Published online Aug 24, 2025. doi: 10.5306/wjco.v16.i8.108371
Revised: June 14, 2025
Accepted: July 17, 2025
Published online: August 24, 2025
Processing time: 119 Days and 20.1 Hours
Metachronous multiple esophageal squamous cell carcinomas (ESCCs) may occur in some patients after endoscopic resection. Multiple dysplastic lesions in the esophagus increase risk of multiple squamous cell carcinomas (SCCs). Endoscopic imaging technology such as narrow band imaging (NBI), can detect early SCC. Lugol chromoendoscopy is also the conventional standard technique for detecting superficial ESCC. However, little is known about the interval from the first SCC to the metachronous SCC. Effective methods to prevent multiple metachronous SCCs are needed in survivors of esophageal SCC.
A 56-year-old man showed a slightly elevated reddish area in the middle thoracic esophagus at 30 cm from the incisors on gastroscopy for routine examination. Esophageal mucosa lesion was about 2.5 cm. NBI and magnifying gastroscopy confirmed intra-epithelial papillary loop type B-1 according to the Japan Eso
This is the first case of multiple dysplastic lesions of esophagus cured by radiotherapy. Radiotherapy after minimally invasive endoscopic treatment might be a safe and effective optional therapeutic strategy to prevent metachronous multiple esophageal SCCs.
Core Tip: The grade of Lugol-voiding lesions is associated with risk of metachronous squamous cell carcinomas (SCCs). Effective methods to prevent metachronous multiple SCCs are needed in survivors of esophageal squamous cell carcinomas. We present the first case of multiple dysplastic lesions of esophagus cured by radiotherapy. This case indicated that radiotherapy after endoscopic submucosal dissection might be a safe and effective optional therapeutic strategy to prevent metachronous multiple esophageal SCCs.
- Citation: Chen D, Zhong DF, Liu D. Exploration of preventive treatment for high risk patients with metachronous multiple esophageal squamous cell carcinoma: A case report. World J Clin Oncol 2025; 16(8): 108371
- URL: https://www.wjgnet.com/2218-4333/full/v16/i8/108371.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i8.108371
Squamous dysplasia is believed to be a pre-neoplastic lesion of squamous cell carcinomas (SCCs) and it is easily identified as Lugol-voiding lesions (LVL) on Lugol chromoendoscopy[1,2]. Many patients with esophageal SCC have multiple LVLs in the esophageal mucosa[3,4]. LVL is graded according to the number of LVL per endoscopic view (A = no lesion; B = 1 to 9 Lesions; C ≥ 10 Lesions). Some studies have shown that higher grade of LVL carries a high risk of metachronous multiple esophageal SCCs[5]. Effective methods are needed to prevent metachronous multiple SCCs. Here we present a case of multiple dysplastic lesions of esophagus cured by radiotherapy.
A 56-year-old man complained of right upper abdominal pain for 2 days.
The patient had a history of diabetes.
The patient had no history of hypertension, hepatitis, tuberculosis, and trauma.
The patient had no personal or family history of tumours.
Physical examination was negative.
The blood tests and tumor markers were all within reference ranges.
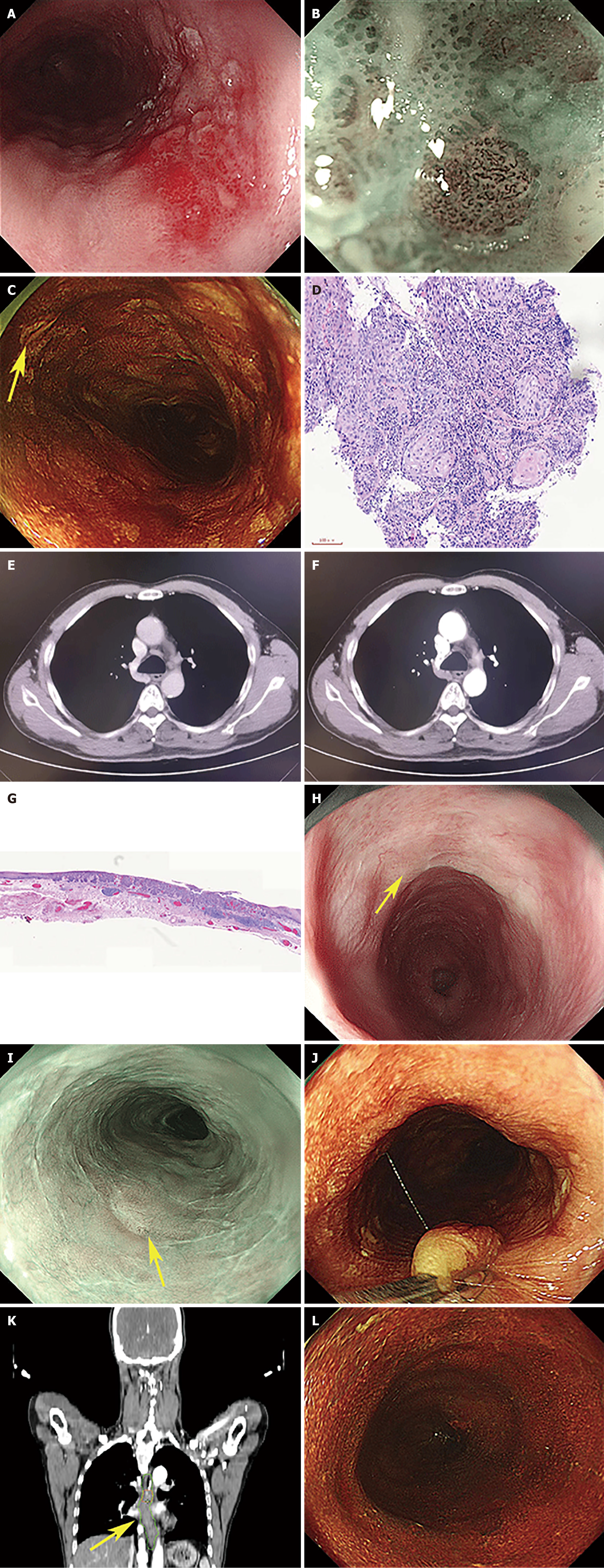
A slightly elevated reddish area in the middle thoracic esophagus at 30 cm from the incisors was revealed by gastroscopy (Figure 1A). Narrow band imaging (NBI) and magnification gastroscopy showed intra-epithelial papillary loop type B-1 (Figure 1B). According to the grade of LVL, more than 10 Lesions per endoscopic view are defined as Grade C (Figure 1C). Biopsy pathology revealed severe dysplastic squamous epithelium (Figure 1D). Computed tomography showed no lymph node metastasis (Figure 1E and F).
Prophylactic radiotherapy can reduce the occurrence of multiple metachronous esophageal cancer.
Endoscopic resection was performed with consent of the patient. Mucosal lesion was completely resected by endoscopic submucosal dissection (ESD). Postoperative pathological results showed moderately differentiated squamous carcinoma, about 1.4 cm × 0.7 cm in size, infiltrated to the muscularis mucosae (Figure 1G). No cancer thrombus was seen in the vasculature, and the surrounding cut edge was not involved.
Patient underwent radiotherapy within 2 months after ESD. We examined patient using Lugol chromoendoscopy to evaluate the dysplastic squamous epithelium of the esophagus before radiotherapy, and found multiple LVLs at 29 cm-40 cm, post-ESD scar at 30 cm-35 cm from the incisors (Figure 1H and I). Titanium clips were used for marking oral and anal sides in multiple LVL ranges (Figure 1J).
Intensity-modulated radiation therapy was delivered by a Varian Synergy linear accelerator (Varian VitalBeam American) with a 6MV X-ray beam. The clinical target volume (CTV) included one tumor bed (CTV1) and multiple LVL (CTV2) (Figure 1K). The planning target volume (PTV) was an additional extension of the caudal and cephalad margin of CTV by 0.3 cm. Standard initial radiation dose of 5040c Gy/28F and 4140cGy/23F were planned for PTV1 and PTV2. The radiation field did not include regional lymph nodes because the probability of metastasis is low in T1a esophageal SCCs (ESCCs). The radiation strategy was designed by an independent radiologist.
Three months after the end of radiotherapy, the multiple LVLs disappeared, evaluated using Lugol chromoendoscopy (Figure 1L). The patient underwent another gastroscopy 8 months after the end of radiotherapy. The multiple LVLs disappeared, and enhanced chest CT did not reveal lymph node metastasis.
The 8.5-year follow-up data of 21111 residents from high-incidence areas for ESCC in China, including Linzhou in Henan Province, Cixian in Hebei Province, and Feicheng in Shandong Province, revealed that the cumulative incidence rates of ESCC were 15.5%, 4.5%, and 1.4% among patients with severe dysplasia/carcinoma in situ, moderate dysplasia, and mild dysplasia, respectively[6]. In patients with early esophageal SCC, organs can be preserved by endoscopic curative treatment, but the preserved organs are strongly affected by squamous dysplastic lesion. Prospective study by Katada et al[5], showed the association between the grade of LVL and risk of metachronous SCC. Higher grade of LVL carried a high risk of metachronous multiple esophageal SCC. However, little research has been done to reduce the grade of LVL. Therefore, effective methods to prevent metachronous multiple SCCs are needed in survivors of esophageal SCC. A cohort study analyzed 330 patients newly diagnosed with superficial ESCC. Patients who ceased or reduced their drinking habit significantly showed improvement in the grade of LVL[1]. In the past, we could only choose endoscopy for reexamination to detect early esophageal SCC as early as possible. In the screening of high-risk populations for esophageal squamous cell carcinoma, we usually choose NBI and Lugol chromoendoscopy. In the background of LVLs, the influence of some inflammatory lesions increases the difficulty of detecting early esophageal squamous cell carcinoma[7,8]. Therefore, the incidence of multiple synchronous esophageal carcinoma remains high during the follow-up process.
ESD is considered the optimal technique for resecting superficial esophageal lesions; however, its high operational complexity and lengthy learning curve pose significant barriers to widespread adoption. Additionally, the potential complication of post-ESD esophageal stenosis remains a critical issue that must be addressed[9,10]. Radiotherapy induces damage to the DNA of abnormally proliferating cells via ionizing radiation, thereby promoting apoptosis or inhibiting mitosis, particularly in rapidly dividing precancerous cells. The presence of multiple dysplastic lesions in the esophagus is associated with an increased risk of ESCC. Radiotherapy can target abnormally proliferating esophageal cells, preventing their progression to SCC. This mechanism parallels the application of radiotherapy in cervical intraepithelial neoplasia[11], where DNA destruction and inhibition of clonal cell survival eliminate residual proliferative epithelial tissue.
We present the first case of multiple dysplastic lesions of esophagus cured by radiotherapy. After the end of radiotherapy, the multiple LVLs disappeared. This case indicated that radiotherapy after ESD might be a safe and effective optional therapeutic strategy to prevent metachronous multiple esophageal SCC. Radiotherapy primarily accomplishes its therapeutic objective by inducing irreparable damage to the DNA of tumor cells via radiation, ultimately resulting in cell death. However, it may also inflict damage on normal cells, potentially leading to adverse effects such as radiation esophagitis, radiation pneumonitis, radiation-induced cardiac injury, and bone marrow suppression. It is imperative to highlight that the treatment effectiveness may have limitations in individual cases. To further substantiate the safety and efficacy of the therapeutic effect, additional randomized controlled trials with a larger sample size are warranted.
The grade of LVL is associated with risk of metachronous multiple esophageal SCCs. Effective methods to prevent metachronous multiple SCC are needed in survivors of esophageal SCC. Radiotherapy after ESD may represent a promising strategy. Further studies are needed to validate its safety and efficacy.
The authors sincerely thank the presented patient for his willingness to participate in this study.
| 1. | Hori K, Katada C, Okada H, Katagiri A, Matsuo Y, Yokoyama T, Yano T, Suzuki H, Shimizu Y, Furue Y, Nakanishi H, Koike T, Takizawa K, Hirao M, Yoshii T, Yamanouchi T, Kawakubo H, Kobayashi N, Shimoda T, Ochiai A, Ishikawa H, Yokoyama A, Muto M. Association between continuous cessation or reduction of drinking alcohol and improvement of multiple dysplastic lesions in patients with esophageal squamous cell carcinoma after endoscopic resection. Esophagus. 2024;21:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Katada C, Yokoyama T, Yano T, Suzuki H, Furue Y, Yamamoto K, Doyama H, Koike T, Tamaoki M, Kawata N, Hirao M, Kawahara Y, Ogata T, Katagiri A, Yamanouchi T, Kiyokawa H, Kawakubo H, Konno M, Yokoyama A, Ohashi S, Kondo Y, Kishimoto Y, Kano K, Mure K, Hayashi R, Ishikawa H, Yokoyama A, Muto M. Alcohol consumption, multiple Lugol-voiding lesions, and field cancerization. DEN Open. 2024;4:e261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Hori K, Okada H, Kawahara Y, Takenaka R, Shimizu S, Ohno Y, Onoda T, Sirakawa Y, Naomoto Y, Yamamoto K. Lugol-voiding lesions are an important risk factor for a second primary squamous cell carcinoma in patients with esosphageal cancer or head and neck cancer. Am J Gastroenterol. 2011;106:858-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Tajiri A, Ishihara R, Sakurai H, Nakamura T, Tani Y, Inoue T, Matsueda K, Miyake M, Waki K, Fukuda H, Shichijo S, Maekawa A, Kanesaka T, Yamamoto S, Takeuchi Y, Higashino K, Uedo N, Michida T, Matsunaga T. Clinical features of superficial esophagus squamous cell carcinoma according to alcohol-degrading enzyme ADH1B and ALDH2 genotypes. J Gastroenterol. 2022;57:630-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Katada C, Yokoyama T, Yano T, Kaneko K, Oda I, Shimizu Y, Doyama H, Koike T, Takizawa K, Hirao M, Okada H, Yoshii T, Konishi K, Yamanouchi T, Tsuda T, Omori T, Kobayashi N, Shimoda T, Ochiai A, Amanuma Y, Ohashi S, Matsuda T, Ishikawa H, Yokoyama A, Muto M. Alcohol Consumption and Multiple Dysplastic Lesions Increase Risk of Squamous Cell Carcinoma in the Esophagus, Head, and Neck. Gastroenterology. 2016;151:860-869.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 148] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 6. | Wei WQ, Hao CQ, Guan CT, Song GH, Wang M, Zhao DL, Li BY, Bai WL, Hou PY, Wang JW, Jin GL, Lei FH, Li XQ, Xue LY, Wang GQ, Abnet CC, Taylor PR, Dawsey SM, Qiao YL. Esophageal Histological Precursor Lesions and Subsequent 8.5-Year Cancer Risk in a Population-Based Prospective Study in China. Am J Gastroenterol. 2020;115:1036-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 7. | Ono S, Dobashi A, Furuhashi H, Koizumi A, Matsui H, Hara Y, Sumiyama K. Characteristics of superficial esophageal squamous cell carcinomas undetectable with narrow-band imaging endoscopy. Gastroenterol Rep (Oxf). 2021;9:402-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 8. | Gruner M, Denis A, Masliah C, Amil M, Metivier-Cesbron E, Luet D, Kaasis M, Coron E, Le Rhun M, Lecleire S, Antonietti M, Legoux JL, Lefrou L, Renkes P, Tarreirias AL, Balian P, Rey P, Prost B, Cellier C, Rahmi G, Samaha E, Fratte S, Guerrier B, Landel V, Touzet S, Ponchon T, Pioche M. Narrow-band imaging versus Lugol chromoendoscopy for esophageal squamous cell cancer screening in normal endoscopic practice: randomized controlled trial. Endoscopy. 2021;53:674-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 9. | Mizuno J, Urabe Y, Oka S, Konishi H, Ishibashi K, Fukuhara M, Tanaka H, Tsuboi A, Yamashita K, Hiyama Y, Kotachi T, Takigawa H, Yuge R, Hiyama T, Tanaka S. Predictive factors for esophageal stenosis in patients receiving prophylactic steroid therapy after endoscopic submucosal dissection for esophageal squamous cell carcinoma. BMC Gastroenterol. 2024;24:41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Kadota T, Yoda Y, Hori K, Shinmura K, Oono Y, Ikematsu H, Yano T. Prophylactic steroid administration against strictures is not enough for mucosal defects involving the entire circumference of the esophageal lumen after esophageal endoscopic submucosal dissection (ESD). Esophagus. 2020;17:440-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Kim YB, Kim YT, Cho NH, Koom WS, Kim S, Kim SW, Nam EJ, Kim GE. High-dose-rate intracavitary radiotherapy in the management of cervical intraepithelial neoplasia 3 and carcinoma in situ presenting with poor histologic factors after undergoing excisional procedures. Int J Radiat Oncol Biol Phys. 2012;84:e19-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |