-mo history of a painful mass in the clitoris. A 2 cm polypoid mass with regular margins in the clitoris was revealed upon vaginal examination (Figure 1). The computed tomography of the chest indicated multiple bilateral pulmonary metastases (Figure 2), and abdominal magnetic resonance imaging showed a mass lesion on the left psoas muscle (Figure 3A). In addition, brain magnetic resonance imaging showed a metastatic mass lesion located in the left temporo-parietal region (Figure 3B). The patient’s medical history revealed that she had undergone a total hysterectomy and bilateral salpingo-oophorectomy at the age of 60 years. During the surgery, a retroperitoneal mass lesion on the psoas muscle under the left kidney had been incidentally determined. The mass lesion was completely removed. A histological examination revealed chronic cervicitis, endocervical polyps, endometrial polyps, corpus albicans in the right and left ovary, paratubal cysts, bilateral chronic salpingitis in total abdominal hysterectomy and bilateral salpingo-oophorectomy specimens, and retroperitoneal leiomyosarcoma in the mass lesion on the psoas muscle under the left kidney. Surgical margins were clearly detected. Distant metastasis was not determined. The patient had refused to undergo chemotherapy and radiotherapy.
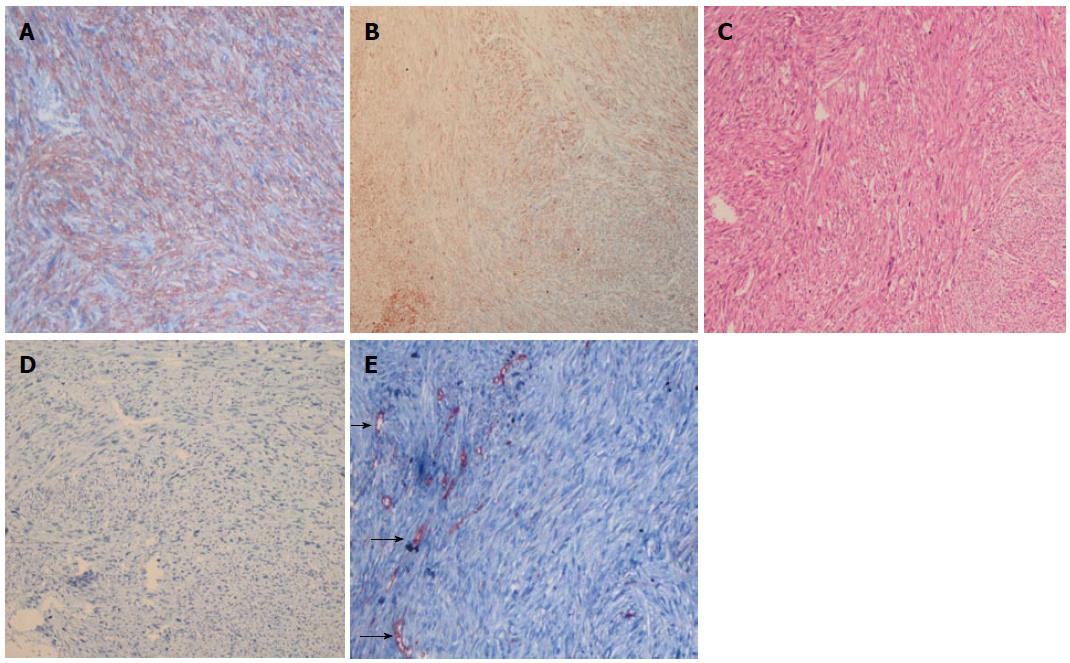
Based on this information, a diagnosis of metastatic retroperitoneal leiomyosarcoma was proposed, and the mass in the clitoris was removed with a wide local excision. The diameter of the clitoral metastatic mass was 2 cm × 1.8 cm, and 6-8 mitoses were microscopically detected per 10 high-power fields. The tumour was well differentiated and immunoreactive for α-smooth muscle actin and desmin (Figure 4A). The histological diagnosis was low-grade leiomyosarcoma of the clitoris. A retroperitoneal leiomyosarcoma specimen was re-examined to distinguish whether the clitoral mass was a metastasis or the primary tumour. The retroperitoneal tumour was composed of spindle-shaped cells with abundant eosinophilic cytoplasm and elongated nuclei (Figure 4B). Most nuclei were centrally located, blunt-ended and “cigar-shaped”. In some areas of the tumour, the nuclear hyperchromatism and pleomorphism were notable. The tumour was composed of compact cellular areas with focal myxoid change. Coagulative necrosis was evident. Mitotic figures were frequent (7-8/10 high-power fields), and atypical mitoses were common. The atypical spindle cells appeared yellow after histochemical staining using the Van Gieson elastic stain. Upon immunohistochemical analysis, the tumour cells were diffusely and strongly positive for smooth muscle actin (Figure 4C), caldesmon and vimentin. In contrast, the tumour cells were negative for desmin (Figure 4D), S-100 protein, epithelial membrane antigen, CD117 and CD 34 (Figure 4E). Approximately 15% of the tumour cells were Ki-67 positive. The surgical margins were clear. Thus, the histopathological and immunohistochemical findings were consistent with leiomyosarcoma of the retroperitoneum. The morphological and immunohistochemical results of the clitoral mass were similar to that of the retroperitoneal mass except for desmin positivity. Based on these findings, chemotherapy and radiotherapy were advised, but the patient refused.
Leiomyosarcomas can originate throughout the body, but the most common site is the retroperitoneum (20%-67% of cases)[1,2]. Retroperitoneal leiomyosarcomas are more frequent in females and typically affect middle-aged to older adults[3]. Diagnosis is delayed because most retroperitoneal leiomyosarcomas are asymptomatic. The primary tumour masses are typically large, and distant metastases are present at the time of diagnosis in approximately 40% of cases[4]. In our patient, retroperitoneal sarcoma was detected incidentally during a gynaecological operation. Although the mass was 8 cm, the patient had no complaints, and distant metastasis was not evident at the time of the diagnosis.
Surgery was the main treatment. Given that the survival of patients with retroperitoneal sarcomas depends on complete resection of the tumour, extensive surgery is recommended[5,6]. Nevertheless, the prognosis of retroperitoneal sarcoma is poor due to a high incidence of local recurrence and distant metastases[6]. However, the following characteristics are associated with a favourable prognosis: tumours less than 5 cm in diameter, low histological grade tumours, and bladder tumours[7]. Tumours that occur in the retroperitoneum have the worst prognosis. Mitotic activity is the primary prognostic factor; specifically, tumours with 5 mitoses per 10 high-power fields are considered malignant[8]. Accordingly, the retroperitoneal leiomyosarcoma in our patient has poor prognostic factors (8 cm size, low grade, retroperitoneal site). Although the mass in the retroperitoneal region was fully removed and the surgical margins were histologically negative, local recurrence and lung, brain and clitoris metastases were detected approximately 4 years after the patient’s first surgery. The recurrent mass detected in our patient can be explained by micrometastasis or tumour seeding. Furthermore, it has been reported that local invasion may be an important factor for tumour recurrence and distant metastasis[7].
The distant spread of these tumours occurs via the bloodstream principally to the lung, liver, and peritoneal cavity. Metastasis may also be found in the bone, spleen, and soft tissues[2-7]. A clitoris metastasis from retroperitoneal leiomyosarcoma have not been reported previously. The brain is an uncommon metastasis site in prior case reports; metastases from previously reported leiomyosarcomas were generally located in the uterus[9,10]. The diameter of the clitoral metastasis was 2 cm × 1.8 cm and 6-8 mitoses per 10 high-power fields were observed. The tumour was well differentiated and immunoreactive for α-smooth muscle actin and desmin. Histopathological examination of the resected lesion revealed features consistent with leiomyosarcoma; therefore, based on the patient’s past medical history and these histological similarities, the patient was diagnosed as having a clitoris metastasis to the from the retroperitoneal leiomyosarcoma. We discussed a potential mechanism of metastasis to the clitoris and brain in the patient. Soft-tissue sarcomas rarely show lymphatic spread; therefore, we hypothesize that clitoris and brain metastases occurred by the haematogenous route.
Other case reports of tumours that metastasize to the clitoris include breast, bladder, renal and gastric cancers[11-14]. Metastatic leiomyosarcomas are treated with surgery and/or adjuvant chemotherapy, but no standard treatment has been established given the small number of patients[6,15]. Increased survival has been reported in patients undergoing a metastasectomy[15]. Because our case refused the chemotherapy or radiotherapy, we only performed the clitoral mass excision. Despite surgery, the patient died six months after metastasis identification.
Herein, we report the case of a 64-year-old woman who was diagnosed with a clitoral metastasis form a retroperitoneal leiomyosarcoma. In addition lung and brain metastases were detected in the work-up examination. In a known case of leiomyosarcoma, a newly developed clitoral mass should be considered as a metastasis and histologically confirmed. Leiomyosarcomas usually recur within several years from the initial diagnosis. Therefore, patients should be observed and clinicians should be aware of areas of atypical metastasis.
A 64-year-old woman has a painful mass in the clitoris.
A 2 cm polypoid mass with regular margins in the clitoris was revealed upon vaginal examination.
The differential diagnosis of the clitoral mass should be performed from infective organisms, cysts, invasion from cancers in the vicinity and metastasis from distant organs and should be confirmed with biopsy.
The diagnosis of clitoral tumors includes radiological diagnosis, surgical procedures (biopsies) and histo-pathological examination.
The computed tomography of the chest indicated multiple bilateral pulmonary metastases, abdominal magnetic resonance imaging showed a mass lesion on the left psoas muscle, and brain magnetic resonance imaging showed a metastatic mass lesion located in the left temporo-parietal region.
The retroperitoneal and clitoral tumour were composed of spindle-shaped cells with abundant eosinophilic cytoplasm and elongated nuclei and most nuclei were centrally located, blunt-ended and “cigar-shaped” and immunohistochemically, tumor cells were diffusely and strongly positive for smooth muscle actin, caldesmon and vimentin, S-100 protein, epithelial membran antigen, CD117 and CD 34.
Because our case refused the chemotherapy and radiotherapy, the authors only performed clitoral tumour excision.
Leiomyosarcoma usually recurs within several years from the initial diagnosis. Therefore, patients should be subject to such an observation period at least and clinicians should be aware of areas of atypical metastasis.
The authors observed a clitoris metastasis originated from retroperitoneal leiomysarcoma. This is a very interesting case and should be published so that the observation can be shared with colleagues in the field. There are some spelling mistakes in the article.
P- Reviewers: Garfield D, Ke YQ, Yang QF S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | O'Sullivan PJ, Harris AC, Munk PL. Radiological imaging features of non-uterine leiomyosarcoma. Br J Radiol. 2008;81:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Mack TM. Sarcomas and other malignancies of soft tissue, retroperitoneum, peritoneum, pleura, heart, mediastinum, and spleen. Cancer. 1995;75:211-244. [PubMed] |
| 3. | Lal H, Neyaz Z, Kapoor VK, Pottakkat B, Gupta P. Local recurrence and multi-organ metastasis of primary retroperitoneal leiomyosarcoma in unusual locations after surgical resection. J Radiol Case Rep. 2011;5:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Storm FK, Mahvi DM. Diagnosis and management of retroperitoneal soft-tissue sarcoma. Ann Surg. 1991;214:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 150] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Stoeckle E, Coindre JM, Bonvalot S, Kantor G, Terrier P, Bonichon F, Nguyen Bui B. Prognostic factors in retroperitoneal sarcoma: a multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group. Cancer. 2001;92:359-368. [PubMed] |
| 6. | Jaques DP, Coit DG, Hajdu SI, Brennan MF. Management of primary and recurrent soft-tissue sarcoma of the retroperitoneum. Ann Surg. 1990;212:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 213] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Wile AG, Evans HL, Romsdahl MM. Leiomyosarcoma of soft tissue: a clinicopathologic study. Cancer. 1981;48:1022-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Wu YY, Wei Q, Zeng H, Chen HJ, Li H, Lin H, Li X. An unusual case of aldosterone- and norepinephrine-secreting retroperitoneal leiomyosarcoma. Eur Surg Res. 2008;41:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Bindal RK, Sawaya RE, Leavens ME, Taylor SH, Guinee VF. Sarcoma metastatic to the brain: results of surgical treatment. Neurosurgery. 1994;35:185-190; discussion 190-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 71] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Ziyal IM, Musluman M, Bejjani GK, Tanik C, Türkmen CS, Aydin Y. Cerebral metastasis of a uterine leiomyosarcoma--case report. Neurol Med Chir (Tokyo). 1999;39:238-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Julien V, Labadie M, Gauthier G, Ronger-Savle S. Clitoral metastasis from ductal breast cancer revealing metastases in multiple sites and review of the literature. J Low Genit Tract Dis. 2012;16:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Yazgan C, Erden A, Yagci C, Ozden E, Turkolmez K. Clitoral metastasis from transitional cell carcinoma of the renal pelvis: CT and MRI findings. Int Urol Nephrol. 2004;36:331-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Thomas JA, Matanhelia SS, Griffiths D, Matthews PN. Clitoral metastasis secondary to transitional cell carcinoma of the bladder. Br J Urol. 1994;74:524-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Ahmed W, Beasley WH. Carcinoma of stomach with a metastasis in the clitoris. J Pak Med Assoc. 1979;29:62-63. [PubMed] |
| 15. | Alldinger I, Yang Q, Pilarsky C, Saeger HD, Knoefel WT, Peiper M. Retroperitoneal soft tissue sarcomas: prognosis and treatment of primary and recurrent disease in 117 patients. Anticancer Res. 2006;26:1577-1581. [PubMed] |